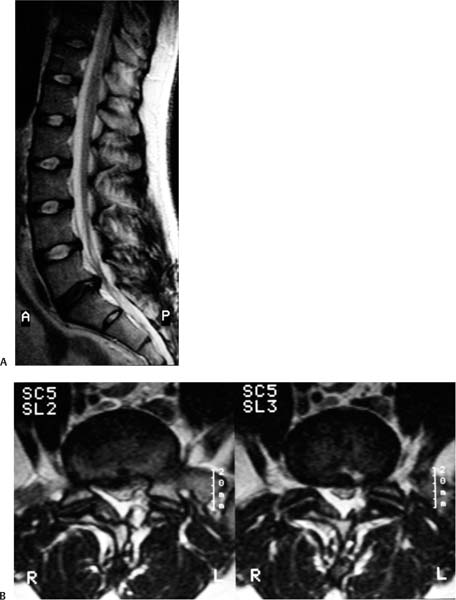
10 In 2001 the Swedish Lumbar Spine Study Group confirmed that lumbar spine arthrodesis was superior to conservative management of debilitating low back pain.1 In addition to alleviating mechanical low back pain and radicular pain, restoration of normal lumbar lordosis and overall sagittal balance is crucial in ensuring lasting pain relief and improved quality of life. To this end, interbody fusion techniques have been used with increasing frequency and offer several advantages over traditional posterior spinal fusion techniques. The increased surface area for fusion and ability to place the graft material under compressive forces should help facilitate fusion. In addition, the ability to reestablish normal disk space height allows for indirect decompression of foraminal stenosis. The concept of spinal fusion was first introduced in the early 1900s by Albee and Hibbs.2,3 They described posterior spinal fusion for management of spinal deformity associated with Pott disease. The first description of an interbody fusion was by Capener and colleagues in the 1930s.4 This was an anterior lumbar interbody fusion (ALIF) via a transabdominal approach for treatment of spondylolisthesis. Years later, in 1953, Cloward described the posterior lumbar interbody fusion (PLIF), allowing for an interbody fusion through a true midline posterior approach.5 Harms and colleagues later introduced the transforaminal lumbar interbody fusion, with the goal of accomplishing an interbody fusion as in the PLIF but through a unilateral postero-lateral approach, obviating the need for significant retraction of the neural elements and hence decreasing the potential for neural injury.6 The eXtreme Lateral Interbody Fusion (XLIF, NuVasive, Inc., San Diego, CA), described by Pimenta in 2001, is a true lateral approach through the retroperitoneal space to the spine.7 XLIF offers many of the same advantages of ALIF while decreasing some of the inherent risks of an anterior approach to the spine. Pimenta also introduced the axial lumbar interbody fusion (AxiaLIF, TranS1, Wilmington, NC), an approach that utilizes the presacral space as an access corridor to the L5–S1 interspace.8 This evolution in spinal fusion has been driven by a desire to minimize morbidity and collateral damage to the surrounding anatomical structures of the spine. The indications for lumbar interbody fusion have expanded since they were first described for the management of spondylolisthesis. Patients with recurrent lumbar disk herniations, postlaminectomy syndrome, and those with axial back pain secondary to degenerative disk disease are now routinely managed with interbody fusion. Patients at high risk for pseudarthrosis or those undergoing reoperations for pseudarthrosis are often also best managed with interbody fusion.9 This chapter reviews the minimally invasive interbody fusion techniques, highlights their advantages, and discusses their indications. The chapter is summarized in the form of a decision-making algorithm designed to help surgeons select the appropriate minimally invasive interbody fusion technique for various clinical scenarios. The transforaminal lumbar interbody fusion (TLIF) is a common procedure performed for the management of a variety of pathologies requiring lumbar arthrodesis. Through a unilateral approach (preferably the side with radicular symptoms) a hemilaminectomy and facetectomy are performed, providing access to the interbody space. A complete diskectomy and end plate preparation are performed, followed by insertion of an interbody graft, which achieves anterior column support. Pedicle screws are inserted and the construct is compressed to facilitate fusion across the interbody graft and reestablish lumbar lordosis. The minimally invasive variation on the TLIF procedure (MI-TLIF) was first described in 2003 by Foley et al and has since become an increasingly popular method of lumbar arthrodesis, offering the advantages of an open TLIF through a smaller exposure.10,11 As opposed to the open approach, the MI-TLIF is performed through a unilateral paramedian incision. Tubular dilators are utilized to minimize injury to the paraspinal musculature. Contralateral percutaneous pedicle screws may be inserted to achieve distraction. Bony decompression, diskectomy, end plate preparation, and interbody graft insertion are achieved through a muscle splitting approach. Ipsilateral pedicle screws are inserted and the construct compressed as in the open approach.10 The minimally invasive TLIF has several important advantages over the open technique. A paramedian approach with removal of the pars interarticularis and total facetectomy allow for a complete decompression of the ipsilateral neural structures and avoid undue retraction of the thecal sac during placement of the bone graft. Furthermore, the structural integrity of the midline osteoligamentous structures is maintained, and the placement of contralateral percutaneous instrumentation minimizes tissue disruption, particularly the facet capsules. The side of the approach should always be ipsilateral to the patient’s radicular symptoms. In cases of severe canal stenosis, decompressive laminectomy can be performed, the spinous process undercut, and the contralateral lamina drilled to achieve bilateral decompression of the spinal canal. In cases of severe bilateral foraminal stenosis, a minimally invasive decompression can be performed through a separate contralateral incision using tubular retractors through which pedicle screws can also be placed. Revision surgery is not made more complicated by a minimally invasive approach. In fact, a paramedian/MI approach for revision surgery is advantageous because it avoids traversing scar tissue, which is unavoidable with exposure through a traditional midline incision. There are certain disadvantages to the TLIF and its MI counterpart. One important limitation is the difficulty involved in placing a large interbody graft when needed to reestablish normal disk space height and lordosis. It is also difficult to ensure that the graft rests anterior to the instantaneous axis of rotation. Sufficient anterior placement of the graft is crucial in reestablishing normal lumbar lordosis following compression of the dorsal fusion construct. A contraindication to this procedure is the presence of a conjoined nerve root within the foramen.11 Although this is an exceedingly rare occurrence, it is one for which there should be a thorough evaluation on preoperative imaging. Attempts to retract the neural elements of conjoined roots for graft placement carry a significant risk of neurological injury.11 If this is appreciated preoperatively, a contralateral TLIF or alternative approach should be considered. Although the MI-TLIF with percutaneous pedicle screws is a relatively new approach, there is early evidence supporting its effectiveness. Lowe et al published a series of 40 patients who underwent minimally invasive TLIF and were followed for an average of 36 months.12 Patients in this series had a confirmed fusion rate of 90%, a significant reduction in pain, and improvement in the Oswestry Disability Index. Schwender et al evaluated the effectiveness of this technique in a series of 49 patients with a minimum of 18 months follow-up.13 In this series, all patients had solid fusion based on radiographic criteria at last follow-up. Patients also had significant improvements in average visual analog pain scale and Oswestry Disability Index. Jang and Lee had similar results in their series of 23 patients who underwent an MI-TLIF with ipsilateral pedicle screw and contralateral facet screw stabilization.14 The indications for a minimally invasive TLIF mirror those for an open TLIF and include degenerative disk disease, grade 1–2 spondylolisthesis associated with mechanical back pain or radicular pain, and recurrent disk herniations with or without mechanical back pain. It is a particularly ideal technique in patients with back pain with unilateral radiculopathy from severe foraminal stenosis or recurrent disk herniations with significant lumbar stenosis (Fig. 10.1). The eXtreme Lateral Interbody Fusion (XLIF) technique was first described by Pimenta in 2001 as a modification of the traditional retroperitoneal approach to the lumbar spine.15 This approach shares many of the advantages of the traditional retroperitoneal exposure in that it provides direct visualization of the disk space and vertebral body, allows for the insertion of a large interbody spacer, and can provide indirect decompression of central and foraminal stenosis. Further, it eliminates many of the disadvantages of an open anterior approach, including the potential need for an access surgeon, risk of vascular or sympathetic nerve injury, and anterior longitudinal ligament disruption. As a result of the transpsoas tubular dilation, there is a risk of injury to the nerve roots of the lumbosacral plexus, particularly at L4–5. However, this is mitigated through the use of real-time intraoperative neural monitoring systems. The XLIF technique is limited to interspaces above the iliac crest and is not applicable to L5–S1 or L4–5 in some cases. Fig. 10.1 A 36-year-old man presented with longstanding back pain and left leg pain with a history of previous L5–S1 diskectomy. (A) Preoperative sagittal and (B) axial magnetic resonance images showed degenerative disk disease at the L5–S1 level with left foraminal stenosis. The patient failed to improve with conservative management and underwent a left-sided L5–S1 minimally invasive transforaminal lumbar interbody fusion with percutaneous screw stabilization.Postoperative AP (C) and lateral x-rays (D) demonstrating placement of the interbody spacer and instrumentation. The patient had significant relief of his back and left leg pain following surgery.
Minimally Invasive Lumbar Interbody Fusion: Choosing Between Approaches
Operative Techniques
Minimally Invasive Transforaminal Lumbar Interbody Fusion with Percutaneous Pedicle Screw Stabilization
Minimally Invasive Lateral Interbody Fusion with Percutaneous Pedicle Screw Stabilization

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree