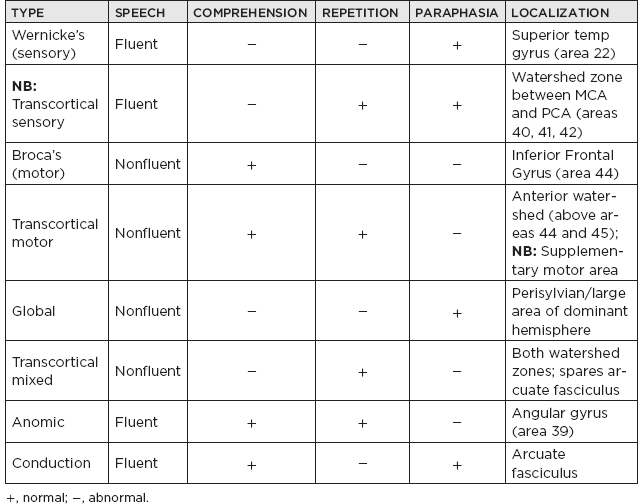
CHAPTER 30 Neurobehavior and Neuropsychology I. Functional-Anatomic Correlations: Review Chapter 4 to identify vessels supplying these important regions of the brain. A. Frontal lobes 1. Luria description of functions a. Identification of problems or objectives b. Formulation of strategies and selection of an appropriate plan c. Execution of the plan d. Evaluation of outcomes 2. Specific behavioral signs and symptoms of frontal damage a. Lateralized signs/symptoms i. Either frontal lobe: release of primitive reflexes (grasp, root, palmomental, suck, glabellar, snout); witzelsucht (inappropriate jocularity); depression ii. Dominant frontal lobe: left-hand apraxia (inability to perform learned patterned movements); poor verbal fluency, including Broca’s aphasia iii. Nondominant frontal lobe: decreased attention; loss of prosody (emotional content of speech); nonspecific behavioral symptoms; mania iv. NB: Bilateral damage: abulia, mutism; poor attention; rigid thinking; gait and sphincter disturbances b. By specific region i. Orbitofrontal—the region of social and interpersonal function: disinhibition, lability, euphoria, lack of remorse or social propriety/comportment Witzelsucht (inappropriate jocularity) is seen in patients with orbitofrontal cortex lesions. ii. Dorsolateral—executive function: poor planning, decreased motivation and flexibility, unable to resist reaction to environmental stimuli iii. Medial: apathy, akinetic mutism Pseudobulbar affect: exaggerated emotional response incongruent to mood. Treat with dextromethorphan/quinidine sulfate. B. Parietal lobes: carry out diverse functions that help us to interpret the environment and our place within it; perform higher-order and multimodal processing of incoming sensory information 1. Damage to either side a. Sensory extinction of the contralateral side of the body b. NB: Hemineglect of the opposite side of space i. May include neglect of body parts (amorphosynthesis) ii. Hemineglect is sometimes accompanied by anosognosia (unawareness of deficits). NB: More common with right-sided parietal lesions. Left-sided lesions may produce transient right-sided neglect, but resolve within a few days. 2. Dominant parietal lobe damage a. Alexia (impaired ability to read) b. Bilateral astereognosis c. Bilateral ideomotor apraxia d. NB: Gerstmann syndrome: tetrad—dysgraphia, dyscalculia, right–left disorientation, finger agnosia; the individual signs of the syndrome are not localizing. e. NB: Alexia without agraphia: intact writing with impaired reading due to damage to dominant occipital, parietal, and forceps major of corpus callosum 3. Nondominant parietal lobe damage a. Constructional apraxia (impaired ability to draw or copy figures) b. Difficulty with visuospatial memory c. Confusion (especially with acute damage, such as cerebrovascular accident) d. Apraxia of eyelid opening—difficulty opening eyes despite normal consciousness and strength Reduplicative paramnesia (reduplication of place) has been associated with combined lesions in the right parietal and bifrontal areas. Anosodiaphoria (indifference to the condition despite recognition of the deficit) is seen with right-hemisphere lesions. 4. Bilateral parietal damage a. NB: Balint’s syndrome i. Caused by damage to posterior superior watershed areas (Brodmann’s areas 19 and 7) ii. Simultanagnosia—inability to relate objects presented together, or appreciate the sum for the parts (e.g., looking at an American flag, a patient might say, “I see a white star,” then, “I see a stripe”) iii. Oculomotor apraxia—inability to direct oculomotor function; paralysis of optic fixation—inability to purposefully direct one’s eyes to a target in a logical fashion iv. Optic ataxia—misreaching in response to visual stimuli, inability to visually direct to a target (patients experience dysmetria with overshooting and undershooting target until they receive proprioceptive or auditory cues, then are able to do task) b. Spatial disorientation C. Temporal lobes: the major functions associated with the temporal lobes are memory, language, and auditory processing. 1. Hemispheric dominance a. “Dominant” is defined by the hemisphere responsible for language. b. Left-hemisphere dominance in 96% of right-handers, 70% of left-handers c. Right-hemisphere dominance in 4% of right-handers, 15% of left-handers d. Bilateral dominance in 0% of right-handers, 15% of left-handers 2. Damage to either temporal lobe a. Hallucinations (any sensory modality) b. Delirium c. Distortions in time perception 3. Damage to dominant temporal lobe a. Aphasias b. Verbal amnesia Aphasias. Naming is poor in all of these syndromes; note that the transcortical (also called extrasylvian) aphasias have spare repetition. In advancing Alzheimer’s disease, speech remains intact as language deteriorates. The result is an aphasia in which the patient is fluent but makes paraphasic errors, with poor comprehension but preserved repetition, similar to transcortical sensory aphasia. 4. Damage to nondominant temporal lobe a. Impaired performance with visual testing b. Impaired visual memory c. Impaired recognition of harmony and melody/prosody of language Topographic disorientation (impaired orientation and navigation in the environment) occurs with a lesion in the right posterior parahippocampal region or the infracalcarine cortex, but a milder form may be seen with a lesion in the right parietal area. 5. Bilateral temporal damage a. Korsakoff’s dementia b. NB: Klüver-Bucy syndrome i. Usually with anterior temporal damage ii. Hyperorality, hypersexuality, apathy, hypermetamorphosis (overly sensitive or acutely aware of minute stimuli in the environment, resulting in preoccupation with these stimuli), and visual agnosia. iii. Aggression is not a component of the syndrome! c. Inability to ignore visual stimuli D. Occipital lobes: receive visual input and perform visual processing; information encoded with the identity of objects is routed ventrally (“what” stream) toward temporal lobes; data about the location and movement of environmental objects (“where” stream) are routed dorsally, to the parietal lobes. 1. Damage to either occipital lobe can cause simple visual hallucinations. 2. Damage to dominant occipital lobe a. Visual object agnosia (inability to identify objects by sight) i. NB: Interhemispheric fibers (from/to splenium) may be involved; disconnects primary visual cortex from language areas; signs: often associated with color anomia, alexia without agraphia (pure word blindness) (A) Patient unable to read words (B) Patient able to write, speak, and spell (C) Patient may be able to read individual letters and numbers 3. Damage to nondominant occipital lobe a. May cause contralateral visual neglect b. Visuospatial disorientation c. Visual illusions and hallucinations 4. Bilateral occipital damage a. NB: Cortical blindness: patient is unable to see; no response to visual threat; pupils remain reactive; Anton’s syndrome—anosognosia for cortical blindness. b. Achromatopsia (loss of color perception) c. NB: Balint’s syndrome (see Section I.B.4.a) d. NB: Prosopagnosia (inability to recognize faces) i. Can occur in the absence of other visual deficits ii. Commonly associated with achromatopsia iii. NB: Requires ventral occipitotemporal lesion (“what” pathway) E. Disconnection syndromes 1. Callosal disconnection a. NB: Left posterior cerebral artery territory and splenium i. Right homonymous hemianopsia—all visual information enters right hemisphere. ii. Damaged posterior corpus callosum prevents right occipital lobe from communicating with language centers on the left; alexia (inability to read), color anomia (inability to name colors); the ability to copy words is spared—motor information crosses in anterior corpus callosum. b. Anterior corpus callosum: disconnects right-hemisphere motor and sensory integration centers from left-hemisphere language areas: signs: apraxia of left hand, agnosia of fingers of left hand Callosal apraxia results from a lesion in the genu of the corpus callosum, resulting in limb kinetic apraxia. Tactile and auditory input cross the corpus callosum posteriorly and are therefore unaffected by a genu lesion! c. Complete callosotomy i. Alien hand (nondominant hand performs apparently independent acts) ii. Disconnection of dominant-sided sensory input (going to the nondominant side of the brain) from the patient’s ability to describe or name the phenomena 2. NB: Arcuate fasciculus—conduction aphasia 3. Subcortical fibers in dominant temporal lobe a. Damages Wernicke’s area and interhemispheric fibers b. No access of auditory input to language area c. Causes pure word deafness—sounds are appreciated, but not speech II. Medical Diseases Causing Psychiatric Symptoms A. Cerebrovascular disease 1. Most common sequela is depression. a. Of stroke victims, 30% to 40% have depression. b. Previously associated with left frontal infarction in particular. 2. Poststroke mania associated with right-sided lesions B. Epilepsy 1. 30% to 50% have psychiatric illness 2. Increased risk of suicide 3. Auras—hallucinations and affective changes 4. Ictal—rarely, complex partial seizures cause violent behavior. 5. Postictal—psychosis, confusion 6. Interictal a. Personality disturbances i. Hyper-religiosity ii. Viscous (“complex partial personality”); circumstantial, pedantic, ponderous speech; hypergraphia iii. Sexual behavior: hyposexuality most common; fetishism, transvestism, deviant interests b. Psychosis i. Usually develops after years of epilepsy ii. Often preceded by other personality changes 7. Medications: all compounds that suppress cerebral activity can cause changes in energy, sleep, appetite, and concentration. a. NB: Topiramate i. Psychosis ii. Cognitive slowing iii. Anomia b. Benzodiazepines and barbiturates i. Cognitive impairment ii. Depression c. Keppra i. Irritability ii. Depression d. Anticholinergics i. Memory loss ii. Hallucinations C. Multiple sclerosis 1. Depression a. 25% to 50% of patients b. Carries a higher risk of suicide 2. Witzelsucht a. Frontal subcortical dementia b. Subsyndromal mania 3. Personality change—irritability or apathy D. Movement disorders 1. NB: Parkinson’s disease a. Depression: may be difficult to distinguish from masked facies and generalized bradykinesias that are part of the motor manifestations of Parkinson’s disease i. Present in 30% to 45% of patients ii. It may be presenting symptom, and it may not be correlated with motor severity. b. Dementia in 30% c. Psychosis i. Associated with dopamimetics, but can occur without ii. Approach (A) Rule out concurrent medical illness causing delirium. (B) Decrease anti-Parkinson’s medications, if possible. (C) NB: Treat with low-dose atypical antipsychotics (quetiapine or clozapine). 2. NB: Huntington’s disease a. Can be accompanied by severe depression and suicidality b. Dementia, psychosis, or irritability may precede motor dysfunction. 3. NB: Wilson’s disease a. Irritability and excessive emotionality may be first symptoms. b. Delirium and dementia may present late or early. 4. Essential tremor a. Associated with anxiety b. Because of beneficial effects of ethanol, abuse may result. E. NB: Acute intermittent porphyria 1. Affects females more than males; between ages 20 and 50 years 2. NB: Recurrent triad: abdominal pain, motor polyneuropathy, psychosis 3. Seizures in 15% 4. NB: Barbiturates and antiepileptics can exacerbate or precipitate attacks. 5. Treatment a. Glucose and hematin infusions (to inhibit aminolevulinic acid [ALA] synthetase) b. Gabapentin for seizures F. NB: B12 deficiency (subacute combined degeneration) 1. Usually results from poor absorption a. Failure to secrete required intrinsic factor, or b. Dysfunction of terminal ileum (absorption site) 2. Psychiatric: depression, dementia, delirium, psychosis 3. Neurologic abnormalities (present in 80%) a. Length-dependent demyelinating polyneuropathy b. Myelopathy (demyelination of posterior columns and lateral corticospinal tracts) 4. Hematologic abnormalities a. Megaloblastic (“pernicious”) anemia b. Hypersegmented neutrophils c. May follow neuropsychiatric symptoms G. HIV 1. Depression very common 2. Dementia 3. Neuropsychiatric disturbances from secondary infections—neuropsychological assessment 4. HAND: HIV-associated neurocognitive disorder: associated with widespread white-matter involvement H. Thyroid disorders 1. Hyperthyroidism a. Anxiety b. Apathy in elderly 2. Hypothyroidism a. Depression b. Cognitive decline III. Intelligence A. Wechsler Adult Intelligence Scale and Wechsler Intelligence Scale for Children 1. NB: Most common test used in clinical practice 2. Six verbal subtests: Information, Comprehension, Arithmetic, Similarities, Digit Span, Vocabulary 3. Four performance subtests: Block Design, Picture Arrangement, Object Assembly, Digit Symbol 4. Scores a. Mean = 100 b. Standard deviation = 10 c. Average range: 90 to 110 d. Intelligence quotient less than 70 defines mental retardation (2.2% of population) 5. Advantages a. Extremely high reliability b. High validity for detecting mental retardation and predicting school performance c. Can be used to localize cerebral dysfunction d. Can compare function in different domains 6. Disadvantages a. Performance subtest is age-sensitive b. Some false lateralization with subcortical or parietal lesions B. Stanford-Binet Test 1. Once the gold standard for children, but now less popular than Wechsler Intelligence Scale for Children 2. Mostly used in psychiatry and education IV. Frontal Lobes A. Executive functioning and reasoning 1. NB: Wisconsin Card Sorting Test a. Subject sorts cards with objects of different shape, color, form, and number i. Initially, the patient does not know the rule. ii. The examiner tells the patient whether the sorting is correct. iii. Scored by the number of trials required to obtain 10 consecutive correct responses iv. Once goal is achieved, the examiner changes the rule again. b. Tests cognitive flexibility (ability to avoid perseveration) and abstract thought i. Sensitive to frontal lobe dysfunction ii. Also abnormal in patients with schizophrenia and caudate lesions 2. Tower of Hanoi, Tower of London a. Subject moves blocks from starting arrangement to goal arrangement. b. Scored by number of moves required (the fewer moves, the better) c. Excellent test of planning abilities/executive function 3. Bedside maneuvers a. Ability to perform nonutile motor sequences (Luria tests): with minimal or no practice, the intact brain can learn simple motor sequences simply by mimicry; the more complex or variable the rhythm or sequence, the more sensitive the test is for frontal lobe dysfunction. i. Two-step hand sequence (reciprocally alternating fists and prone hands) ii. Three-step hand sequence (“fist-edge-palm”) iii. Rhythm tapping iv. Alternating pattern (drawing alternating peaks and blocks) b. Suppression of motor impulses: the intact frontal lobes should be able to suppress the instinctive tendency to direct activity toward novel stimuli. i. Crossed response inhibition (“raise the hand that I don’t touch”) ii. Antisaccades (“look away from the finger that moves”) iii. “Go/no-go” evaluates for errors of commission (e.g., tapping when asked not to) c. Creativity: the normal frontal lobes are able to categorize and retrieve items in memory that have concrete or abstract relationships to one another. i. “Thurstone” Controlled Oral Word Association Test (“all the words that start with the letter —”) ii. Category fluency (“name all the [farm animals, cities] you can in 1 minute”) d. Suppression of primitive reflexes: glabellar (Myerson’s), snout, rooting, suck, Babinski, grasp (palmar and plantar), and palmomental reflexes are present in early life but sequentially extinguish as the frontal lobes myelinate and organize their function. B. Attention 1. Three types of attention a. Focused attention—seeking and finding an objective b. Sustained attention or vigilance—extended monitoring of an objective c. Divided attention—ability to perform two tasks simultaneously 2. Tests a. Trail making (connect the dots) i. Trails A—connect dots in simple numerical order (focused attention) ii. Trails B—connect dots with alternating sequence of numerical and alphabetical order (i.e., 1-A-2-B-3-C. . . .) (divided attention) iii. Scored based on time to perform each test and difference in performance between A and B b. Stroop test i. Reading of words on cards with increasingly difficult-to-ignore distractors ii. Most difficult is reporting the color in which a word representing a different color is printed (e.g., for the word “black” printed in green, the correct response is “green”) c. NB: Digit span: good bedside exam of attention i. Count backwards from 100 by 7, or 30 by 3 V. Memory A. Temporal categorization 1. Working memory: a temporary storehouse for recently acquired (within the past minute) information; managed by the frontal lobes; usually able to store about seven or eight “chunks” of information a. Digit span and reverse digit span b. Memory for designs c. “N-back” test 2. Recent memory: the collection of events over the past few minutes to hours a. Verbal memory: word lists (Hopkins Verbal Learning Test, Rey Auditory Verbal Learning Test) b. Visual memory: diagrams (Rey-Osterrieth Complex Figure) 3. Recent past memory: extends over the past few months; asking about recent events in the patient’s life or in the news is a useful test. 4. Remote memory: concerns events in the distant past a. Although preserved (relative to more recent memories) in dementias and amnesias, usually not intact B. Categorization by type of data 1. Episodic memory: the recall of specific events (e.g., what you ate for breakfast today) 2. Semantic memory: the storage of knowledge and facts (e.g., semantic memory is the storage of knowledge and facts) 3. Procedural or implicit memory: preservation of learned automatic skills (e.g., riding a bicycle) 4. Semantic and implicit memories do not deteriorate with normal aging; episodic memory may decline slightly because of age-related inefficiency of frontal processing. VI. Perceptual and Motor Performance A. Bender Visual Motor Gestalt 1. Originally developed to test cognitive maturity of children 2. Normal 12-year-old children can complete the test well. 3. Consists of nine simple diagrams, which are directly copied by the patient 4. Used to screen for cerebral dysfunction (sensitive, but nonspecific) B. Benton Facial Recognition Test 1. The patient is shown a head-on photograph of an unfamiliar face. 2. The patient is shown the same face photographed in different ways (changed lighting or angle) and scored on the number of previously presented faces he or she recognizes 3. Specific for posterior right-hemisphere lesions C. Hooper Visual Organization Test: subject names fragmented objects VII. Language Function A. Lengthy, comprehensive tests 1. Boston Diagnostic Aphasia Examination 2. Western Aphasia Battery 3. Porch Index of Communicative Ability B. Brief, but fairly complete: Reitan Aphasia Screening Test C. Specific tests 1. Token Test: verbal comprehension 2. Boston Naming Test: naming pictured objects 3. Peabody Picture Vocabulary Test: auditory comprehension VIII. Comprehensive Tests of Brain Function A. Halstead-Reitan Battery 1. Domains tested a. Tactile perception (stereognosis, manual dexterity, finger localization, graphesthesia, simultaneous tactile stimulation) b. Auditory perception (rhythm discrimination, speech-sounds test) c. Abstraction (categorization test) d. Aphasia screening (naming, speech sounds, body part identification) e. Attention (trail-making test, flickering light) f. Visual perception (flickering light) g. Dexterity and motor speed (finger oscillation) 2. Long, intense test procedure 3. Reliably identifies subjects with brain damage B. Luria-Nebraska Neuropsychological Battery 1. Tests broad range of cerebral function 2. Can localize dysfunction and identify particular disorders (i.e., sensitive and specific) 3. Can define hemispheric dominance
![]() NB:
NB:
![]() NB:
NB:
![]() NB:
NB:
![]() NB:
NB:
![]() NB:
NB:
![]() NB:
NB:
![]() NB:
NB:
![]() NB:
NB:
![]() NB:
NB:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






