Muscle disease
Primary muscle disease is relatively uncommon (prevalence 12 per 100 000) and may be inherited or acquired. This is an area in neurology where the recent rapid developments in molecular genetics are providing new insights into the molecular basis of muscle disease. This is also leading to developments in the classification of muscle disease, for example the channelopathies.
Inherited diseases include the following:
 Progressive muscular dystrophies causing progressive weakness. The patterns of inheritance, age of onset, patterns of muscular involvement and prognoses differ according to type.
Progressive muscular dystrophies causing progressive weakness. The patterns of inheritance, age of onset, patterns of muscular involvement and prognoses differ according to type. Metabolic myopathies may produce progressive deficits, e.g. most mitochondrial myopathies, or intermittent, particularly exertional symptoms, e.g. McArdle’s disease.
Metabolic myopathies may produce progressive deficits, e.g. most mitochondrial myopathies, or intermittent, particularly exertional symptoms, e.g. McArdle’s disease. Non-progressive congenital myopathies present at various ages and may be mild to severe. Examples include central core, myotubular and nemaline myopathies. All are rare.
Non-progressive congenital myopathies present at various ages and may be mild to severe. Examples include central core, myotubular and nemaline myopathies. All are rare. Myotonic syndromes are characterized by impaired muscle relaxation after contraction, sometimes with muscle weakness.
Myotonic syndromes are characterized by impaired muscle relaxation after contraction, sometimes with muscle weakness. Syndromes of episodic weakness or periodic paralysis due to disorders of ion channels in the muscle membranes.
Syndromes of episodic weakness or periodic paralysis due to disorders of ion channels in the muscle membranes.Muscular dystrophies
Boys with DMD develop weakness of the lower limb girdle by the age of 3–6 years. They adopt the Gower manoeuvre to rise from lying (Fig. 1). Weakness then spreads to other muscle groups in the legs and arms. There may be characteristic rubbery enlargement (pseudohypertrophy) of the calf muscles and 30% have a low IQ. Untreated, most are wheelchair-bound by the age of 12 years and die from respiratory complications by the age of 25 years.
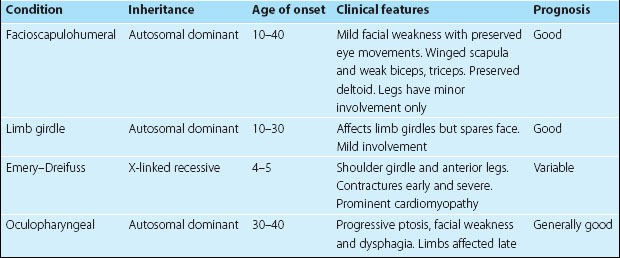
Investigations include muscle creatine kinase (CK), which is highly elevated, and muscle biopsy, which shows no fibres staining for dystrophin. An ECG is often abnormal. Treatment is supportive, especially prevention of complications, including respiratory infection and contractures. Steroids may slow the progression and respiratory support can prolong survival. Genetic treatments and stem cell implants have yet to provide benefit. BMD follows a milder course with an onset at age 5–45 years; there is also calf pseudohypertrophy and a highly elevated CK, 20–200 times normal. Other dystrophies are described in Table 1; some have been identified as affecting proteins closely linked with dystrophin.
Metabolic myopathies
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree