Multiple Brain Hyperintensities (T2/FLAIR), Less Common
Gary M. Nesbit, MD
DIFFERENTIAL DIAGNOSIS
Less Common
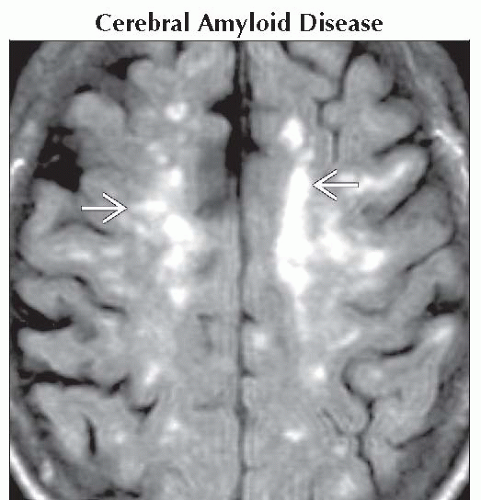
Cerebral Amyloid Disease
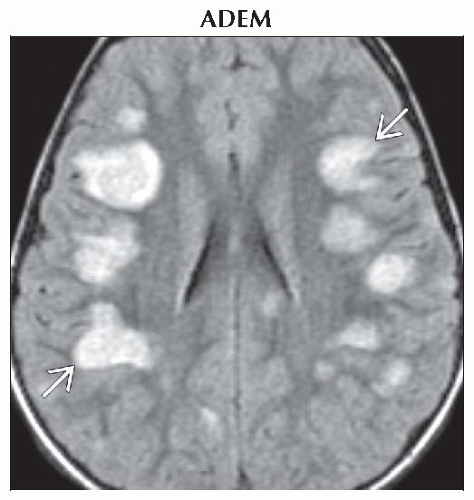
ADEM
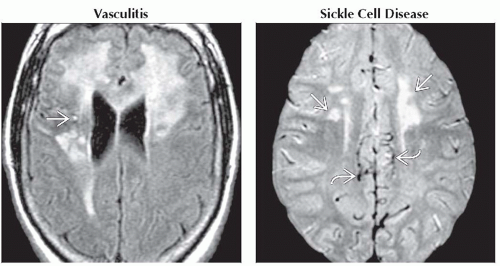
Vasculitis
Sickle Cell Disease
Leigh Syndrome
Thrombosis, Cortical or Deep Venous
CMV, Acquired
CMV, Congenital
Cerebritis
Encephalitis (Miscellaneous)
Herpes Encephalitis
Septic Emboli
Neurocysticercosis (NCC)
Parasites, Miscellaneous
PML
Opportunistic Infection, AIDS
Glioblastoma Multiforme
Gliomatosis Cerebri
Osmotic Demyelination Syndrome
CO Poisoning
Drug Toxicity, NOS
Tuberous Sclerosis Complex
Susac Syndrome
ESSENTIAL INFORMATION
Helpful Clues for Less Common Diagnoses
Cerebral Amyloid Disease
Multifocal juxtacortical small infarcts & hemorrhages of varying ages
Little to no deep white matter (WM) or basal ganglia (BG) involvement
Acute lobar hemorrhage, the usual presenting symptom, typically large
May see confluent WM hyperintensity
ADEM
Multifocal WM lesions, punctate to flocculent, with enhancement, faint & fuzzy early, ring-like later
May mimic MS, but lesions are often more peripheral WM & all at same stage
Usually 10-14 days following infection or vaccination
Vasculitis
Multiple hyperintensities typical; pial & subarachnoid hemorrhage common
Less cortical involvement & more enhancement than embolic stroke
Granulomatous (PACNS), drug-induced, & infectious vasculitis usually moderate-sized vessels: M1 to cortical surface, may involve basal structures
Lupus & radiation-induced vasculitis are small vessel & usually angiographically occult with punctate to confluent hyperintensities
Sickle Cell Disease
Creates a moyamoya pattern of vascular stenosis & occlusion with infarcts in MCA territory or watershed
Demographic & family history differentiate it from classic moyamoya
Leigh Syndrome
Symmetric hyperintensity in regions of oxidative activity
Putamina & periaqueductal gray > caudate > globi pallidi, brainstem, thalami, dentate
Thrombosis, Cortical or Deep Venous
T2 hyperintensity without diffusion restriction unless infarction has developed
Lesions usually solitary when isolated cortical venous
Dural sinus: Multiple lesions
Deep venous: Bilateral thalamic
CMV, Acquired
Opportunistic infection with periventricular (4th > lateral) & cerebellar > cortical hyperintensity with mild enhancement
CMV, Congenital
Multifocal deep band-like T2 hyperintensity with microcephaly & calcifications
Cortical dysplasia, agyria, myelination delay, periventricular cysts
Cerebritis
Early stage of bacterial infection, prior to cavitation & enhancement seen in abscess
Peripheral, poorly marginated large lesion with mass effect
Encephalitis (Miscellaneous)
Most non-herpes encephalitides involve the BG, thalamus, midbrain, & WM
Variable enhancement
Herpes Encephalitis
Cortical & subcortical WM with bilateral, asymmetric involvement of the medial temporal & inferior frontal lobes & insula
Pial-cortical enhancement; DWI positive
Septic Emboli
Scattered small juxtacortical hyperintensities
Develop into small ring-enhancing micro-abscesses
Neurocysticercosis (NCC)
Vesicular phase: Small 10 mm cysts with central dot- or comma-shaped scolex, no edema, follows CSF
Colloidal phase: Cyst may enlarge, is hyperintense to CSF, + surrounding edema, enhancement
Granular nodular & calcified phase: Cyst retracts, wall thickens, edema resolves, calcifies
Parasites, Miscellaneous
Cystic mass or masses with hypointense rim & surrounding edema
Many with hemorrhage, which is uncommon in bacterial infection
PML
Multifocal large WM lesions that lack mass effect, rarely enhance
Involves subcortical U-fibers
Opportunistic Infection, AIDS
Toxoplasmosis: Peripheral ring-enhancing “abscesses”
Cryptococcus: Enlarged perivascular spaces
CMV: Subtle ventriculitis, pial inflammation
Tuberculosis: Meningitis, tuberculous abscesses
Glioblastoma Multiforme
Rarely multifocal or multicentric
Heterogeneous mass with irregular enhancement
May cross the corpus callosum
Gliomatosis Cerebri
Extensive multilobar or diffuse cerebral hyperintensity with mild mass effect
Preservation of underlying architecture
Osmotic Demyelination Syndrome
Central pontine hyperintensity sparing the periphery & cortical spinal tract, round or trident-shaped (CPM)
BG & WM lesions with extra-pontine myelinolysis (EPM)
CO Poisoning
Bilateral globi pallidi hyperintensity ± adjacent hemorrhage
May see putamen, caudate, & WM hyperintensity
Drug Toxicity, NOS
WM multifocal strokes: Cocaine, amphetamine
Diffuse leukoencephalopathy: Inhaled heroin
Tuberous Sclerosis Complex
Cortical tubers: Juxtacortical hyperintensities
Calcified subependymal nodules
Susac Syndrome
Callosal involvement always; central rather than at callosal septal margin seen in MS
Will leave “holes” in central callosum in chronic cases
Involves BG in 70%, much more than MS
Image Gallery
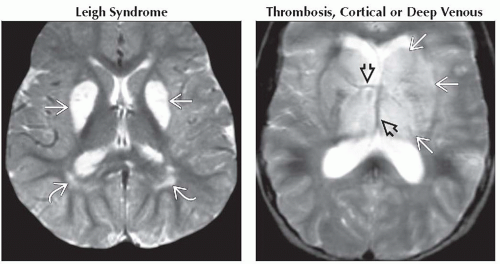 (Left) Axial T2WI MR shows bilateral putaminal hyperintensity
 & swelling classic for acute Leigh syndrome with periatrial signal abnormality & swelling classic for acute Leigh syndrome with periatrial signal abnormality  . (Right) Axial T2WI MR shows hyperintensity & swelling in the thalami, putamina, & caudate heads . (Right) Axial T2WI MR shows hyperintensity & swelling in the thalami, putamina, & caudate heads  bilaterally with hypointensity of the internal cerebral & thalamostriate bilaterally with hypointensity of the internal cerebral & thalamostriate  veins due to deep venous thrombosis. veins due to deep venous thrombosis.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|