3 | Multilevel Cervical Spondylosis: Anterior Approach |
 | Case Presentation |
History and Physical Examination
A.W. is a 69-year-old housewife who presented to the spine clinic with neck pain and right arm pain that had lasted for 6 months. She had no prior injuries to her neck. She walked without assist devices but stated that her balance had become worse over the last few months. She had no trouble with her hand function. She denied bowel and bladder problems. On physical exam, she had a normal gait but had difficulty maintaining her balance on one leg. Her Romberg test was positive. Range of motion of the cervical spine was 40 degrees in all directions with some pain. Neurological exam showed no weakness and no sensory loss to pinprick stimulation, and deep tendon reflexes were 3+ in her upper and lower extremities. She had two jogs of clonus on the right. Hoffmann sign was positive. Babinski sign was negative.
Radiological Findings
Anteroposterior and lateral radiographs of the cervical spine (Figs. 3–1, 3–2) showed advanced cervical spondylosis with congenital stenosis and pronounced disk space collapse at C5-6 and C6-7. Anterior and posterior osteophytes were present. Some cervical lordosis was present. Sagittal magnetic resonance image (Fig. 3–3) showed a central disk protrusion at C3-4 that was effacing the spinal cord. Ossification of the posterior longitudinal ligament (OPLL) was present central and to the right at C5-6 and C6-7, which was significantly compressing the spinal cord and take-off of the nerve roots.
Diagnosis
Cervical spondylosis with myeloradiculopathy, OPLL C5-6 and C6-7
 | Background |
Cervical spondylosis is the natural result of aging. Disk degeneration with collapse and osteophyte formation are the hallmarks of this process. This may occur at one motion segment but frequently involves more than one level of the subaxial cervical spine. Cervical spondylosis is a common phenomenon. Friedenberg and Miller1 reported that degenerative changes of the cervical spine are seen on radiographs in 25% of people by the age of 50 and 75% of people by the age of 70. Fenlin2 later reinforced this by showing that 70% of asymptomatic people over the age of 70 years have degenerative changes of the cervical spine. Radiculopathy develops when the disk space collapses leading to foraminal stenosis and nerve root compression. Myelopathy develops when there is cervical stenosis and the spinal cord is compressed by degenerative structures such as disk and osteophyte complex, the in-folding ligamentum flavum, and the posterior longitudinal ligament.3–5 Myelopathy is a progressive disorder that follows a predictable path leading to quadriparesis and death over many years. Clarke and Robinson6 first described the progressive nature of myelopathy associated with cervical spondylosis in 1956. Nurick developed a scale to grade myelopathy that is based on ambulation and activities of daily living.7,8 This was later modified by Zeidman and Ducker to include hand function.9 When patients present with hyperreflexia and hand or gait disturbances, operative intervention is usually recommended. The goals of surgery are to remove the compressive structures that impair nerve root and spinal cord function and to stabilize the decompressed motion segments. Both anterior cervical diskectomy and fusion (ACDF) and anterior cervical corpectomy and fusion (ACF) provide good clinical results with improvement in pain and motor function for patients with radiculopathy and myelopathy.4,10,11 Cervical corpectomy and fusion has a lower pseudarthrosis rate than multilevel interbody grafting.12,13 However, anterior cervical plates have increased fusion rates for multilevel ACDF.14,15 Allograft bone has been used for anterior cervical fusion with good results in patients with single-level16,17 and multilevel18 ACDF, but the incidence of pseudarthrosis is higher. Allograft strut is not routinely used in the setting of cervical corpectomy because of the extended length of time required for complete incorporation, which can be as long as 1 year. Reconstruction of the cervical spine with titanium mesh cages and local autograft following corpectomy has been described in the literature.19–21 Multiple complications and a longer time to fusion have prevented the widespread use of titanium cages.22,23

Figure 3–1 Lateral radiograph of the cervical spine that shows multilevel spondylosis with severe degenerative changes seen at C5-6 and C6-7.

Figure 3–2 Anteroposterior radiograph of the cervical spine.

Figure 3–3 Sagittal T2-weighted magnetic resonance image of the cervical spine that shows spinal cord compression at C5-6 and multiple degenerative disks. Ossification of the posterior longitudinal ligament is present at C5-6 and C6-7.
 | Authors’ Preferred Method of Surgical Management |
Anterior cervical corpectomy and fusion with autograft bone strut, either iliac crest or fibula, is our preferred method of treatment for multilevel cervical spondylosis with radiculopathy or myelopathy. An anterior cervical plate is added if the patient is at risk for developing a pseudarthrosis or extrusion of the graft. During surgery, the patient is positioned supine on the operating room table. A hip bump (for iliac crest graft) and a scapula roll are placed under the patient. Electrodes are placed on the scalp, neck, and extremities to monitor cortical evoked potentials. The head is held in place using the Mayfield headrest (Integra, Plainsboro, NJ). Cervical traction (15 lb) is applied using Gardner-Wells tongs. It is important to pull down the shoulders with tape to elongate the neck. Avoid excessive traction on the shoulders, which may cause a brachial plexus neuropathy. Depending on the length of graft needed to stabilize the cervical spine, either the ipsilateral iliac crest (one- to one-and-a-half-level corpectomy) or the ipsilateral fibula (two or more levels) is prepped and draped. If the fibula is harvested, a tourniquet is applied to the thigh prior to draping. The bed is placed in reverse Trendelenburg to help with blood loss and bring the operative field closer to the surgeon. The cervical spine is approached from the left as described by Southwick and Robinson.24 It is important to incise the superficial layer of the deep cervical fascia, the fascia of the sternocleidomastoid muscle, and the pretracheal fascia both proximally and distally to gain adequate exposure of the spine (Fig. 3–4). The omohyoid may be incised as well to aid with exposure. The cervical level is localized with a spinal needle and intraoperative radiograph. The graft site is then exposed. After confirmation of the level, the diskectomies are completed at all involved levels. Make sure the anterior osteophytes are removed with a rongeur or 5 mm burr early to facilitate exposure of the posterior aspect of the disk space. The corpectomy is complete by removing the anterior central two thirds of the vertebral body with a 5 mm burr. Visualize the uncovertebral joints and stay medial to them to prevent injury to the vertebral artery. It is safe to burr down to the posterior longitudinal ligament (PLL) with the diamond-tipped burr. A small, angled curette is used to remove osteophytes from the foramen and edges of the vertebral body. The posterior cortex of the vertebral body is lifted off the PLL using a small curette as well. The PLL is intentionally preserved to protect the dura and spinal cord. In 30 years of using this technique, we have not had a postoperative neural deficit secondary to spinal cord manipulation.
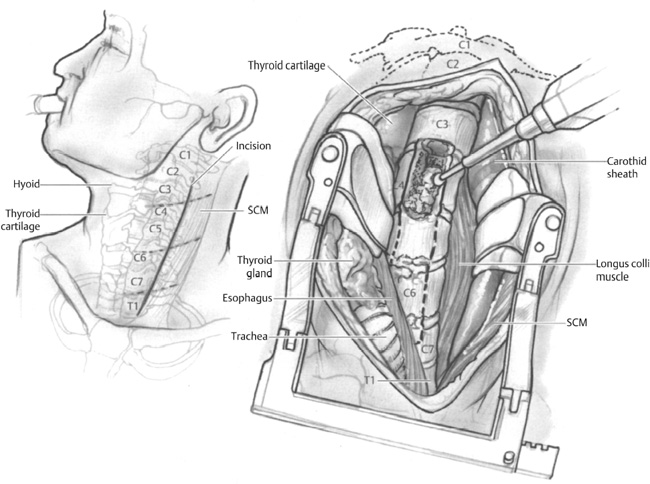
Figure 3–4 The surgical approach involves an anterior, transverse incision with dissection between the carotid sheath and the trachea and esophagus. Please also see Fig. 1–5 in chapter 1.



