Mood stabilisers and ECT
Mood stabilisers
The discovery that lithium reduces the risk of both manic and depressive relapse in bipolar affective disorder has resulted in it being viewed as a mood stabilising drug. Some anticonvulsants, such as valproate salts and carbamazepine, have similar effects and have also come to be thought of as ‘mood stabilisers’. In some ways, this is an unhelpful term. It wrongly implies that drugs such as lithium will help in other conditions in which there is instability of mood, such as emotionally unstable personality disorder. It does not take account of the fact that lithium is widely used to augment antidepressants in cases of treatment resistant unipolar depression. There is the additional issue of what to call the atypical antipsychotic drugs, such as quetiapine, that are effective in both the depressive and manic phases of bipolar disorder. It is probably more helpful to remember the indications for individual drugs (e.g. Table 1 on p. 51), rather than categorise them in a potentially misleading way, and we have only used the term ‘mood stabilisers’ as a heading for this chapter because it is conventional to do so.
Lithium
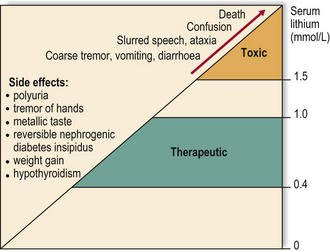
Lithium is a naturally occurring ion and a member of group one of the periodic table, the alkali metals. Compared with other drugs, the ratio of toxic to therapeutic levels is low, so lithium can only be used safely if blood levels are monitored. At therapeutic levels, lithium has a number of benign side effects, as shown in Figure 1. It can cause nephrogenic diabetes insipidus early in treatment, which is reversible at first but can become permanent if lithium is not stopped soon enough. Chronic kidney disease is an uncommon but important long-term effect of treatment with lithium – the cases that do occur are usually in people who have taken the drug for 20–30 years. Hypothyroidism affects about 10% of people who take lithium, usually after several years of treatment and more frequently in people with other risk factors for hypothyroidism, such as female gender and family history. Hyperparathyroidism and hypercalcaemia can also occur. Lithium toxicity is usually associated with levels of 1.5 mmol/L or more. People taking lithium should be advised to stop the drug if they develop a coarse tremor, vomiting or diarrhoea, and to drink plenty of fluid and seek medical advice. Toxicity can be precipitated by dehydration, for example during hot weather, and prescription of drugs that increase lithium levels, such as NSAIDs and thiazide diuretics. Some people will develop abnormalities of cardiac conduction after starting lithium. The monitoring required during lithium treatment is summarised in Table 1.
Table 1 Monitoring of people taking lithium
| Test | When? | Why? |
|---|---|---|
| Lithium level | < div class='tao-gold-member'> Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|