Neonatal and Pediatric Electroencephalography
QUESTIONS
1. All of the following is true about neonatal electroencephalographic (EEG) electrode placement except:
A. Typically, nine scalp electrodes are used
B. F1 or Fp3 and F2 or Fp4 are the most frontal electrodes placed in accordance to the 10-20 international system
C. The longitudinal bipolar montage is the most commonly used montage for recording
D. Electrooculogram, electromyogram, and respiratory monitoring are often added
View Answer
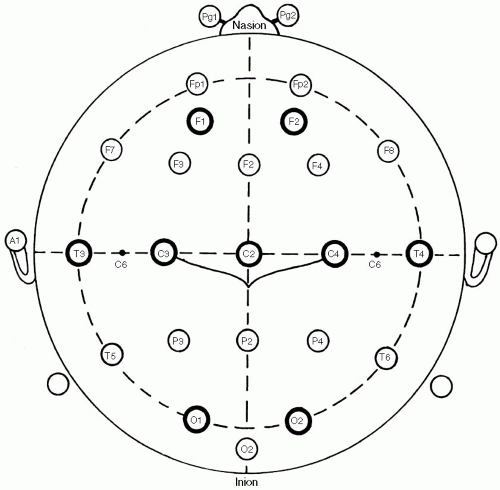
1. (B): Neonatal EEG electrode placement is mildly modified from the 10-20 system to accommodate for the smaller head circumference and the relatively immature frontal lobes. Every EEG laboratory uses its own electrode system, but typically nine electrodes are used (F1, F2, C3, C4, Cz, T3, T4, O1, and O2). F1/Fp3 and F2/Fp4 are the frontal electrodes measuring 20% from the nasion. Also, typically a longitudinal bipolar montage is used for the whole recording in order to identify state changes and characterize reactivity and abnormalities. Commonly, infraorbital and submental electrodes are used to help identify state changes in addition to respiration monitoring which can help distinguish respiration artifact from cerebral activity (Fig. 5.8). (Mizrahi, Hrachovy and Kellaway 2003, pp. 5-10; Ebersole and Pedley 2003, pp. 161-162)
2. In full-term infants, sleep spindles become apparent at the age of:
A. Birth
B. 1 to 3 months
C. 6 to 12 months
D. 12 to 24 months
View Answer
2. (B): Sleep spindles are formed at the age of 1 to 3 months in term infants, maximally in the central regions. They are initially bilateral but asynchronous until the age of 2 years when they become synchronous. In the first year, their morphology may be arciform or comb-like maturing in the later stages of life. They are also more frequent in the early years of life during NREM sleep. Spindle duration is approximately 2.5 seconds at 3 months and 0.75 seconds at 22 months. Spindle frequency remains constant at 12 to 16 after age 5. (Blume and Kaibara 1999, pp. 5-6, 124-128; Daube 2002, p. 114)
3. Canavan disease will likely produce:
A. Generalized spike-and-wave discharge
B. Diffuse polymorphic delta activity
C. Periodic lateralized epileptiform discharges (PLEDs)
D. Temporal intermittent rhythmic delta activity (TIRDA)
View Answer
3. (B): Canavan disease like all leukodystrophies affects the white matter. In the case of Canavan disease, there is diffuse white matter disease, which will produce diffuse EEG slow activity such as continuous polymorphic delta activity. Polymorphic delta activity consists of high-amplitude delta waves with irregular shapes and variable duration and frequency. This EEG pattern represents a nonspecific diffuse cerebral dysfunction and is often nonepileptiform in nature. For example, it can be seen in toxic, metabolic states as well as brainstem lesions such as the diencephalon.
PLEDs and TIRDA may also represent nonspecific EEG patterns but they are often associated with focal lesions. Generalized spike-and-wave discharges are seen in generalized epilepsies. (Ebersole and Pedley 2003, pp. 294-295, 515)
4. The EEG of patients with Rasmussen syndrome is likely to reveal:
A. Absence status
B. Focal electrographic status
C. Generalized attenuation
D. Burst suppression pattern
View Answer
4. (B): Rasmussen syndrome is characterized by progressive intellectual deterioration and recurrent seizures of different types that usually progress into the form of epilepsia partialis continua (in 50% of the cases), also known as focal motor status epilepticus. Clinically, the seizures are simple motor with possible progression into complex partial or secondarily generalized seizures. Because this disease affects the cortical and subcortical areas of one hemisphere, the interictal EEG may show lateralized slow activity and abundant epileptiform discharges. Hemispherectomy is usually the treatment of choice. (Wyllie, Gupta and Lachhwani 2005, pp. 272-273)
5. The EEG of a 6-year-old boy with progressive regression of speech will more likely show abnormalities during:
A. Wakefulness
B. Drowsiness
C. Non-rapid eye movement (NREM) sleep
D. REM sleep
View Answer
5. (C): The clinical history may be consistent with the diagnosis of acquired epileptic aphasia commonly referred to as Landau–Kleffner syndrome. This condition affects young children (3 to 9 years of age) causing regression of speech, personality changes, with or without seizures.
The EEG often shows focal, bilateral independent, or generalized epileptiform activity in the form of spikes or spike-and-wave discharges. These discharges are markedly activated during NREM sleep when they become extremely frequent. These discharges can be missed in wakefulness, drowsiness, or REM sleep recordings. (Ebersole and Pedley 2003, pp. 554-556)
6. The EEG tracing shown in Figure 5.1 is that of a healthy 6-year-old girl. Which of the following medical conditionsmay exacerbate this EEG pattern?
A. Acute intermittent porphyria
B. Alzheimer’s dementia
C. Reye syndrome
D. Hashimoto’s thyroiditis
View Answer
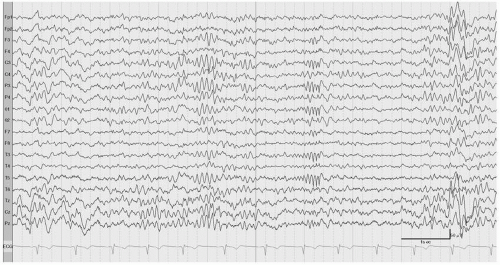
6. (C): This EEG tracing (Fig. 5.1) is displayed in an average referential montage. The presence of vertex waves and low-voltage mixed theta and delta activity suggest a drowsy or light sleep state. There is a burst of sharply contoured waveform of 14 and 6 Hz frequency. This EEG pattern is referred to as 14 and 6 positive spikes and is most prominently seen in the posterior temporal region of healthy children. This pattern is most prominent in drowsiness and light sleep.
Interestingly, this EEG pattern is excessively seen in children with Reye syndrome (acute childhood toxic encephalopathy). Reye syndrome is always associated with hepatic dysfunction but unlike in adults it is not strongly associated with triphasic waves. (Ebersole and Pedley 2003, pp. 359-361; Blume, Kaibara and Young 2002, pp. 168-169)
7. Hypnagogic hypersynchrony is most commonly seen in:
A. Neonates
B. Children
C. Menstruating women
View Answer
7. (B): Hypnagogic hypersynchrony refers to a normal EEG pattern seen at the beginning of drowsiness. It consists of abrupt onset of rhythmical and bisynchronous 4 to 5 Hz high-amplitude waves, often with a wide distribution. It is first seen in children aged 3 months and gradually vanishes by age 12 years. It can also occur at the end of drowsiness when it is referred to as hypnopompic hypersynchrony. (Fisch 1999, pp. 172-173; Ebersole and Pedley 2003, pp. 132-140)
8. The EEG tracing shown in Figure 5.2 belongs to a normal child. On the basis of this EEG, the age of this child is most likely:
A. Neonate
B. 3 months to 2 years old
C. 2 to 5 years old
D. 6 to 8 years old
View Answer
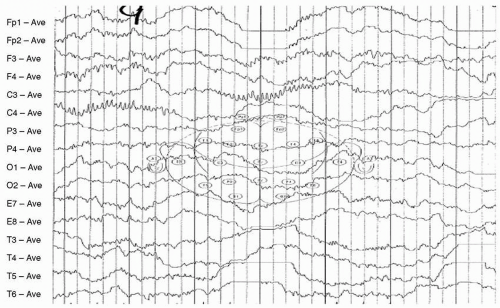
8. (B): This EEG tracing (Fig. 5.2) is displayed in an average referential montage. There are symmetrical but asynchronous sleep spindles, maximally seen in the central electrodes. Sleep spindles are initially formed bilaterally but asynchronously by 1 to 3 months of age. They are predominantly synchronous by the age of 2 years. If they remain asynchronous, they are suggestive of structural abnormalities such as agenesis of the corpus callosum. (Ebersole and Pedley 2003, pp. 144-145; Blume and Kaibara 2002, pp. 123-126)
9. West syndrome is characterized by:
A. Myoclonic seizures
B. Infantile spasms
C. Absence seizures
D. All of the above
View Answer
9. (B): West syndrome consists of a triad of infantile spasms, developmental delay, and a grossly abnormal EEG pattern termed hypsarrythmia. It usually affects infants between the ages of 4 to 8 months. In most cases, West syndrome is associated with serious neurologic abnormalities, including genetic, structural, metabolic, or infectious. (Ebersole and Pedley 20003, pp. 540-544)
10. The recommended length of a neonatal EEG is:
A. 20 minutes
B. 30 minutes
C. 60 minutes
D. 90 minutes
View Answer
10. (C): The recommended length of a neonatal EEG recording is 60 minutes. This is because the neonatal sleep cycle is approximately 45 to 60 minutes in a full-term neonate. This will allow the sampling of all the neonatal sleep stages that approximately include 25 minutes of active sleep, 20 minutes of quiet sleep, and 15 minutes of intermediate sleep. Unlike neonates, adults have a typical sleep cycle of 80 to 120 minutes. (Fisch 1999, pp. 159, 205-206)
11. At which gestational age is wakefulness distinguished from sleep?
A. 28 to 30 weeks
B. 30 to 34 weeks
C. 34 to 36 weeks
View Answer
11. (B): Wakefulness or active sleep can be distinguished from quiet sleep by the gestational age of 30 to 34 weeks. Sleep is divided into active and quiet sleep. Wakefulness and active sleep are similar to REM sleep in which the muscle tone is low, respiration and ECG are irregular, and grimaces and twitches are common. At the age of 30 to 34 weeks, the active sleep EEG consists of a relatively more continuous pattern with shortening of the interburst interval duration.
On the other hand, quiet sleep which is similar to non-REM sleep consists of reduced eye and muscle movements with regular ECG and respiration rate. Quiet sleep EEG remains discontinuous with prolonged interburst interval duration known as tracé discontinu. (Mizrahi, Hrachovy and Kellaway 2003, pp. 56-61; Eebersole and Pedley 2003, pp. 183-184)
12. The EEG recording of a 15-year-old male patient with progressive cognitive decline reveals regular periodic complexes every 8 seconds. The likely diagnosis is:
A. Lithium toxicity
B. Rasmussen syndrome
C. Subacute sclerosing panencephalitis
D. Creutzfeld-Jacob disease
View Answer
12. (C): Subacute sclerosing panencephalitis (SSPE) is a slowly progressive encephalitis characterized by cognitive decline, behavioral changes, myoclonus, seizures, movement disorder, and visual loss. SSPE is caused by central nervous system (CNS) involvement with the measles virus. It carries a very poor prognosis.
In this condition, the periodic EEG complexes are pathognomonic in the appropriate clinical setting. Complexes are of high voltage; usually consisting of diffuse or symmetrical sharp waves or sharply contoured waves that are persistent throughout the recording. The interval varies from 4 to 20 seconds, being longer in the early stages of the disease and shorter with disease progression. Compressing the EEG by decreasing the speed of recording may help in appreciating the regularity of the long interval complexes. When present, myoclonic jerks tend to occur in deep sleep and almost always coincide with the complexes. (Blume and Kaibara 1999, pp. 283, 368-370)
13. A 7-year-oldmale has nocturnal seizures consisting of strange guttural noise and left face contraction followed by generalized jerking. The highest yield EEG is during:
A. Hyperventilation
B. Photic stimulation
C. Wakefulness
D. Sleep
View Answer
13. (D): The age and description of the seizures is consistent with benign epilepsy with centrotemporal spikes (BECTS) also known as benign rolandic epilepsy. Onset of seizures occurs between the ages of 4 to 10 years. Clinically, seizures are common during sleep (80% of times) consisting of unilateral tonic or clonic activity of the face and excessive salivation often followed by secondarily generalization.
Interictal EEG demonstrates characteristic central midtemporal spikes. Sleep dramatically activates these discharges. Discharges are more common in slow wave sleep than REM sleep. About one third of patients have interictal discharges only during sleep. (Ebersole and Pedley 2003, pp. 526-532)
14. The EEG recording shown in Figure 5.3 ismost consistent with the diagnosis of:
A. West syndrome
B. Lennox-Gastaut syndrome
C. Benign epilepsy with centrotemporal spikes
D. Juvenile myoclonic epilepsy
View Answer
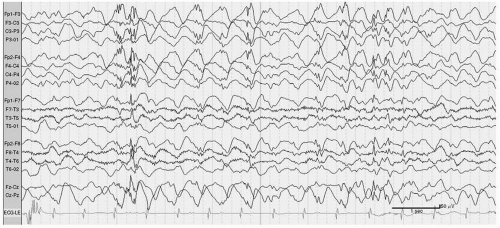
14. (B): This EEG tracing (Fig. 5.3) is displayed in a longitudinal bipolar montage. The background activity is disorganized with frequent 1.5 to 2 Hz generalized spike-and-wave discharges. These, referred to as slow spike-and-wave discharges, are seen in Lennox-Gastaut syndrome (LGS), a form of symptomatic generalized epilepsy. Slow spike-and-wave discharges can be symmetrical, can have shifting predominance, or even be consistently asymmetrical. They are commonly seen in the anterior and central regions and are typically seen during NREM sleep. Patients with LGS usually have an abnormal background in waking. (Ebersole and Pedley 2003, pp. 548-551; Blume and Kaibara 1999, pp. 156-157)
15. The EEG of a 6-year-old boy with congenital blindness willmost likely show:
A. Slowing of the occipital rhythm
B. Occipital spikes
C. A and B
View Answer
15. (C): Congenital blindness is commonly associated with ipsilateral occipital spikes and slowing of occipital rhythm. Occipital abnormalities are more prominent in patients with amblyopia or blindness that started early in life. These discharges are not associated with increased risk for seizures. Other abnormalities include loss of photic response and absence of positive occipital sharp transients (POSTs) during sleep and lambda waves during wakefulness. (Fisch 1999, pp. 340-341; Blume and Kaibara 1999, p. 352)
16. The EEG recording shown in Figure 5.4 ismost consistent with the diagnosis of:
A. Multifocal epilepsy
B. Benign rolandic epilepsy with centrotemporal spikes
C. Symptomatic generalized epilepsy
D. Idiopathic generalized epilepsy
View Answer
16. (B): This EEG tracing (Fig. 5.4) is displayed in a referential average montage. There are frequent single or runs of spikes during sleep, recorded independently from the two sides. The spikes have a peak negativity (upward deflection) in the central (C3 or C4) and midtemporal regions (T3). They also have a positive end (downward deflection) in the frontal region (Fp1, Fp2, F3, F4, Fz) and vertex (Cz). These findings are typical of BECTS. Spikes could be bilateral (as in this case) or unilateral. Sleep dramatically enhances rolandic spikes, and wakefulness may abolish them completely. The frequency of rolandic spikes does not correlate with seizure frequency or severity. Most patients with BECTS will have normal EEGs in late adolescence. The background is typically normal. (Ebersole and Pedley 2003, pp. 526-531; Blume and Kaibara 1999, pp. 159, 236-244)
17. A 12-year-old male with severe autism has bursts of high-amplitude 3 Hz sharply contoured delta activity during hyperventilation. This is most consistent with the diagnosis of:
A. Symptomatic generalized epilepsy
B. Lennox-Gastaut syndrome
C. Encephalopathy
D. Normal finding
View Answer
17. (D): Hyperventilation is routinely performed to activate generalized 3 Hz spike-and-wave discharges and absence seizures. Hyperventilation effect is more pronounced in children, resulting in high-amplitude bisynchronous delta activity. The morphology of the response can be notch shaped or sharply contoured. Only the presence of a classic generalized spike-and-wave or spike-and-slow wave morphology or clear focal abnormality is considered abnormal. (Fisch 1999, pp. 219-223; Blume and Kaibara 1999, pp. 4-5, 89-91)
18. Which of the following EEG properties of benign occipital epilepsy of childhood is true?
A. Interictal discharges are always seen in the occipital regions
B. Extraoccipital epileptiform discharges are not present
C. Ictal discharges consist of low-voltage fast activity in late onset benign occipital lobe epilepsy
D. Discharges are attenuated with eye opening
View Answer
18. (D): Benign occipital epilepsy is divided into early onset (Panayiotopoulos) or late onset (Gastaut) types. Clinically, they are associated with visual symptoms and vomiting with frequent secondary generalization. Most children outgrow these seizures.
Interictal EEG epileptiform discharges are seen in approximately 80% of patients, consisting of unilateral or bilateral repetitive spikes or sharp waves in the occipital region. Extraoccipital spikes are common in the Panayiotopoulos type, and can be the only abnormality in approximately one third of patients. Discharges are attenuated when eyes are open and activated when eyes are closed. Ictal EEG consists of rhythmic posterior delta or theta discharge in the Panayiotopoulos type and fast posterior rhythmic discharge in the Gastaut type. (Wyllie, Gupta and Lachhwani 2005, pp. 382-385; Daube 2002, p. 118)
19. Benign EEG patterns in a 7-year-old child include all of the following except:
A. Frontal intermittent rhythmic delta activity (FIRDA)
B. 14 and 6 Hz positive spikes
C. Rare frontal sharp waves
View Answer
19. (C): 14 and 6 positive spikes bursts occur normally during drowsiness, mostly in the posterior temporal region at a frequency rate of 14 and 6 Hz. FIRDA is a normal finding in children. Posterior slow waves of youth are delta activity superimposed to the occipital rhythm. It reacts to eye opening and closure in the same manner as the posterior rhythm. Frontal sharp waves are abnormal in children or adults. (Daube 2002, pp. 115-118)
20. In a 28-week preterm infant, the EEG shows a pattern of:
A. Tracé alternant
B. Tracé discontinu
C. Tracé continu
D. Tracé parallel
View Answer
20. (B): At a gestational age of 28 to 30 weeks, the EEG activity usually consists of a burst of mixed frequency (mostly delta frequency) in a discontinuous manner interspaced with periods of EEG attenuation lasting for few seconds to 1 to 2 minutes. The higher amplitude of the bursts occurs in the posterior region. This EEG pattern is referred to as tracé discontinu. At this age, there is no distinction between sleep and awake states. (Mizrahi, Hrachovy and Kellaway 2003, pp. 56-59)
21. A 12-year-old boy has EEG attenuation in the left hemisphere. Among the following, which condition ismost likely to show this finding?
A. Tuberous sclerosis
B. Neurofibromatosis I
C. Sturge-Weber
D. Von-Hippel Lindau
View Answer




21. (C): EEG voltage attenuation can result from cortical injury or dysfunction or signal attenuation by increased distance between the cortex and recording electrodes. Hemispheric voltage attenuation is commonly seen with Sturge-Weber disease. (Ebersole and Pedley 2003, p. 316)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree