SECTION V MULTIFOCAL NEUROLOGICAL DISEASE AND ITS MANAGEMENT
BACTERIAL INFECTIONS – MENINGITIS
ACUTE BACTERIAL MENINGITIS
Causative organisms
| In neonates | |
| Haemophilus influenzae. | |
| In children | |
| Meningococcus. (Neisseria meningitidis). | |
| In adults |
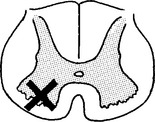
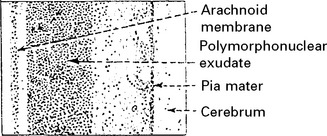
Pathology
A purulent exudate most evident in the basal cisterns extends throughout the subarachnoid space.
The underlying brain, although not invaded by bacteria, becomes congested, oedematous and ischaemic.
The integrity of the pia mater normally protects against brain abscess formation.
Clinical
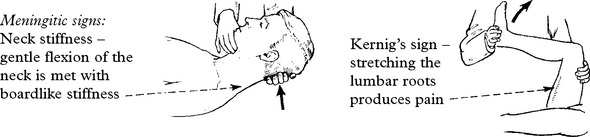
The classical clinical triad is fever, headache and neck stiffness.
| Prodromal features (variable) | Meningitic symptoms |
|---|---|
| A respiratory infection otitis media or pneumonia associated with muscle pain | Severe frontal/occipital headache |
| Stiff neck | |
| Photophobia. |
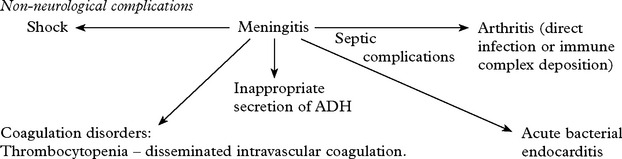
Systemic signs: – High fever. Transient purpuric or petechial skin rash in meningococcal meningitis.
Non-neurological complications
Features specific to causative bacteria
| Haemophilus meningitis | Meningococcal meningitis | Pneumococcal meningitis |
|---|---|---|
| Often occurs in epidemics where the organism is carried in the nasopharynx. Septicaemia can occur with arthralgia; purpuric skin rash. When overwhelming, confluent haemorrhages appear in the skin due to disseminated intravascular coagulation. | ||
| Outcome | ||
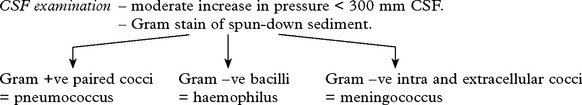
Investigations
Treatment
Initial therapy (before organism identification)
| Neonates (above 1 month) | |
| Children (under 5 years) | |
| Adults | |
| Immunocompromised patient |
Therapy after organism identification
| ORGANISM | ANTIBIOTIC | ALTERNATIVE THERAPY |
|---|---|---|
| Haemophilus | Ampicillin or 3rd generation cephalosporin according to sensitivities | |
| Pneumococcus | Benzylpenicillin or 3rd generation cephalosporin according to sensitivities | |
| Meningococcus | Benzylpenicillin or 3rd generation cephalosporin according to sensitivities | |
| E. coli | 3rd generation cephalosporin | Aztreonam, fluoroquinolone, meropenem, ampicillin |
| Listeria |
BACTERIAL INFECTIONS – CNS TUBERCULOSIS
MENINGITIS
In adults, it may occur many years after the primary infection.
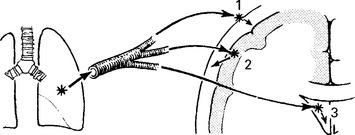
Following bacteraemia, metastatic foci of infection lodge in:
The clinical features of tuberculous meningitis (TBM) result from:
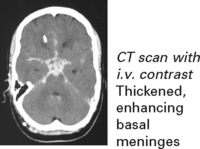
The basal meninges are generally most severely affected.
Clinical features
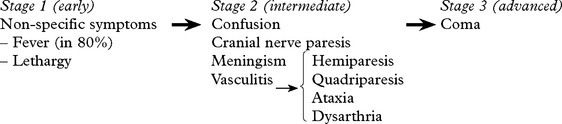
Staging is useful for predicting outcome.
Seizures may occur at the onset. Involuntary movements (chorea, myoclonus) occur in 10%.
Untreated, the illness may progress from phase 1 to death over a 3-week period.
Arachnoiditis inflammatory exudate may result in hydrocephalus/dementia/blindness.
TUBERCULOUS MENINGITIS
Investigations
Diagnosis
Diagnosis is based on the clinical presentation with characteristic CSF findings.
DIFFERENTIAL DIAGNOSIS – Viral meningoencephalitis – Subacute/chronic meningitis (see pages 517–8).
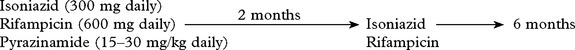
Treatment
If suspect, commence antituberculous treatment.
Recommended treatment programme:
Drug resistance suspected due to previous antituberculous therapy, e.g.
→ Add a fourth drug – streptomycin (1 g daily) or ethambutal (25 mg/kg daily).
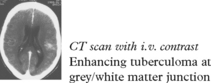
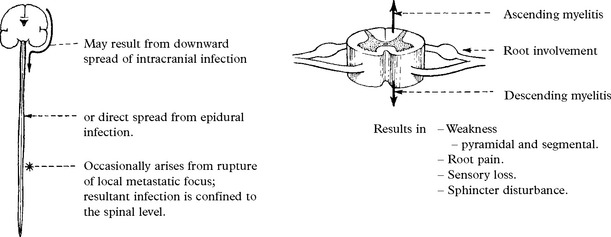
OTHER FORMS OF CNS TUBERCULOUS INFECTION
SPIROCHAETAL INFECTIONS OF THE NERVOUS SYSTEM
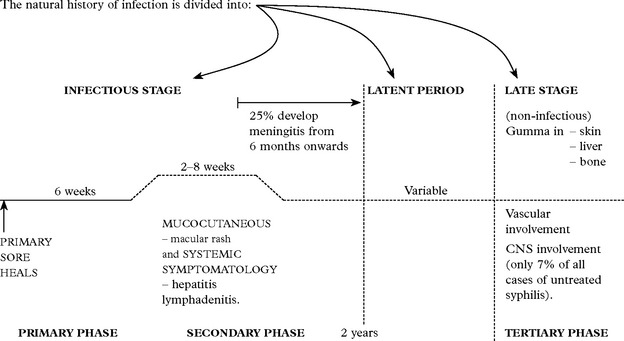
SYPHILIS
This infectious disease is caused by the spirochaete Treponema pallidum. Entry is by:
Not all patients untreated in the secondary phase progress to the tertiary phase.
In HIV patients the neurological complications occur earlier and advance more quickly.
Investigations
Serological diagnosis depends on detection of antibodies.
SPIROCHAETAL INFECTION – NEUROSYPHILIS
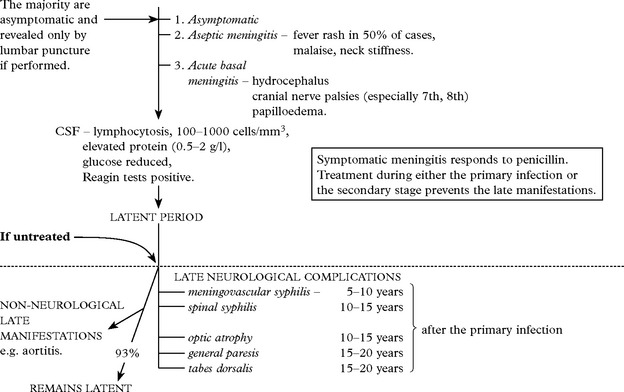
ACUTE SYPHILITIC MENINGITIS: Three clinical forms are recognised:
Late neurological complications occur in only 7% of untreated cases.
MENINGOVASCULAR SYPHILIS
‘Early’ late manifestation resulting in an obliterative endarteritis and periarteritis.
OCULAR MANIFESTATIONS
Meningitis around optic nerve with subpial necrosis may be the only manifestation of late syphilis.
Presents as a constriction of the visual fields with a progressive pallor of the optic disc:
Neuroretinitis, uveitis and chorioretinitis occur, especially in HIV patients.
GENERAL PARESIS
Argyll Robertson pupils may be present (see page 146).
CSF – lymphocytes 50/mm3, protein ↑ 0.5–2 g/l, gammaglobulin ↑.
Reagin tests in CSF positive in the majority.
Treatment in the preparalytic phase will halt progression in 40%.
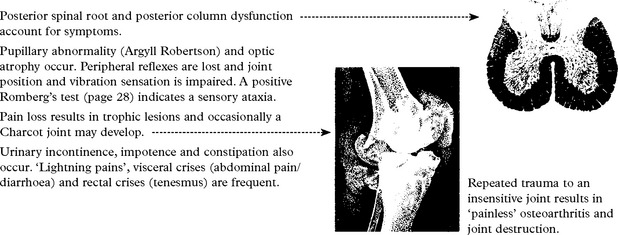
TABES DORSALIS
Posterior spinal root and posterior column dysfunction account for symptoms.
SYPHILITIC GUMMA presenting as an intracranial mass is extremely rare.
TREATMENT OF NEUROSYPHILIS
| Penicillin G. | 2–4 megaunits i.v. | (When patient sensitive to penicillin |
| or | 4-hourly for 10 days. | ↓ |
| Procaine Penicillin | 600 000 units i.m. daily for 15 days. | erythromycin or tetracycline may be given orally over 30 days.) |
| Benzathine Penicillin | 2–4 megaunits i.m. weekly × 3. |
CSF follow up: CSF is checked initially and at 6 monthly intervals until normal.
Cell count and degree of positivity of VDRL are the best indicators of persistent infection.
SPIROCHAETAL INFECTION
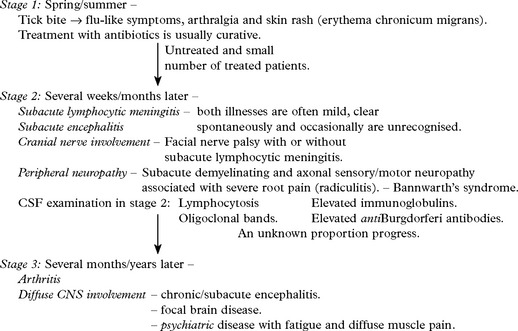
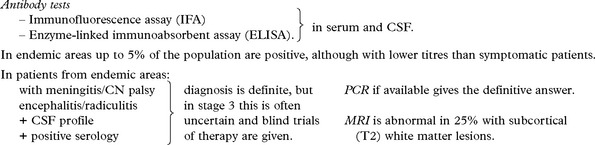
LYME DISEASE (NEUROBORRELIOSIS)
Treatment
Stage 1 – Oral antibiotics: penicillin, erythromycin or tetracycline.
Stage 2 – I.V. penicillin G. 20 million units for 10 days (or ceftriaxone).
If symptoms persist – wrong diagnosis with misleading titres, or – immune mediated damage.
Steroids can be used in late stages when symptoms have not responded to antibiotics.
PARASITIC INFECTIONS OF THE NERVOUS SYSTEM – PROTOZOA
TOXOPLASMOSIS
A world-wide parasitic infection affecting many species, including man.
Organism: An anaerobic intracellular protozoan, Toxoplasma gondii.
There are two forms of toxoplasmosis:
Organisms are seldom identified.
Serological tests may be negative in AIDS.
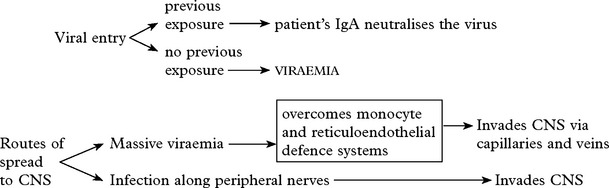
VIRAL INFECTIONS
MENINGITIS
| Common causal viruses – | Rare causal viruses – |
| ENTEROVIRUSES | LYMPHOCYTIC CHORIOMENINGITIS |
| MUMPS VIRUS | HUMAN IMMUNODEFICIENCY VIRUS (HIV) |
| HERPES SIMPLEX (subtype 2) | WEST NILE VIRUS |
| EPSTEIN-BARR VIRUS (EBV) |
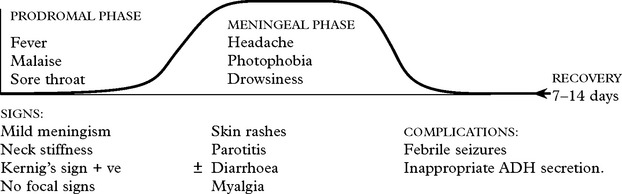
VIRAL INFECTIONS – MENINGITIS
Clinical features of acute aseptic meningitis
Spread is by the faecal/oral route.
Mumps – affects children/young adults. Winter/spring incidence.
Human Immunodeficiency Virus (HIV) – suspect in high risk groups (page 515). HIV antibodies are often absent and develop 1–3 months later during convalescence.
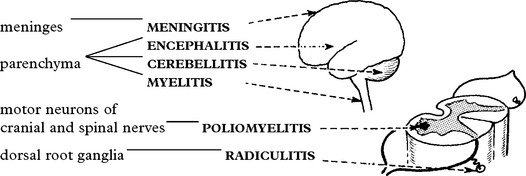
VIRAL INFECTIONS – PARENCHYMAL
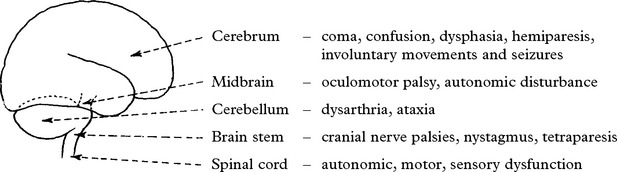
ACUTE VIRAL ENCEPHALITIS
Viral infection causes neuronal and glial damage with associated inflammation and oedema.
Viral encephalitis is a worldwide disorder with the highest incidence in the tropics.
| Rare forms in specific areas: | ||
General: pyrexia, myalgia, etc.
Specific to causative virus, e.g. features of infectious mononucleosis (Epstein-Barr).
Meningeal involvement (slight) → neck stiffness, cellular response in CSF.
Signs and symptoms of parenchymal involvement – focal and/or diffuse.
In general, the illness lasts for some weeks.
Prognosis is uncertain and depends on the causal virus as do neurological sequelae.
Herpes Simplex (HSV) and Varicella-Zoster (VZV) commonly cause disease in humans.
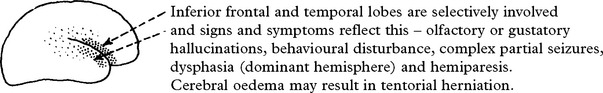
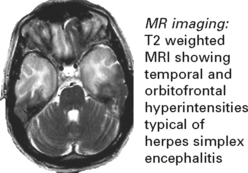
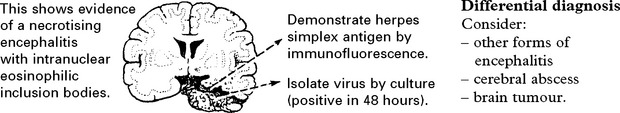
HERPES SIMPLEX ENCEPHALITIS
HSV-1 is the commonest cause of sporadic encephalitis.
One third occur due to primary infection; two thirds have pre-existing antibodies (reactivation).
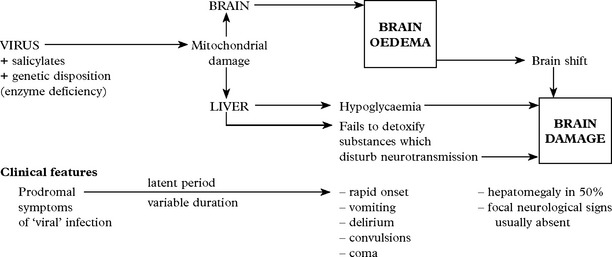
VIRAL INFECTIONS – REYE’S SYNDROME
REYE’S SYNDROME
Pathogenesis
Viral synergism with an environmental factor, e.g. salicylates, may be responsible.
Morphological changes in mitochondria indicate a central role.
Differential diagnosis
Consider other causes of raised intracranial pressure in childhood, especially
Treatment
Treatment aims at lowering intracranial pressure with the aid of intracranial pressure monitoring (see page 52). In addition, blood glucose must be maintained and any associated coagulopathy treated. Reduction of ammonia may be achieved by peritoneal dialysis or exchange transfusion.
VIRAL INFECTIONS – CHRONIC DISORDERS
In these disorders the infection results in a chronic progressive neurological condition.
The evidence of a viral etiology is:
Direct – finding of inclusion bodies, demonstration of viral particles or isolation of virus.
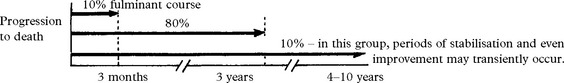
SUBACUTE SCLEROSING PANENCEPHALITIS (SSPE)
Caused by measles-like paramyxovirus – isolated from brain biopsy.
Less common with the availability of widespread primary measles vaccination.
Stage 1: Behavioural problem, declining school performance, progression → dementia
Stage 2: Chorioretinitis, myoclonic jerks, seizures, ataxia, dystonia
Stage 3: Lapses into rigid comatose state
Accompanying features of infection, i.e. pyrexia, leucocytosis, are absent.
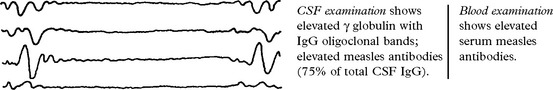
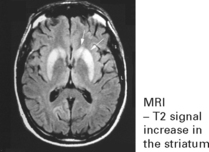
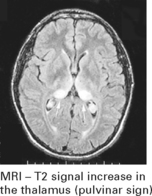
Investigations
EEG – shows periodic high voltage slow wave complexes on a low voltage background trace.
PROGRESSIVE RUBELLA PANENCEPHALITIS
Similar to SSPE with a fatal outcome, caused by rubella virus.
| Presents at a later age (10–15 years) | CSF shows high γ globulin. |
| Progressive dementia. | Antibodies elevated in serum and CSF to rubella. |
| Ataxia. Spasticity. Myoclonus. | Biopsy does not show inclusion bodies. |
| Treatment: No effective treatment |
PRION DISEASES
Investigation
EEG – 1–2 Hz triphasic sharp waves with periodic complexes
CSF – increase in protein 14–3–3 (a protein kinase inhibitor)
[The combined EEG and CSF findings, where positive, have diagnostic sensitivity/specificity of 97%]
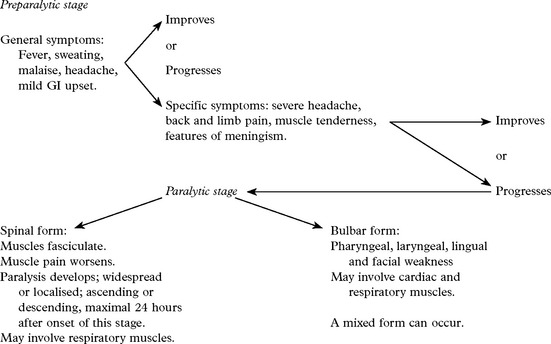
VIRAL INFECTIONS – MYELITIS AND POLIOMYELITIS
POLIOMYELITIS
The poliovirus is a picornavirus (RNA virus).
Epidemiology
A highly communicable disease which may result in epidemics.
Seasonal incidence – late summer/autumn.
World-wide distribution, although more frequent in northern temperate climates.
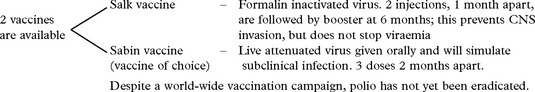
VIRAL INFECTIONS – POLIOMYELITIS
Treatment
The patient is kept on bed rest and fluid balance carefully maintained.
Respiratory failure may require ventilation.
Avoid the development of deformities in affected limbs with physiotherapy and splinting.
VIRAL INFECTIONS – VARICELLA-ZOSTER INFECTION
| Conditions caused: | < div class='tao-gold-member'> Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|

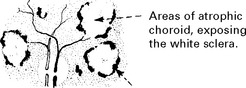 Retinal pigment epithelium becomes hyperplastic – densely pigmented areas result.
Retinal pigment epithelium becomes hyperplastic – densely pigmented areas result.