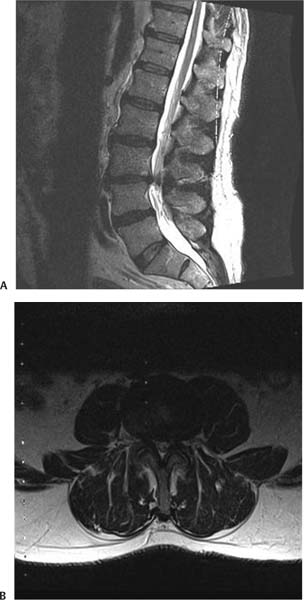
6 Lumbar spinal stenosis is defined as any condition that leads to narrowing of the spinal canal and exiting nerve roots. It can be divided into six categories, as defined by Arnoldi et al and modified by Katz and Harris.1,2 These include congenital stenosis, acquired stenosis, iatrogenic stenosis, spondylotic stenosis, and posttraumatic stenosis. Most frequently, stenosis is caused by a constellation of factors that are associated with lumbar degenerative disease. Anterior to the neural canal, the degenerating lumbar disks continue to desiccate and lose their elasticity. This then leads to loss of lumbar disk height and a broad “bulging” of the disk contents into the neural canal, and laterally into the lateral recess and neural foramen. Lateral to the central neural canal, chronic stress and strain on the lumbar facets lead to hypertrophy of these joints and often the formation of osteophytes and degenerative cysts. These enlarged, overgrown facets also contribute to pressure on the exiting nerve roots and diminish the entire cross-sectional area of the lumbar canal. Degenerative changes also lead to the hypertrophy of the ligamentum flavum in the dorsal aspect of the spinal canal. Furthermore, as the overall disk height collapses anteriorly, the ligamentum flavum begins to buckle and impinge upon the neural canal as well. When the patient extends the spine, the posterior elements are compressed, exacerbating the buckling of the ligamentum flavum and leading to worsening of the clinical symptoms. Patients with congenital stenosis will often present before the age of 65, usually in their 30s to 40s. These patients are born with congenitally shortened pedicles leading to a narrowed cross-sectional area of the lumbar canal from birth. Degenerative changes in the lumbar disk and facets are not tolerated well and lead to early presentation of neurological symptoms. Iatrogenic stenosis can be the result of laminectomy or lumbar fusion. There is evidence that in a small percentage of the population, fusion of the lumbar motion segments will lead to accelerated degenerative changes at the levels above and below the fusion.3 The ideal candidate for surgery of lumbar stenosis is the elderly patient with classic symptoms of lumbar claudication who has failed a thorough trial of nonsurgical therapy. These patients complain of back and bilateral buttock pain that has severely limited their ability to walk. This pain can often radiate into the thighs and legs in various dermatomal distributions. Pain in the bilateral buttock region that is exacerbated with standing or walking and gradually relieved by sitting is classical neurogenic claudication. The pain can be initiated by the transition from a sitting to a standing position, but often it begins after a short period of standing or ambulating. The pain is often described as worsened with extension of the spine and mildly relieved by flexion of the spine. This “shopping cart” sign, where patients will describe symptomatic relief while walking in a flexed position with the aid of a walker or shopping cart, is helpful in identifying patients with lumbar stenosis. A detailed history can help differentiate neurogenic claudication from vascular claudication. In vascular claudication, patients do not generally describe significant pain with standing. They often describe pain that is initiated with walking, especially uphill, that is immediately relieved by rest. Patients with vascular claudication will also reproduce their pain with exercise on a bicycle, whereas patients with lumbar stenosis will often not be able to reproduce their back pain in the flexed bicycle riding position. To confirm the diagnosis, all patients with these complaints should have antero-posterior (AP), lateral, flexion, and extension x-rays of their lumbar spine. These films quickly identify the extent of degenerative changes in the lumbar spine, the overall sagittal and coronal balance, the degree of disk height loss, end plate sclerosis, and facet hypertrophy. Furthermore, these radiographs can rule out the presence of spondylolisthesis and the presence of any abnormal motion between the lumbar levels. The presence or absence of motion can be a key component in the treatment algorithm for lumbar stenosis. The next radiographic test that is ordered is magnetic resonance imaging (MRI) or computed tomographic (CT) myelography in patients who are unable to undergo MRI. Although the CT-myelogram gives a better understanding of the bony anatomy and a clearer view of facet hypertrophy, it is an invasive procedure with an associated risk of complications. MRI will give a clear view of the soft tissue anatomy, including the degree of degenerative changes in the lumbar disks and ligamentum flavum. There is often a complete loss of T2 cerebrospinal fluid (CSF) signal at the level of the most severe lumbar stenosis (Fig. 6.1A,B). The classic appearance of a “trefoil”-shaped lumbar canal can also be appreciated on axial T2 MRI sequences. This trefoil shape is the result of compromise of the cross-sectional area by the degenerated, bulging lumbar disks anteriorly, the hypertrophic facets laterally, and the buckling enlarged ligamentum flavum posteriorly. The MRI can also reveal the presence of degenerative facet cysts, “synovial cysts,” that can further lead to canal narrowing. MRI scans can be highly sensitive in identifying the cardinal radiographic signs of lumbar stenosis. It is important to clearly correlate the findings on the history and physical with the radiographic results. In one study performed on asymptomatic patients, the presence of lumbar stenosis identified on MRI was as high as 20%.4 Fig. 6.1 (A) Sagittal and (B) axial T2-weighted magnetic resonance imaging showing lumbar stenosis at L3–4 ideally suited for a minimally invasive approach. Recent prospective, randomized, multicentered studies have demonstrated a significantly better outcome for the surgical treatment of lumbar stenosis over non-surgical treatment.5 The classic surgical treatment of lumbar stenosis is an open posterior decompressive lumbar laminectomy. This is performed via a midline incision over the affected lumbar levels. The midline lumbodorsal fascia is incised the length of the skin incision, and periosteal dissection is used to strip the erector spinae musculature off the posterior spinal elements. These denervated muscles are retracted laterally throughout the procedure. The supraspinous ligament and interspinal ligaments are then resected with the spinous processes. The bilateral lamina, medial facet joint complexes, and ligamentum flavum are then removed. Upon adequate visualization of the decompressed lumbar canal and exiting nerve roots, hemostasis is achieved and the wound is closed. The stripped paraspinal musculature is reapproximated with loose sutures. The thoracodorsal fascia is closed watertight, followed by closure of the subdermal layer. There are many studies that have shown the effectiveness of this operation to treat lumbar stenosis.6,7 However, the disadvantages of this procedure were also clearly evident to many observers. The first major disadvantage of the open technique is the muscle injury that results from the dissection, denervation, and retraction. The second major disadvantage is the destabilization that results from the disruption of the supraspinal and interspinal ligaments. The third disadvantage is the potential destabilization that occurs with significant bilateral medial facetectomies that are often performed. Finally, the frequency of medical complications in the elderly population during the recovery time required for the open procedure can also pose a problem. There have been several steps in the evolution of less invasive treatment of lumbar stenosis. An open procedure with bilateral laminoforaminotomies was first advocated to preserve the posterior tension band.8 This was followed by the recommendation for a less invasive unilateral open laminoforaminotomy to achieve a bilateral decompression while preserving the contralateral musculature.9 This approach involves a midline incision, unilateral subperiosteal exposure, ipsilateral laminotomy and medial facetectomy, and contralateral decompression by undercutting the lamina from within the spinal canal with the use of the operating microscope. The operating table can be tilted away from the surgeon to provide greater visualization for performing the contralateral decompression. This technique preserves the posterior tension band, contralateral facet joints, and contralateral musculature. In a retrospective review of 374 patients with spinal stenosis treated with unilateral laminotomy and bilateral microdecompression, Costa et al found 87.9% of patients experienced a significant benefit with a very low complication rate.10 No patient went on to require a fusion procedure for iatrogenic instability. Two major technological advancements pioneered modern minimally invasive spinal surgery. First, the introduction of the tubular retraction system allowed for an effective muscle-sparing access to the spine. Second, the advancement in microscopic and endoscopic technology allowed for a safe, illuminated, and magnified view of the pathological conditions that could now be treated. In 2002, a novel minimally invasive laminectomy was presented and quickly validated in clinical series. The microendoscopic decompression of stenosis (MEDS) offers an alternative to the classic open laminectomy. The MEDS accomplishes the same goals as the open laminectomy procedure, the decompression of the lumbar canal and exiting nerve roots, without the major drawbacks of an open procedure. The surgical techniques are described in detail.
Minimally Invasive Lumbar Laminectomy for Stenosis
Preoperative Evaluation
Open Decompressive Laminectomy
Unilateral Laminotomy for Bilateral Decompression
Minimally Invasive Decompression
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree