Neurobehavioral Aspects of Traumatic Brain Injury in Children
Aleksandra Djukic
Introduction
The tragedy of traumatic brain injuries (TBIs) begins with its sudden onset and selection of victims, generally children and young adults who have an expectation of long life and unlimited possibilities. The tragedy then encompasses families, whose coping abilities are stretched to the limit, patients who only dimly understand why their lives must be changed in such dramatic ways, and a professional community, which is responsible for their recovery and reintegration (1).
The burden of TBI in children is heavy. Each year, approximately 475,000 children younger than 14 years sustain TBI (2). For 5,000 of them, the outcome is fatal. TBI takes the lives of 6 times more U.S. children than those who die of HIV/AIDS (3). Of TBI survivors, 30,000 remain permanently disabled (4).
During the first days to week after the injury, the main focus of medical and surgical intervention is stabilization of the patient. As acute medical care has improved, the number of survivors has increased. These patients place increased and specific demands on the medical and educational communities to address their disabilities, which are often “silent.”
Favorable initial physical recovery, which is usually quick, often leads to erroneous optimism based on assumptions that cognitive and behavioral recovery has been equally favorable. This misconception leads to the premature release of injured children to their prior, now inappropriate, school environments and other problems.
In reality, the acute TBI can become not only a chronic disease but also, because of the nature of development, a progressive one. Children grow out of certain disabilities caused by TBI but may grow into new ones. Functions that escaped damage by the impact can later pay the price of compensation for the recovery of those functions primarily damaged. To optimize long-term outcome, coordinated and lasting action by the medical, social, and educational communities is required.
Pathophysiology of TBI
Injury to the head can result in two categories of brain injuries: primary and secondary.
Primary injury occurs immediately after the impact and is related to instantaneous events caused directly by the blow. This injury results from tissue disruption that is
often permanent and constitutes one of the most important limiting factors for a full recovery.
often permanent and constitutes one of the most important limiting factors for a full recovery.
Secondary injuries are caused by a cascade of events triggered by the impact, such as vessel disruptions and hemorrhages, edema, seizures, increase in intracranial pressure, consequent decrease in the brain perfusion pressure, and brain shifts/herniations.
Mechanisms/Physics of the Primary Injury
The central event in any brain injury is movement of the brain within the skull (5). An understanding of the physics of TBI is a prerequisite for an understanding of the pathophysiology of brain injury, the basis of residual impairment, and possible treatment targets.
Two types of accelerating movement—linear and rotational—of the head and brain caused by the impact are pertinent. Each of them causes distinctive patterns of tissue damage (Fig. 13.1).
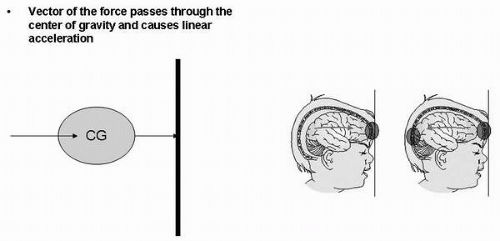
If the vector of the force passes through the center of gravity (CG) of the head, the head will assume linear acceleration along the direction of the force. All particles (cells) will travel with the same velocity and in the same direction: Hence they will sustain no intermolecular stress. As the accelerating head hits the ground, the skull suddenly decelerates, but the brain continues to move forward until it is stopped by one of the poles of the calvarium. This impact injures the brain at that pole and creates a negative pressure at the opposite one, which injures that pole of the brain (Fig. 13.2). Gyri, which are flat and have a large surface area, such as those in the frontal lobes, will be prone to extensive lesions. Injuries caused by the linear acceleration are mostly superficial (6).
 ▪ FIGURE 13.1. Linear acceleration causing crowding of the brain at the pole (coup) and creating negative pressure and cavitations at the antipole |
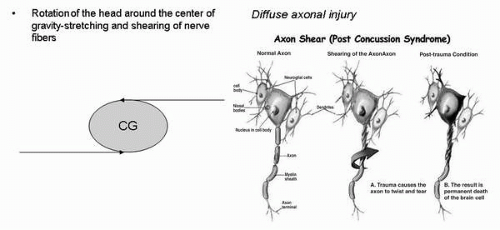
When the vector of the force does not pass through the CG of the head, the head will assume rotational acceleration. Whereas the effect of linear acceleration depends on pressure changes and the impact of the brain against bony structures, rotational mechanisms produce shearing strain. Shearing-strain forces distort the shape of the brain, cause intermolecular stress, and lead to tearing of neural elements (7). Injuries caused by rotational forces are deep. The abundance of white matter lesions throu ghout the brain, indicative of widespread axonal injury (disconnection syndromes), is a pathologic hallmark of severely injured patients (Fig. 13.3). Axonal injury has a predilection for the gray-white matter junction, cerebellar peduncles, corpus callosum, fornices, and fiber tracts around the brain stem (8,9).
Asynchrony between the rotational movements of the brain and skull causes rubbing of the friable cortex against the rough surfaces of the skull base. Temporal and frontal parts of the brain and cingulate gyri, which are adjacent to the most prominent dural surfaces, are particularly vulnerable to injury. This disruption correlates with impairments of memory, frontal lobe functions, and emotional control.
In reality, most TBIs are produced by the combination of the two accelerating movements.
Imaging
Various neuroimaging techniques offer pertinent information concerning the diagnosis, clinical outcome, and recovery mechanisms after pediatric TBI. The main advantage of the computerized tomography (CT) is its availability and ability to detect lesions rapidly that require immediate surgical intervention, such as epidural hematomas and fractures. Magnetic resonance imaging (MRI) has a higher sensitivity in detecting intraparenchymal injuries, especially those associated with diffuse axonal injury. Diffusion tensor imaging (DTI) provides a quantitative assessment of the integrity of white matter tissue.
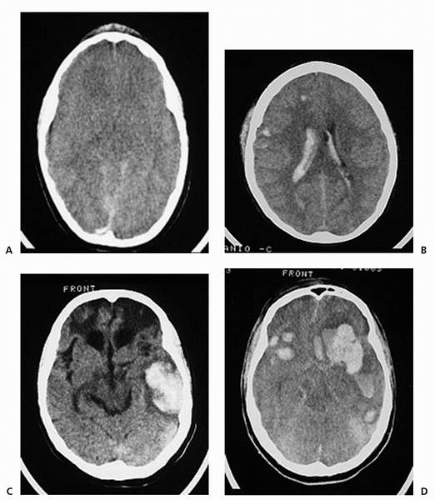 ▪ FIGURE 13.3. MRI findings. A: Diffuse swelling. B: Diffuse axonal injury. C, D: Frontotemporal contusions. |
Newer imaging techniques, such as functional MRI, which records blood oxygen level-dependent signal in conjunction with conventional imaging, may in the future enable the clinician to understand plasticity and recovery processes. It also may facilitate the design of early-intervention and rehabilitation programs for children with TBI (10, 11, 12).
Clinical Course of TBI
Immediately after the injury, children may lose consciousness and remain comatose. If not comatose, injured children may show confusion, disorientation, and amnesia (Fig. 13.4). After the resolution of coma, pediatric patients recovering from severe TBI enter a state of anterograde amnesia (13). Behaviors characteristic of this period are restlessness, impulsive behaviors alternating with lethargy, irritability, and agitation. Restoration of memory
for ongoing events is not a continuous process. Patients regain “islands of memory,” in which periods of confusion and amnesia alternate with those of good orientation. With time, lucid periods become longer and finally continuous. For confused TBI patients, the length of time elapsed until information is remembered on a day-to-day basis (i.e., the duration of post-traumatic amnesia) is a vital indicator of outcome (14).
for ongoing events is not a continuous process. Patients regain “islands of memory,” in which periods of confusion and amnesia alternate with those of good orientation. With time, lucid periods become longer and finally continuous. For confused TBI patients, the length of time elapsed until information is remembered on a day-to-day basis (i.e., the duration of post-traumatic amnesia) is a vital indicator of outcome (14).
 ▪ FIGURE 13.4. Restoration of cognitive functions after severe TBI. RGA, retrograde amnesia; PTA, post-traumatic, anterograde amnesia. |
Examples of different course scenarios in brain-injured patients who do not fully recover are the following:
1. There is gradual improvement of neurological functions, which is most prominent during the first months after injury but continues at a slower pace, especially with regard to cognitive recovery, which can occur over years.
2. Consequences become apparent after a delay. Damage to some areas of the brain, particularly the frontal lobes, in early childhood may not give rise to major problems until early or late adolescence, when normal maturation fails to occur (15,16).
3. Developmental functions that were not primarily injured eventually pay the price for the recovery of the injured functions. For example, young children who have injury to their language areas recover better than both older children and adults. In these young patients, “vicarious” areas of the contralateral hemisphere assume the functions of the damaged areas. However, these newly created and unnatural tasks eventually lead to overcrowding of the neural networks within the uninjured hemisphere. In addition to developing visuospatial skills, the nondominant hemisphere then becomes burdened with the task of organizing language. For example, visuospatial functions suffer as language functions recover (17,18).
Classification of TBI
The depth and duration of coma and length of time that children remain amnestic reflect the severity of brain damage. TBI is most often classified as mild, moderate, or severe, based on the Glasgow Coma Score (GCS) at presentation (Table 13.1) (19,20). A GCS of 13 to 15 defines mild TBI; 9 to 12, moderate TBI; and 8 or less, severe TBI. Although the GCS is a useful tool for the initial management, it has not been found to be an accurate predictor of cognitive outcome in children (21,22). For this purpose and for the prediction of residual deficits, especially those of interest to child psychiatrists, the duration of post-traumatic amnesia (PTA) is a more valuable index. As a rough guide, children with a GCS of 12 or below, those who have lost consciousness for more than 20 to 30 minutes, or those who have PTA of longer than 7 days are more likely to have psychological sequelae. These are children with moderate or severe injuries. This degree of brain injury warrants hospital admission and close medical surveillance after discharge. This group of patients might be of specific interest to child psychiatrists because it typically consists of
children with pre-existing behavioral problems that worsen after the injury. These children are prone to recurrent injuries (23). Sports and bicycle accidents account for the majority of cases among 5- to 14-year-old children. Every attempt to reduce the likelihood of recurrent injury should be made because repeated TBIs may have an additive effect and lead to cognitive decline (24).
children with pre-existing behavioral problems that worsen after the injury. These children are prone to recurrent injuries (23). Sports and bicycle accidents account for the majority of cases among 5- to 14-year-old children. Every attempt to reduce the likelihood of recurrent injury should be made because repeated TBIs may have an additive effect and lead to cognitive decline (24).
TABLE 13.1. GLASGOW COMA SCORE | |||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Immaturity of the Brain: Opportunities and Vulnerabilities
It was previously thought that infants would suffer minimal damage from TBI because of greater brain plasticity. Classic studies by Kennard (25,26) showed that the immaturity of the brain has a protective role regarding outcome. Optimistic clinical expectations that followed are summarized in the statement “It is better to have your injury early, if you can manage it” (27).
This concept has been challenged. Young children may be especially vulnerable to the diffuse nature of TBI and tend to have more global and profound consequences than do older children (28,29). Depending on the child’s age, the same injury can lead to very different functional outcomes. A review of evidence for and against the argument that younger people show better recovery after brain injury can be found in Wilson (30).
In the report from the Traumatic Coma Data Bank, children younger than 4 years exhibited the poorest outcomes (28). The two main reasons for these observations are related to the nature of the injury and the specific tasks children encounter.
Because of the diffuse nature of rotational forces, all severe head injuries should be considered diffuse from the pathophysiological standpoint. The diffuse nature of injury associated with rotational forces decreases the ability of distant areas and surrounding areas to compensate (31).
With regard to the nature of the task, although adults may function well by relying on previously acquired knowledge, children cannot, because functions emerging at the time of TBI may suffer more than established ones (32). Thus depending of the developmental stage at the time of the injury, the same insult might have different outcomes (Table 13.2).
TABLE 13.2. PROGNOSTIC FACTORS RELEVANT FOR RECOVERY | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
According to Wilson (33), it is not only the kind of head injury that matters but also “the kind of head.”
Neurobehavioral Outcome
Behavioral and cognitive problems as well as difficulties in adaptive functioning are common after TBI (34,35). Outcomes range from almost complete recovery to profound deficits that affect both the child and the family. Injury causes not only a direct loss of brain function but also indirect dysfunction. Sequelae develop as a result of emotional response to injury, exacerbation of pre-existing problems, and the fact that injured children have difficulty meeting the expectations of their peers.
Post-traumatic epilepsy is a serious clinical problem that can worsen functional outcome. The incidence of post-traumatic seizures ranges from 2% to 35%, with higher frequencies seen with more severe injury. The incidence of seizures after mild head injuries is not significantly greater than that in the general population. The seizure focus in 56% of patients is temporal, and in 36% of patients, frontal. Unfortunately, no efficacious preventive therapy for post-traumatic epilepsy has been established. Prophylactic use of antiepileptic drugs does not prevent post-traumatic epilepsy and may produce negative cognitive effects (36).
The incidence of psychiatric disorders is twice as high in children with TBI as in those with physical handicaps without cerebral involvement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree