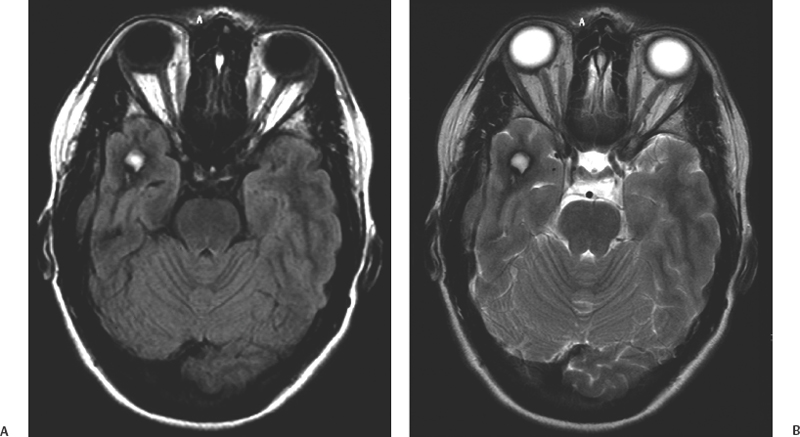
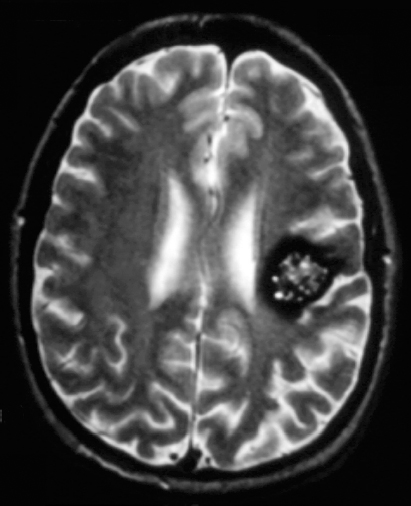
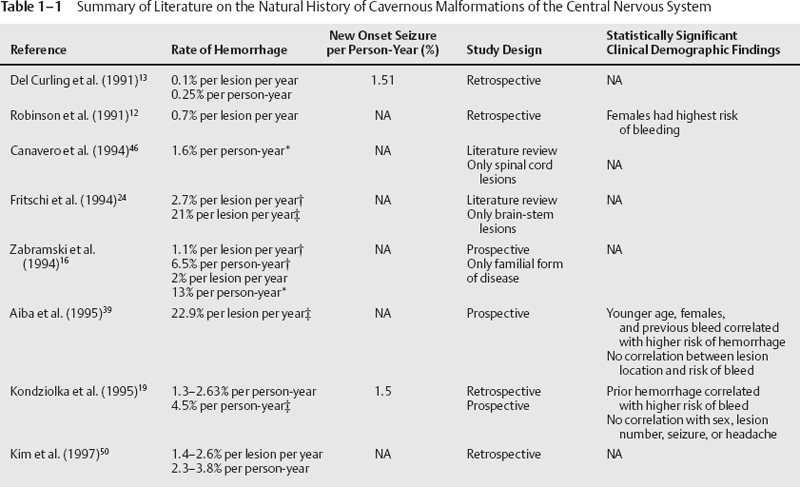
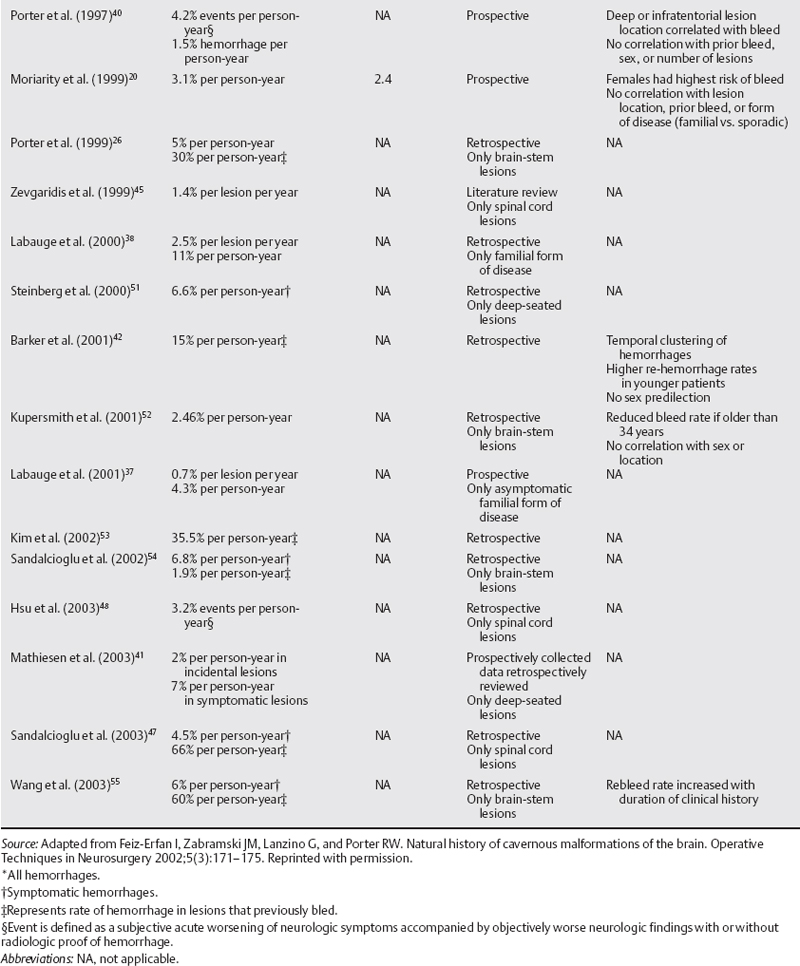
1 Iman Feiz-Erfan, Joseph M. Zabramski, Louis J. Kim, and Jeffrey D. Klopfenstein Cavernous malformations are focal vascular abnormalities that affect the blood vessels supplying the brain. Although cavernous malformations make up only 5 to 10% of all cerebrovascular malformations, they are increasingly recognized as a cause of seizures and focal neurologic deficits.1–4 The introduction of magnetic resonance imaging (MRI) allowed cavernous malformations to be diagnosed without the need for pathologic confirmation, which, in turn, has greatly enhanced our understanding of the natural history of these lesions. The growing availability of MRI has encouraged clinical interest in these lesions, and recognition that a large number of these cases have a familial component has stimulated research into the genetic basis of this disease, which is reviewed elsewhere in this text. A logical approach to the management of these lesions requires that neurosurgeons understand the epidemiology and natural history of cavernous malformations. The purpose of this chapter is to provide readers with an in-depth review of the available literature on these topics and to examine the implications related to the treatment of these patients. Before the introduction of modern imaging technology, cavernous malformations were considered rare lesions. In 1976, Voigt and Yasargil5 described their clinical experience with one case and thoroughly reviewed the world literature; they found only 126 reported cases. Soon after the publication of this article, computed tomography (CT) became widely available. Although CT was a significant advance in neuroimaging, it lacked both sensitivity and specificity for the diagnosis and imaging of cavernous malformations. The subsequent introduction of MRI in the mid-1980s revolutionized our understanding of these lesions. The imaging characteristics of cavernous malformations are sufficiently unique to allow most lesions to be diagnosed on the basis of MR findings alone (Fig. 1-1).6–10 Cavernous malformations are more common than is generally suspected. Postmortem studies performed in the 1980s demonstrated that cavernous malformations affect 0.37 to 0.5% of the population.2,11 Remarkably similar results were reported by two groups reviewing more than 22,000 MR examinations, with incidence rates of 0.4 to 0.5%.12,13 Based on these studies, it is estimated that 18 to 22 million people are affected by cavernous malformations worldwide. Cavernous malformations occur in two forms: spontaneous and familial. The spontaneous form occurs as an isolated case, most commonly with a single lesion, whereas the familial form is characterized by multiple lesions and an autosomal dominant mode of inheritance.14–17 The presence of three or more lesions and a family history of seizures are pathognomonic for the familial form of this disease. Cavernous malformations have been reported in infants and children, but most patients become symptomatic between their second and fifth decades.12,13,16 Not all patients with cavernous malformations are clinically symptomatic. Fifteen to 20% of lesions are incidental findings discovered during a workup for headache.12,13 In the authors’ experience, as many as 40% of patients with the familial form of the disease remain asymptomatic despite the presence of multiple lesions.16 Seizures are the most common manifestation of supratentorial cavernous malformations, accounting for 40 to 80% of the presenting symptoms.1,12,13,15,16,18 A few studies have focused on the future risk of seizure activity in patients harboring asymptomatic cavernous malformations. The rate of new onset of seizures in this group ranges between 1.5 and 2.4% per patient-year.13,19,20 The exact mechanism that leads to seizure activity in these lesions is unknown, but it appears to be related to the deposition of iron in hemosiderin. Iron is a well-known epileptogenic material and has been used to induce seizures in laboratory models of epilepsy.21,22 Focal neurologic deficits are rarely associated with supratentorial lesions. In contrast, the sudden onset of focal neurologic deficits is the most frequent presentation of patients with cavernous malformations involving the brain stem.23–26 Porter et al.26 reported 100 surgical cases of brain-stem cavernous malformations. In their series, 97% of patients presented with focal neurologic deficits from hemorrhage. In the brain stem where lesions may be adjacent to critical tracts and nuclei, even small focal hemorrhages may be poorly tolerated. Symptoms are characteristically maximal at onset. Symptoms from the initial episode tend to resolve as the hemorrhage is organized and absorbed. Often, patients have recovered completely by the time they are seen in neurosurgical consultation. Recurrent episodes of hemorrhage, however, are associated with progressively more severe deficits and an increased risk of permanent neurologic impairment. Death is rare without a history of multiple previous episodes of symptomatic hemorrhage. Figure 1-1 T2-weighted magnetic resonance image demonstrating the classic appearance of a cavernous malformation. Note the reticulated “salt and pepper” core surrounded by a hypointense rim. Numerous studies have been published on the natural history of cavernous malformations (Table 1-1). Most of the data are derived from patients referred to neurosurgical centers and are therefore subject to bias that is likely to inflate hemorrhage rates. On the other hand, calculations that assume that these lesions are present from birth may significantly underestimate the risk of hemorrhage. The congenital nature of cavernous malformations has been recently challenged by well-documented reports of de novo formation of lesions in both sporadic and familial forms of the disease.16,17, 27–36 These uncertainties emphasize the need to rely on prospective natural history data in this population. Another confounding factor is the dynamic nature of these lesions. Zabramski et al. classified cavernous malformations into four types based on imaging characteristics (Table 1-2; Figs. 1-1 to 1–4).16 These authors and others have found that the risk of hemorrhage appears greatest for type I and type II lesions, both of which are more likely to be associated with symptoms.37,38 Most clinical studies are heavily biased to these two lesion types, which are most readily identified on MRI and do not require gradient-echo sequences for visualization.
Natural History of Cavernous Malformations of the Central Nervous System
 Epidemiology
Epidemiology
 Clinical Manifestations
Clinical Manifestations
 Natural History
Natural History
| Lesion Type | MRI Signal Characteristic | Pathologic Characteristics |
|---|---|---|
| Type IA | T1: hyperintense focus of hemorrhage T2: hyper- or hypointense focus of hemorrhage extending through at least one wall of the hypointense rim that surrounds the lesion. Focal edema* may be present. (Figs. 1-2 and 1–3) | “Overt” subacute focus of hemorrhage extending outside the lesion capsule of hemosiderin-stained gliotic brain |
| Type IB | T1: hyperintense focus of hemorrhage T2: hyper- or hypointense focus of hemorrhage surrounded by a hypointense rim (Fig. 1-4) | Subacute focus of hemorrhage surrounded by a rim of hemosiderin-stained macrophages and gliotic brain |
| Type II | T1: reticulated mixed signal core T2: reticulated mixed signal core surrounded by a hypointense rim (Fig. 1-1) | Loculated areas of hemorrhage and thrombosis of varying age surrounded by gliotic, hemosiderin-stained brain; in large lesions, areas of calcification may be seen |
| Type III | T1: iso- or hypointense T2: hypointense with a hypointense rim that magnifies size of lesion GE: hypointense with greater magnification than T2 | Chronic resolved hemorrhage with hemosiderin staining within and around the lesion |
| Type IV | T1: poorly seen or not visualized at all T2: poorly seen or not visualized at all GE: punctate hypointense lesions | Two lesions in the category have been pathologically documented to be telangiectasias |
Source: Adapted from Zabramski JM, Wascher TM, Spetzler RF, et al. The natural history of familiar cavernous malformations: results of an ongoing study. J Neurosurg 1994;80:422–432. Reprinted with permission.
*Focal edema may surround the extralesional portion of hemorrhage in type IA lesions but raises diagnostic concerns in other lesion types.
Abbreviations: GE, gradient-echo sequences; MRI, magnetic resonance imaging; T1, T1-weighted MRI; T2, T2-weighted MRI.
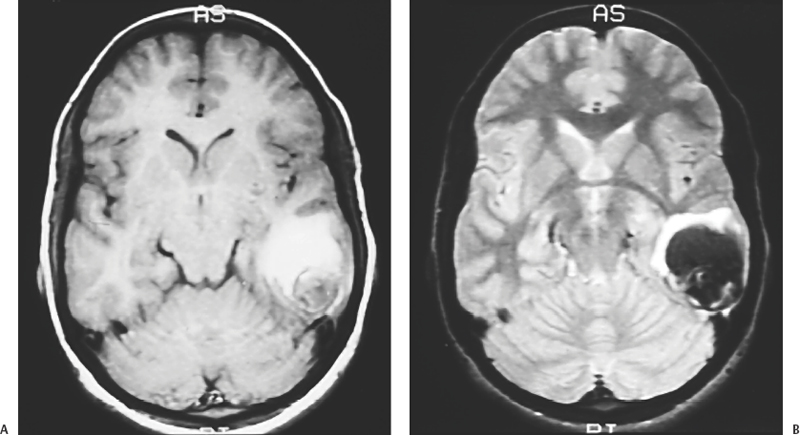
Figure 1-2 Example of a large “overt” hemorrhage (type IA; Table 1-2). (A) T1-weighted and (B) T2-weighted magnetic resonance images demonstrating subacute, extralesional hemorrhage from a pathologically proven posterior temporal lobe cavernous malformation. The signal characteristics of the blood on these images are consistent with early subacute hemorrhage (within 1 week).
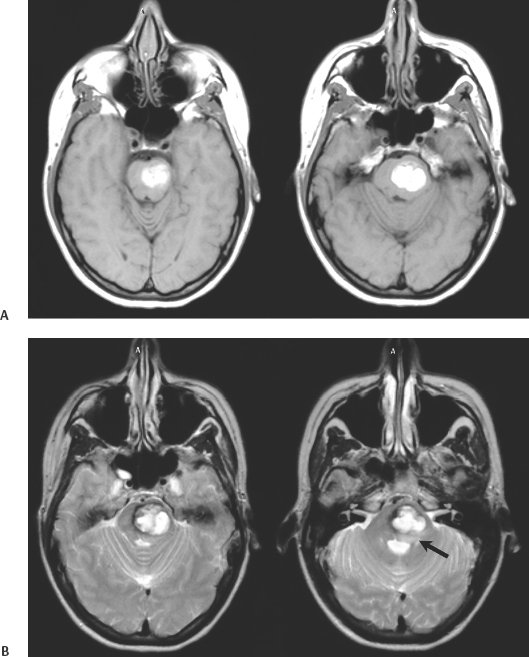
Figure 1-3 (A) T1-weighted and (B)T2-weighted magnetic resonance images demonstrating a subacute “overt” hemorrhage (type IA; Table 1-2) from a brain-stem cavernous malformation. Note the displacement of the fourth ventricle secondary to mass effect, and the focal edema (B, arrow) adjacent to the area of hemorrhage that extends outside the hypointense rim (capsule) that surrounds the remainder of the lesion on the T2-weighted image.
Most studies of the natural history of cavernous malformations have tended to include patients with both the spontaneous and familial forms of the disease. Del Curling et al.13 reviewed 8131 MRI studies performed at their institution over 3 years and identified 32 patients with 76 lesions. Six of these patients had four or more lesions (range, 4 to 19), consistent with a familial etiology. Sixteen patients presented with seizures. Assuming all lesions had been present from birth, they estimated that the risk of seizure development was 1.56% per person-year (1.34% for 26 patients with a single lesion and 2.48% per person-year for the 6 patients with multiple lesions). An additional problem, which is well illustrated in this study, is the lack of a widely accepted definition of hemorrhage. The authors report that only three patients exhibited “clinically significant, radiographically identifiable hemorrhages” and calculated a hemorrhage rate for their cohort of 0.25% per person-year. Yet they note that 7 of 32 patients had focal neurologic deficits attributable to their cavernous malformation at the time of diagnosis and that three patients had a history of prior transient deficits. Of the entire population, only six patients were asymptomatic. Assuming that the onset of seizures and neurologic deficits (whether temporary or permanent) follows at least one episode of hemorrhage, the risk of symptomatic hemorrhage in this cohort would be a minimum of 2.18% per person-year or 0.9% per lesion-year.
In another review of serial MRI studies, Robinson et al.12 identified 66 patients with 76 lesions from 14,035 scans. They prospectively followed 57 patients with 66 lesions for an average of 26 months and found a risk of symptomatic hemorrhage of 0.7% per lesion-year. This rate compares favorably to the adjusted risk of symptomatic hemorrhage of 0.9% per lesion-year for the patients in study by Del Curling et al. and to the risk of symptomatic hemorrhage of 1.2% per lesion-year reported by Zabramski et al.16 in a group of patients with familial cavernous malformations.
Kondziolka et al.19 reported a slightly higher hemorrhage rate of 2.6% per year but noted that the risk of hemorrhage was strongly related to clinical presentation. They followed 122 patients with cavernous malformations for a mean of 34 months. The hemorrhage rate was significantly lower in patients who presented with incidental lesions: 0.6% per year (n = 61) compared with 4.5% per year in those with a history of previous symptomatic hemorrhage (n = 61). Aiba et al.39 noted a similar low risk of hemorrhage in asymptomatic patients. They followed 23 patients with incidental cavernous malformations for a mean of 2.4 years and reported a 0% hemorrhage rate for patients with incidental lesions and rate of 0.4% per year in those with seizures.
Porter et al.40 reported a slightly higher annual event rate of 4.2%. This group defined an event as any neurologic worsening of symptoms with or without radiologically proven hemorrhage. The authors followed 110 patients with cavernous malformations for an average of 46 months, yielding 427 years of observation. In this study, location was the most important factor for predicting future events. Event rates were significantly higher for deeply located (10.6% per year) than for superficially located lesions (0% per year). Radiographically proven interval hemorrhages occurred in seven patients, for an annual risk of 1.6% per patient-year. Six of these seven patients presented with a history of hemorrhage.
Mathiesen et al.41 also noted an increased risk of hemorrhage associated with deep-seated and brain-stem cavernous malformations. The authors followed 11 patients with asymptomatic lesions for an average of 4 years. The symptomatic hemorrhage rate was 2% per patient-year in this group, compared with a hemorrhage rate of 7% per patient-year in 23 patients with symptomatic lesions.
Hemorrhage rates appear to be particularly high in patients who present after bleeding episodes that violate the lesion capsule, producing a so-called overt extralesional hemorrhage (type IA) into the surrounding brain (Figs. 1-2 and 1–3). Aiba et al.39 followed 62 such patients for a mean of 3.12 years. Their risk of recurrent symptomatic hemorrhage was 22.3% per lesion-year. Barker and colleagues42 reported a similar experience with 141 patients selected for intervention who presented with “overt” hemorrhages. In this series, 63 patients experienced a second hemorrhage before treatment. Hemorrhages clustered around the initial event; the re-hemorrhage rate was 25.2% per year for the first 28 months. After this 28-month cutoff, the risk of rebleeding decreased to 9.6% per year. Comparable rates of rebleeding have been reported after incomplete resection of cavernous malformations that interrupt the lesion capsule, stressing the importance of complete resection if surgery is contemplated.24,41,43,44