Mood Disorders
Mood is defined as a pervasive and sustained feeling that is experienced internally and that, in the extreme, can markedly influence all aspects of a person’s behavior and his or her perception of the world. Affect is the external expression of mood. Mood disorders, formally known as affective disorders, include a group of psychological disorders that are mainly characterized by pathological moods and related vegetative and psychomotor disturbances. The term mood disorder is preferred over affective disorder because it refers not only to the external (affective) expression of the present emotional state but also to sustained emotional states. Mood disorders are syndromes (not diseases) that consist of signs and symptoms that present a deviation from a person’s normal functioning and are sustained over a period of weeks to months. These signs and symptoms tend to recur, often in periodic or cyclical fashion.
The most common mood disorder is major depressive disorder (unipolar depression). Major depressive disorder is characterized by one or more episodes of major depression without a manic episode. Patients with both manic and depressive episodes or with manic episodes alone are diagnosed with bipolar disorder. Dysthymia and cyclothymia are less severe forms of major depression and bipolar disorder, respectively. Hypomania is an episode of manic symptoms but does not meet the criteria for a manic episode.
Mood disorders can sometimes be difficult to diagnose, given the subjective nature of the symptoms. All people have normal periods of feeling either blue or elated, and most of these obviously are not diagnosable as disorders. A mood disorder is characterized by the intensity, duration, and severity of the symptoms. Symptoms interfere with normal thought process and content and cognitive, speech, and social functioning. Unfortunately, many people with depressive disorders go untreated because their symptoms are minimized or misinterpreted. People with bipolar disorders are more often treated because their symptoms more frequently are bizarre or disruptive enough to bring them to medical and psychiatric attention.
Mood disorders are caused by a complex interplay of biological and psychological factors. Biologic theories involve the role of the biogenic amines, particularly dysfunction in the norepinephrine, serotonin, dopamine, and GABA (γ-aminobutyric acid) neurotransmitter systems. Most antidepressant medications involve complex manipulations of these systems. There appears to be dysregulation as well in the adrenal, thyroid, and growth hormone axes, all of which have been implicated in the etiology of mood disorders. Abnormalities in the sleep cycle and in regulation of circadian rhythms have also been studied.
Genetics always play an important role in the etiology of mental disorders, but genetic input is especially relevant in mood disorders. Bipolar I disorder is one of the most genetically determined disorders in psychiatry. However, as with any mental disorder, psychosocial factors play a crucial role in the development, presentation, course, and prognosis of mood disorders. Issues of real and symbolic loss, family relationships and dynamics, environmental stress, and unconscious conflicts all strongly contribute to and determine mood symptoms. Some clinicians believe that these factors are particularly important in the first episodes of mood disorders, but in one form or another, they play a role in all episodes.
Students should study the questions and answers below for a useful review of these disorders.
Helpful Hints
Students should know the following terms that relate to mood disorders.
adrenal axis
anxiety-blissfulness psychosis
atypical features
biogenic amines
bipolar I disorder
bipolar II disorder
carbamazepine
cognitive, behavioral, family, and psychoanalytic therapies
cognitive theories
cyclothymic disorder
depression rating scales
depressive equivalent
double depression
dysthymia
ECT
euthymic
folieà double forme
folie circulaire
GABA
GH
5-HT
hypomania
kindling
learned helplessness
LH, FSH
lithium
major depressive disorder
mania
MAOIs
melancholic features
melatonin
mild depressive disorder
mixed episode
mood-congruent and -incongruent psychotic fear
neurological, medical, and pharmacological causes of mood disorders
norepinephrine
phototherapy
postpartum onset
premenstrual dysphoric disorder
premorbid factors
pseudodementia
rapid cycling
REM latency, density
RFLP
seasonal pattern
SSRI
suicide
T3
thymoleptics
TSH, TRH
vegetative functions
Zeitgeber
Questions
Directions
Each of the questions or incomplete statements below is followed by five suggested responses or completions. Select the one that is best in each case.
15.1 Mild, nonpsychotic depression with predominant anxiety is called
A. Endogenomorphic depression
B. Bipolar disorder
C. Chronic depression
D. Dysthymia
E. Anxiety disorder
View Answer
15.1 The answer is D
Dysthymia is defined as a reactive nonpsychotic depression of mild to moderate intensity with predominant anxiety. It is characterized by the presence of a depressed mood that lasts most of the day and is present almost continuously. Patients complain that they have always been depressed. It is not a sequela to a major depressive episode as with chronic depression. There are associated feelings of inadequacy, guilt, irritability, and anger; withdrawal from society; loss of interest; and inactivity and lack of productivity. Most cases are of early onset, beginning in childhood or adolescence and certainly by the time patients reach their 20s. The overall prognosis for dysthymia is good with treatment; however, 25 percent of dysthymic patients never attain complete recovery.
Bipolar disorder is defined as a mood disorder in which the patient exhibits both manic and depressive episodes. The criteria for a manic episode require the presence of a distinct period of abnormal mood lasting at least 1 week. Typically beginning in the teenage years, the 20s, or the 30s, the first episode of bipolar I disorder could be manic, depressive, or mixed. On average, manic episodes predominate in youth, and depressive episodes predominate in later years. Although the overall sex ratio is 1:1, men, on average, undergo more manic episodes, and women experience more mixed and depressive episodes.
Endogenomorphic depression is a term used to describe inhibition of the pleasure or reward system to such an extent that the patient no longer has the capacity for enjoyment. There may or may not be an apparent environmental precipitant or stress. In most cases, patients show dramatic abnormalities in psychomotor activity and somatic rhythms (i.e., sleep, appetite, libido). Such patients may also be delusional. The symptom profile in chronic depression usually displays low-grade intensity. Full criteria for a major depressive episode must have been met continuously for at least the past 2 years. Instead of the customary remission within 1 year, patients are ill for years.
Anxiety disorders are disorders in which anxiety is the most prominent disturbance or in which patients experience anxiety if they resist giving in to their symptoms. They are among the most prevalent mental disorders in the general population. Women are affected nearly twice as frequently as men. They are associated with significant morbidity and often are chronic and resistant to treatment. They include (1) panic disorder with or without agoraphobia, (2) agoraphobia with or without panic disorder, (3) specific phobia, (4) social phobia, (5) obsessive-compulsive disorder (OCD), (6) posttraumatic stress disorder (PTSD), (7) acute stress disorder, and (8) generalized anxiety disorder.
15.2 The most consistent computer tomography (CT) and magnetic resonance imaging (MRI) abnormality observed in depressive disorders is
A. cortical atrophy
B. sulcal widening
C. ventricular enlargement
D. increased frequency of hyperintensities in subcortical regions
E. none of the above
View Answer
15.2 The answer is D
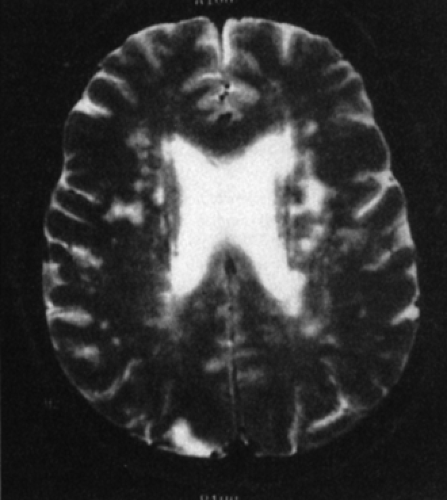
Computed tomography (CT) and magnetic resonance imaging (MRI) scans provide sensitive, noninvasive methods to assess the brain, including cortical and subcortical tracts, as well as white matter lesions. The most consistent abnormality observed in the depressive disorders is increased frequency of abnormal hyperintensities in subcortical regions, especially the periventricular area, basal ganglia, and thalamus (Figure 15.2). More common in bipolar I disorder and among the elderly, these hyperintensities appear to reflect the deleterious neurodegenerative effects of recurrent mood episodes. Ventricular enlargement, cortical atrophy, and sulcal widening have also been reported in patients with mood disorders compared with normal control subjects. In addition to age and illness duration, structural abnormalities are associated with increased illness severity, bipolar status, and increased cortisol levels. Some depressed patients also may have reduced caudate nucleus volumes, suggesting a defect in the mesocorticolimbic system. Cerebrovascular factors often involve subcortical frontal and basal ganglia structures and appear particularly relevant to late-life depression.
15.3 The following situations call for a break in doctor–patient confidentiality except
A. A patient with a delusional disorder thinks his boss is out to get him and threatens to kill her.
B. A patient with major depressive disorder who is sexually promiscuous contracts syphilis.
C. A patient with bipolar I disorder admits he is homosexual.
D. A patient with conduct disorder thrives on the sexual abuse of young children.
E. A patient with schizoaffective disorder hallucinates that he can fly.
View Answer
15.3 The answer is C
Confidentiality refers to the therapist’s responsibility to not release information learned in the course of treatment to third parties. Confidentiality is an essential ingredient of psychiatric care because it is a prerequisite for patients to be willing to speak freely to therapists. People would be less likely to go for help and would tend to withhold crucial information if confidentiality was not assured. There is no reason to break doctor–patient confidentiality in situations involving a patient’s sexual preference (e.g., homosexuality) unless there is some threat to the patient’s safety. Confidentiality must give way to the responsibility to protect others when a patient makes a credible threat to harm someone (e.g, a patient threatening to kill his boss) or acts in a way that could harm him- or herself (e.g., a patient who thinks he can fly). Reportable diseases (e.g., syphilis) must also be reported to the proper authorities despite the bond of patient confidentiality. Any suspicion of child abuse must also be reported to the authorities.
15.4 A 27-year-old patient has been diagnosed with bipolar disorder. Before starting this patient on lithium for mood stabilization, which of the following laboratory tests should be obtained?
A. Thyroid function tests, creatinine, pregnancy test
B. Thyroid function tests, creatinine, liver function tests
C. Thyroid function tests, creatinine, complete blood count
D. Thyroid function tests, liver function tests, pregnancy test
E. Thyroid function tests, complete blood count, pregnancy test
View Answer
15.4 The answer is A
Lithium (Eskalith), used for mood stabilization in patients with bipolar disorder, is known for its low margin of safety, making frequent monitoring necessary. Common side effects include gastrointestinal disturbances, nephrotoxicity, hypothyroidism, tremors, leukocytosis, acne, psoriasis flares, hair loss, and edema. Because of these effects, it is important to get thyroid function tests and renal function tests (creatinine) before starting any patient on this medication. Lithium is also teratogenic and has been associated with cardiac defects, so a pregnancy test is necessary before lithium therapy.
15.5 Which of the following statements regarding mood disorders is false?
A. One of four patients with an acute depressive episode will have recurrences throughout life.
B. Approximately 15 percent of depressed patients eventually commit suicide.
C. Incidence of depression in younger age groups is increasing.
D. Manic forms of mood disorders predominate in men.
E. Depressive disorders are more common in women.
View Answer
15.5 The answer is A
Three (not one) out of four patients with acute depression will experience recurrences, with varying degrees of residual symptoms between episodes. Of note, although depressive disorders are more common in women, more men than women die of suicide because of more lethal methods chosen.
15.6 All of the following are vegetative disturbances of depression except
A. Hypersexuality
B. Anorexia
C. Hypersomnia
D. Insomnia
E. Circadian dysregulation
View Answer
15.6 The answer is A
Hypersexuality is cardinal sign of mania and usually indicates a mixed episode of bipolar disorder in depressed patients. The small subgroup of depressed persons with increased sexual drive usually exhibit other atypical features; hence, increased sexual drive is considered the fifth reverse vegetative sign (after even worsening mood, initial insomnia, hypersomnia, and weight gain).
The biological concomitants of melancholia include profound reductions in appetite (i.e., anorexia or weight loss), sleep (i.e., insomnia), and sexual functioning, as well as alterations in other circadian rhythms, especially worsening of mood and psychomotor performance. An equally prominent subgroup of depressed persons exhibits a reversal of the vegetative and circadian functions, with increases in appetite and sleep—and sometimes in sexual functioning—and an evening worsening of mood; in this atypical pattern, patients characteristically exhibit mood reactivity and sensitivity to rejection.
15.7 Serotonin
A. helps to regulate circadian rhythms
B. is an important regulator of sleep, appetite, and libido
C. stores are increased by transient stress and depleted by chronic stress
D. permits or facilitates goal-directed motor and consummatory behavior in conjunction with norepinephrine and dopamine
E. all of the above
View Answer
15.7 The answer is E (all)
Serotoninergic neurons project from the brainstem dorsal raphe nuclei to the cerebral cortex, hypothalamus, thalamus, basal ganglia, septum, and hippocampus. Serotonin (5-HT) pathways have both inhibitory and facilitatory functions in the brain. For example, much evidence suggests that 5-HT is an important regulator of sleep, appetite, and libido. Serotonergic neurons projecting to the suprachiasmatic nucleus of the hypothalamus help to regulate circadian rhythms (e.g., sleep–wake cycles, body temperature, and hypothalamic-pituitary-adrenocortical axis function). Serotonin also permits or facilitates goal-directed motor and consummatory behaviors in conjunction with norepinephrine and dopamine. Moreover, serotonin inhibits aggressive behavior across mammalian and reptilian species.
There is some evidence that serotonin neurotransmission is partly under genetic control. Nevertheless, whereas acute stress increases serotonin release transiently, chronic stress eventually depletes serotonin stores. Chronic stress may also increase synthesis of 5-HT1A autoreceptors in the dorsal raphe nucleus, which further decrease serotonin transmission. Elevated glucocorticoid levels tend to enhance serotonergic functioning and thus may have significant compensatory effects on chronic stress.
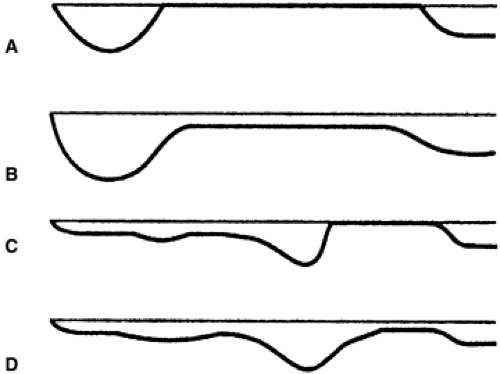
15.8 Which graph in Figure 15.1 depicts the pattern with the best future prognosis?
A. A
B. B
C. C
D. D
E. None of the above
View Answer
15.8 The answer is A
The course of major depressive disorder, recurrent, with no antecedent dysthymic disorder and a period of full remission between the episodes predicts the best future prognosis. This is depicted in graph A.
15.9 Which of the graphs in Figure 15.1 depicts the prototypical course of double depression?
A. A
B. B
C. C
D. D
E. None of the above
View Answer
15.9 The answer is D
Graph D depicts double depression, which is characterized by recurrent major depressive disorder and antecedent dysthymic disorder with no period of full remission in between the two most recent episodes. Graph A is the course of major depressive disorder, recurrent, with no antecedent dysthymic disorder and full remission between episodes. Graph B is the course of major depressive disorder, recurrent, with no antecedent dysthymic disorder but with prominent symptoms persisting between episodes (partial remission is attained). Graph C is the rare pattern major depressive disorder, recurrent, with antecedent dysthymic disorder but with full interepisodic recovery.
15.10 Double depression is characterized by
A. two family members with major depressive disorder concurrently
B. recurrent major depressive disorder with current symptoms twice as disabling as usual
C. two episodes of major depressive disorder per month consistently
D. superimposed bipolar II disorder and atypical depression
E. recurrent major depressive disorder superimposed with dysthymic disorder
View Answer
15.10 The answer is E
Double depression is characterized by recurrent major depressive disorder with antecedent dysthymic disorder and no period of full remission between the two most recent episodes. This pattern is seen in approximately 20 to 25 percent of the persons with major depressive disorder.
15.11 Depression and mania share which of the following symptoms?
A. Psychomotor acceleration
B. Low-self esteem
C. Grandiosity
D. Anger
E. Pessimism
View Answer
15.11 The answer is D
Despite their contrasts, depression and mania share such symptoms as irritability, anger, insomnia, and agitation. Mania is defined as a mood disorder characterized by elation, agitation, hyperactivity, and hyperexcitability. The clinical features of mania are generally the opposite of those of depression. Depression is defined as a mental state characterized by feelings of sadness, loneliness, despair, low self-esteem, and self-reproach. Depression is commonly associated with cases of lowered mood, thinking, self-esteem, and activity. Mania, on the other hand, is commonly associated with elevated mood, a rush of ideas, psychomotor acceleration, and grandiosity. An excess of the shared symptoms of escalating intensity suggests a mixed phase of mixed episode of mania and depression occurring simultaneously, commonly called bipolar I disorder.
15.12 The person least likely to develop major depressive disorder in his or her lifetime is
A. a 60-year-old man with pancreatic cancer
B. a 19-year-old woman who was raped 3 weeks ago
C. a 12-year-old girl mourning the death of her mother
D. a 10-year-old boy diagnosed with dysthymia
E. an identical twin of a patient with major depressive disorder who committed suicide
View Answer
15.12 The answer is B
The 19-year-old rape victim is more likely to develop a variation of posttraumatic stress disorder, which is highest among victims of rape, military combat veterans, and survivors of torture. Childhood onset of dysthymia similarly presages extremely high rates of depression and bipolar disorder in adulthood. Monozygotic twins have been shown to have a two- to fourfold increase in concordance rates for mood disorders over dizygotic twins, compelling data for the role of genetic factors in mood disorders.
Parental loss before adolescence is also a well-documented risk factor for adult-onset depression. Medical problems of many types, such as cancer of the pancreas, multiple sclerosis, and space-occupying lesions of the brain, can produce depression.
15.13 A hypomanic episode differs from a manic episode in that a hypomanic episode
A. lasts at least 1 week
B. lacks psychotic features
C. is severe
D. causes greater social impairment
E. all of the above
View Answer
15.13 The answer is B
A hypomanic episode lacks psychotic features, which can sometimes be associated with mania. A manic episode is a distinct period of an abnormally and persistent elevated, expansive, or irritable mood lasting for at least 1 week or less if a patient must be hospitalized. A hypomanic episode lasts at least 4 days and is similar to a manic episode except that it is not sufficiently severe to cause impairment in social or occupational functioning. Patients often believe that they benefit from the energy and confidence of hypomania. Diagnostically, history of hypomania is preferably obtained from significant others who have observed the patient; the experience is often pleasant, and the subject may be unaware of it or may tend to deny it. Both mania and hypomania are associated with inflated self-esteem, decreased need for sleep, distractibility, great physical and mental activity, and overinvolvement in pleasurable behavior.
15.14 The defense mechanism most commonly used in depression is
A. undoing
B. sublimation
C. projection
D. introjection
E. altruism
View Answer
15.14 The answer is D
In Sigmund Freud’s structural theory, introjection of the lost object into the ego leads to the typical depressive symptoms of a lack of energy available to the ego. The superego, which is unable to retaliate against the lost object externally, flails out at the psychic representation of the lost object, now internalized in the ego as an introject. When the ego overcomes or merges with the superego, energy previously bound in the depressive symptoms is released, and mania supervenes with the typical symptoms of excess.
Projection is the unconscious defense mechanism in which a person attributes to another person those generally unconscious ideas, thoughts, feelings, and impulses that are personally undesirable or unacceptable. Sublimation is an unconscious defense mechanism in which the energy associated with unacceptable impulses or drives is diverted into personally and socially acceptable channels.
Undoing is an unconscious defense mechanism by which a person symbolically acts out to reverse something unacceptable that has already been done or against which the ego must defend itself. Altruism is regard for and dedication to the welfare of others.