
Neuroendovascular Diseases: Past, Present, and Future
Objectives: Upon completion of this chapter, the reader should be able to explain the current state of the endovascular industry and report how evolving endovascular technologies might impact aneurysm and ischemic stroke management in the future.
Accreditation: The AANS* is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to sponsor continuing medical education for physicians.
Credit: The AANS designates this educational activity for a maximum of 15 credits in Category 1 credit toward the AMA Physician’s Recognition Award. Each physician should claim only those hours of credit that he/she spent in the educational activity.
The Home Study Examination is online on the AANS Web site at: http://www.aans.org/education/books/controversy.asp
* The acronym AANS refers to both the American Association of Neurological Surgeons and the American Association of Neurosurgeons.
The field of neurointerventional medicine in the United States has experienced rapid growth over the past decade. In 2002, nearly 20,000 endovascular procedures were performed in the United States. This number is projected to increase to more than 50,000 over the next 5 years (Fig. 5-1).
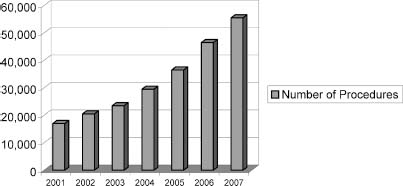
FIGURE 5-1 The projected growth rate in neuroendovascular procedures. From Boston Scientific Data and Estimates, Natick, MA. Reprinted by permission.
Some of the same foundations that have revolutionized the field of interventional cardiology are the basis for the success of neuroendovascular procedures—a reliance on a technology-based, less-invasive approach to the treatment of a complex set of diseases. Technology generates solutions to clinical needs in a dynamic and fast-paced fashion, and the less-invasive nature of the therapy permits lower rates of procedural morbidity, shorter lengths of stay, and quicker recovery times. Just as interventional cardiology has become the preferred procedural treatment for the heart, within the next 5 years neuroendovascular procedures will be used in the majority of all therapeutic neurovascular cases.
While the advantages of a technology-driven, less-invasive therapy are the main drivers of neuroendovascular therapy’s success, several other factors have helped and will continue to help fuel its growth. First, enough physicians have attended neuroendovascular training programs to keep pace with the expanding number of procedures. Second, clinical data and research comparing surgical and neuroendovascular treatment of aneurysms has helped demonstrate some of the advantages of the less-invasive approach and persuaded patients and physicians to use the procedure. The next generation of research in this area is underway and could provide conclusive, level-one evidence that neuroendovascular therapy should be the front-line aneurysm treatment. In addition, this research and other research on the impact of hospital volume on aneurysm treatment outcomes could help centralize care into centers specializing in neuroendovascular therapy. Finally, the ischemic stroke market will be a significant accelerant of case growth. This market is large, presenting an urgent need for an effective treatment; and neuroendovascular approaches offer significant promise in this regard.
In this chapter we attempt to capture the current state of neuroendovascular treatments in the United States and project the possible development of this field in the next 5 years. Neuroendovascular procedures include the treatment of aneurysms, AVMs, ischemic disease and various embolization procedures for conditions like fistulas and menenginomas. We will focus on the two primary areas of growth—aneurysms and ischemic disease above the carotid bifurcation.
 Market Infrastructure Supports the Neuroendovascular Market
Market Infrastructure Supports the Neuroendovascular Market
Neuroendovascular approaches to vascular disease have made significant inroads against traditional surgical treatments. In 1996, there were fewer than 1000 endovascular aneurysm treatments in the United States. By 2004, that number had increased to over 11,000 cases (Fig. 5-2). Endovascular treatment of aneurysms now accounts for over 50% of treated cases, and overall there were ~18,000 neuroendovascular procedures in the United States in 2002.
Structurally the market has responded to the demand for neuroendovascular services. The number of physicians able to perform neuroendovascular procedures has increased substantially since 1995. Physician training should continue to keep pace with demand. The number of fellowship-trained neuroendovascular physicians practicing in the United States is projected to be 475 by 2007 (Fig. 5-3).
The number of hospitals with neuroendovascular services has dramatically increased over the past 8 years. The total number of hospitals performing neuroendovascular procedures (all types) will increase moderately in the next 5 years; it is likely that existing centers will be treating a much larger number of patients (Fig. 5-4). The creation of Neurovascular Centers of Excellence, focused on clinical excellence and protocol-driven patient care in all diagnostic and therapeutic approaches directed specifically at neurovascular diseases, will contribute to the centralization of cases at the best and biggest neurovascular centers.
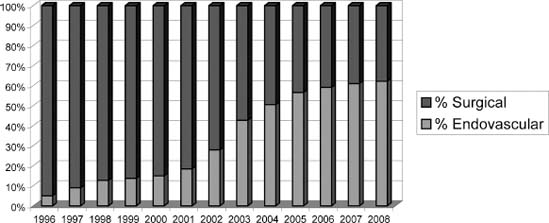
FIGURE 5-2 The projected growth rate in aneurysm treatments in the United States. From Boston Scientific Data and Estimates, Natick, MA. Reprinted by permission.
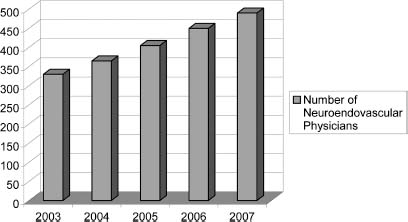
FIGURE 5-3 The projected growth rate in the number of neuroendovascular physicians. From Boston Scientific Data and Estimates, Natick, MA. Reprinted by permission.
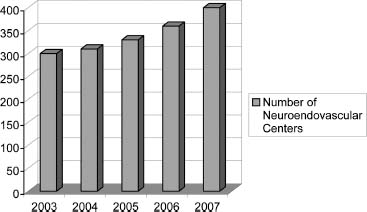
FIGURE 5-4 The projected growth rate in the number of neuroendovascular centers. From Boston Scientific Data and Estimates, Natick, MA. Reprinted by permission.
 Outcomes Research Demonstrates Clinical Profile
Outcomes Research Demonstrates Clinical Profile
Endovascular therapy developed because of technology’s ability to fit devices into small tubes and navigate them through the vasculature. This approach allows diseased vessels in the head to be accessed through a small incision in the groin. The trauma to patients is significantly less than that involved in a craniotomy—an advantage well understood by patients. Patients with unruptured aneurysms, who typically have time to consider treatment options, opt for endovascular therapy at a higher rate than do patients with ruptured aneurysms, who usually rely on the recommendation of the treating surgeon.
Research comparing the short-term outcomes of neuroendovascular treatment of aneurysms with surgical results has helped document what is intuitively obvious— that endovascular therapy should offer shorter lengths of stay, lower procedural morbidity, and shorter recovery time. Claiborne Johnston’s research has played an important role in legitimizing the endovascular treatment of aneurysms. Johnston compared outcomes for surgical and endovascular cases at the University of California, San Francisco (UCSF), in a retrospective double-blind study of unruptured aneurysms. The study found significantly less morbidity and a much shorter recovery time for patients treated endovascularly.1 A retrospective database analysis of unruptured aneurysms treated at university hospitals across the country found better outcomes associated with the endovascular approach.2 Johnston conducted a similar database analysis of unruptured aneurysms in California and found significantly lower rates of morbidity for patients undergoing endovascular therapy.3
Although these studies have not provided level I evidence, the careful methods involved and the consistent findings demonstrating that neuroendovascular aneurysm treatment has less short-term morbidity have been extremely persuasive. It is has been conceded that this approach is superior to surgery in terms of procedural morbidity and patient recovery, and the debate has shifted to whether neuroendovascular treatment is durable as well.3A
 Technological Innovation Expands Treatment Applications
Technological Innovation Expands Treatment Applications
The technological basis of endovascular therapy also generates benefits for physicians interested in “pushing the envelope” of treatment options. Technology often advances faster than human manual skills in treating difficult features of the human anatomy; technological innovations can compensate for skill limitations. The FDA clearance of Guglielmi Detachable Coils (GDC) in late 1995 opened the floodgates to a wave of technology development and innovation. Most of the early tools used in neuroendovascular treatments were borrowed technologies from either the interventional cardiology or peripheral vascular fields. In the past decade, numerous companies or divisions of larger companies have focused specifically on the design and development of tools for the neuroendovascular field. The major technological advancements over the past decade have been aimed at developing tools that overcome the tortuosity of the intracranial vasculature and developing coils suited for more difficult aneurysm morphologies in order to improve treatment efficacy.
The development of microguidewires with enhanced durability and steering ability has allowed physicians to reach intracranial vessels in a safe manner and to avoid multiple wire exchanges. The first decade of neuro interventional procedures saw rapid microguidewire development. Guidewires made of more durable materials, with better hydrophilic coatings and equipped with tips that could be more easily shaped, were introduced. Since then, newer materials and enhanced design and manufacturing techniques have improved these early technologies. Braided microcatheters and guiding catheters provide a level of support and luminal integrity that allows therapeutic tools to be delivered through microcatheters with internal lumens as small as 0.015 inches. The enhanced malleability of microcatheters has also added a level of stability not available in prior microcatheters.
Today’s neuroendovascular physician can choose between more than 20 different varieties and makes of microcatheters and guidewires. In 2005, eight new guidewires and microcatheters were introduced into the U.S. market.
The detachable coil market has experienced major change and innovation over the past 5 years. At last count, there are seven different companies marketing endovascular coils to neuroendovascular physicians around the world. The major advancements in basic coil technology include softer coils, two-dimensional coils, three-dimensional or complex-shaped coils, stretch-resistant coils, ultrasoft stretch-resistant coils, and second-generation “coated” coils.
 What Will Drive the Growth of Neuroendovascular Procedures?
What Will Drive the Growth of Neuroendovascular Procedures?
The increase in neuroendovascular procedures has been meteoric, and the projections suggest that these procedures will soon become the first-line treatment for some diseases. Figure 5-2 displays the estimate of penetration rates for endovascular treatment of aneurysms versus surgical treatment. Future projections include an assumption that endovascular aneurysm cases grow at 10%. This growth rate suggests that in 2008 endovascular aneurysms will represent about 60% of all treated intracranial aneurysms in the United States.
These projections may seem ambitious; however, the key elements to support this growth are already in place or are on the horizon. First, the physician and hospital infrastructure required to support this caseload is growing at a pace that will easily allow it to deliver these services. Second, technology is continuing to improve to meet unmet clinical needs. Third, accumulating clinical evidence combined with institutional changes in the delivery of care have the potential to change treatment and referral patterns so that care is concentrated in highvolume centers of excellence that offer endovascular services. Finally, it will be the implementation of neuroendovascular treatment in cases of ischemic stroke that will drive its growth as the treatment of choice.
 Market Infrastructure Will Continue to Meet Demand
Market Infrastructure Will Continue to Meet Demand
In simple terms a 70% penetration rate would result in 13,000 neuroendovascular treatments of intracranial aneurysms in 2008. The total projected case volume per hospital is given in Figure 5-5. The total aneurysm case volume per neuroendovascular physician is shown in Figure 5-6. Currently, there are ~400 practicing (mostly fellowship-trained) neuroendovascular specialists in the United States. In 2004, U.S. training centers produced 35 graduating fellows. Assuming the number of fellowship programs continues to grow in response to the demand for training, by 2007 there will be almost 500 fellowship-trained neuroendovascular specialists practicing in the United States; neuroendovascular physicians’ caseloads then would average only 27 aneurysm cases per year.
 Innovations Are Allowing More Aneurysms to Be Treated
Innovations Are Allowing More Aneurysms to Be Treated
Achieving 70% aneurysm penetration will require neuroendovascular therapy to treat a wider array of aneurysm morphologies.
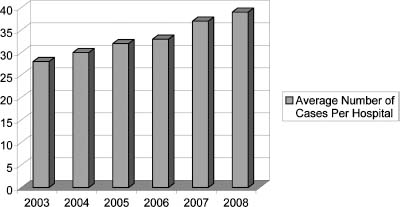
FIGURE 5-5 The projected growth rate in the number of endovascular aneurysm cases per U.S. center (300 neuroendovascular hospitals in 2003, growing to 340 in 2008).



