Multiple Hyperdense Parenchymal Lesions
Anne G. Osborn, MD, FACR
DIFFERENTIAL DIAGNOSIS
Common
Cerebral Contusion
Diffuse Axonal Injury (DAI)
Hypertensive Intracranial Hemorrhage
Cerebral Amyloid Disease
Metastases, Parenchymal
Cavernous Malformations
Less Common
Cerebral Infarction, Subacute
Thrombosis, Cortical Venous
Acute Hypertensive Encephalopathy, PRES
Anticoagulation Complications
Glioblastoma Multiforme
Lymphoma, Primary CNS
Tuberous Sclerosis Complex
Rare but Important
Tuberculomas
Neurosarcoid
Leukemia
Thrombotic Microangiopathies (HUS/TTP)
Thrombolysis Complications
Parasites, Miscellaneous
Acute Hemorrhagic Leukoencephalopathy
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Hyperdense parenchymal lesions
↑ Attenuation compared to normal brain
Caused by
Clotted blood, most common
Nonhemorrhagic hypercellular mass (electron dense), less common
Calcification (excluded from this differential diagnosis)
Helpful Clues for Common Diagnoses
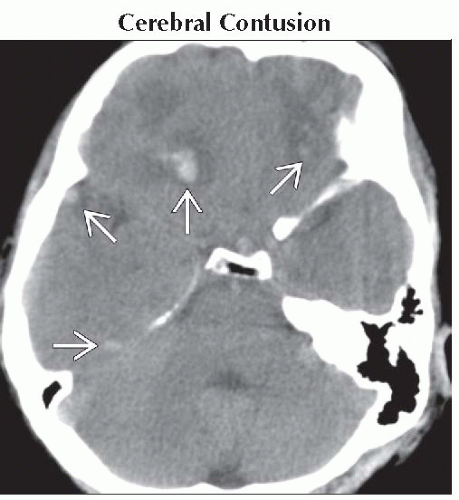
Cerebral Contusion
Peripheral (cortex) > deep lesions
Anteroinferior frontal, temporal lobes most common sites
Patchy superficial hemorrhages ± low density edema
Focal traumatic subarachnoid hemorrhage often associated
Diffuse Axonal Injury (DAI)
Punctate/linear hemorrhages at gray-white junction most common
Other: Corpus callosum, deep gray nuclei, midbrain/brainstem
T2* scan (GRE/SWI) helpful
Hypertensive Intracranial Hemorrhage
Solitary hematoma > patchy/multifocal hemorrhage
Deep > superficial lesions
Nearly 2/3 striatocapsular
Thalamus 15-25%
Look for multifocal “microbleeds” (1-5%), best seen on MR with GRE/SWI sequence
Basal ganglia, cerebellum (vs. cortical, peripheral in amyloid)
Cerebral Amyloid Disease
Causes 15-20% of primary nontraumatic intracranial hemorrhage in older patients
Classic = lobar hemorrhages of different ages
Most common manifestation actually “microbleeds”
Do T2* (GRE or SWI) scan to detect
Metastases, Parenchymal
Electron dense (hypercellular or hemorrhagic)
Some enhancement usually present
Cavernous Malformations
Multiple (familial) lesions
NECT often normal unless acute intralesional hemorrhage
Iso-/hyperdense ± Ca++
Mass effect absent unless hemorrhage
Do MR with T2* (GRE or SWI) for optimal imaging
Helpful Clues for Less Common Diagnoses
Cerebral Infarction, Subacute
Hemorrhagic transformation
Typically 2-3 days after ischemic infarct
Patchy petechial hemorrhages in cortex, basal ganglia
Thrombosis, Cortical Venous
With or without dural sinus thrombosis
Patchy cortical/subcortical petechial hemorrhages
Acute Hypertensive Encephalopathy, PRES
Most common: Patchy hypodense cortical/subcortical foci
Occipital lobes > basal ganglia > brainstem, cerebellum
Less common: Petechial hemorrhages (gross hematomas rare)
Anticoagulation Complications
Mixed density hemorrhages
Fluid-fluid levels, unclotted blood
Glioblastoma Multiforme
Necrosis, hemorrhage common
Low density center, thick irregular high density hypercellular rim
Multifocal GBM, “butterfly” GBM of corpus callosum
Both can appear to have separate hyperdense regions
Can be either hemorrhage or hypercellular regions
Lymphoma, Primary CNS
Iso-/hyperdense lesions in corpus callosum, basal ganglia, periventricular WM
Frank hemorrhage? Suspect HIV/AIDS
Tuberous Sclerosis Complex
98% have Ca++ subependymal nodules
Some cortical, subcortical tubers calcify
Occasional noncalcified cortical, subcortical hyperdensities seen
Helpful Clues for Rare Diagnoses
Tuberculomas
Meningitis > parenchymal lesions
Mildly hyperdense (rim > solid) ± edema
Healed granulomas may calcify
Neurosarcoid
Infiltrates along perivascular spaces → parenchymal mass
May cause focal patchy hyperdense mass(es)
Leukemia
Most parenchymal hyperdensities are hemorrhages
Hypercellular parenchymal masses (chloromas) < extra-axial tumor
Thrombotic Microangiopathies (HUS/TTP)
Thrombocytopenia, intravascular hemolysis characteristic of 3 disorders
Malignant hypertension (often with HUS)
Disseminated intravascular coagulation (DIC)
Thrombocytopenic thrombotic purpura (TTP)
Patchy petechial hemorrhages, predominately cortical
Thrombolysis Complications
10-15% hemorrhage
Petechial > gross lobar
Post-procedural T1 C+ MR may predict hemorrhagic transformation (HT)
If present, risk of HT ↑
Parasites, Miscellaneous
Cysts > hyperdensities
Consider travel history, especially in endemic area
Beware: Conglomerate parasitic masses can mimic brain tumor!
Acute Hemorrhagic Leukoencephalopathy
Fulminant variant of ADEM
Hyperintensities in/along perivascular spaces
Microhemorrhages > gross lesions
CT, MR may not show hemorrhage
Image Gallery
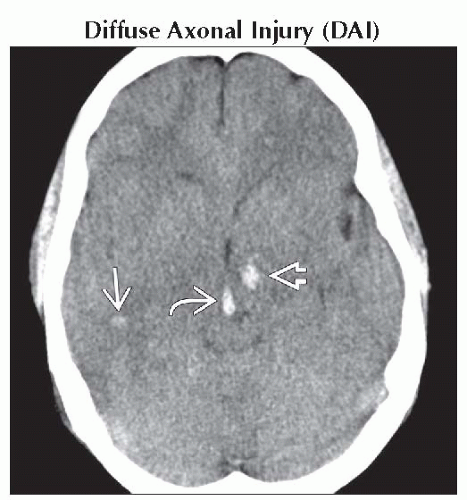 Axial NECT shows scattered hyperdense foci of DAI at gray-white interfaces
 , left thalamus , left thalamus  , and midbrain , and midbrain  . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|