affect certain body part functions. Usually pain is the result of the injury, with some limitation in neck movement.
Temporomandibular joint disorder
Nerve damage
Mechanism of injury identifies acceleration-deceleration action
Pain initially minimal but increases 12 to 72 hours after the accident
Dizziness
Headache
Back pain
Shoulder pain
Vision disturbances
Tinnitus
Neck muscle asymmetry
Reduced neck mobility
Gait disturbances
Rigidity or numbness in the arms
Tenderness at the exact location of the injury
Decreased active and passive range of motion
Full cervical spine X-rays rule out cervical fracture.
Until X-rays rule out cervical fracture, treatment focuses on protecting the cervical spine through immobilization. After cervical spine injury has been ruled out, initial treatment includes limited activity during the first 72 hours after the injury, use of a soft cervical collar, and application of ice packs. (See Using a cervical collar.) Oral analgesics provide pain relief, and oral corticosteroids help reduce inflammation and relieve chronic discomfort. To restore flexibility,
physical therapy, including mobilization exercises, is started 72 hours after the injury. It’s combined with the application of moist heat and a gradually decreased use of the soft collar.
If the patient experiences persistent ligamentous or articular pain, he may benefit from cervical traction and diathermy treatment. Surgical stabilization may be necessary with severe cervical acceleration-deceleration injury.
Maintain spinal immobilization until cervical X-rays are evaluated.
Protect the patient’s spine during all care.
Give prescribed drugs.
Apply a soft cervical collar.
Monitor pain level, administer analgesics as ordered, and evaluate response to medications.
Observe for signs and symptoms of complications.
Assess the patient’s neurologic status per facility protocol and clinical status.
 TEACHING THE PATIENT WITH AN ACCELERATION-DECELERATION INJURY
TEACHING THE PATIENT WITH AN ACCELERATION-DECELERATION INJURY
the disorder and its implications
medication administration, dosage, and possible adverse effects, and when to notify the physician
how to apply a soft cervical collar correctly
activity restrictions
signs and symptoms of complications
the importance of follow-up care
the benefit of available community support groups.
Provide appropriate education to the patient before discharge. (See Teaching the patient with an acceleration-deceleration injury.)
and primary infections of the spinal cord itself, such as syphilis or acute disseminated encephalomyelitis. Acute transverse myelitis may also accompany demyelinating diseases, such as acute multiple sclerosis, and inflammatory and necrotizing disorders of the spinal cord such as hematomyelia.
Shock
Motor impairment
Sensory impairment
Sensory or motor dysfunction, depending on the site of damage to the spinal cord
Rapid onset with motor and sensory dysfunctions below the level of spinal cord damage appearing in 1 to 2 days
Flaccid paralysis of the legs (sometimes beginning in just one leg) with loss of sensory and sphincter functions; may follow pain in the legs or trunk
Absent reflexes in early stages but possibly reappearing in later stages
Extent of damage dependent on level of the spinal cord affected; transverse myelitis seldom involving the arms; with severe spinal cord damage, shock possible (hypotension and hypothermia)
Neurologic examination confirms paraplegia or neurologic deficit below the level of the spinal cord lesion and absent (or, in later stages) hyperactive reflexes.
Cerebrospinal fluid may be normal or show increased lymphocytes or elevated protein levels.
Magnetic resonance imaging rules out spinal cord tumor.
Culture specimens identify the cause of any underlying infection.
Monitor vital signs. Watch carefully for signs of spinal shock (hypotension and excessive sweating).
 TEACHING THE PATIENT WITH MYELITIS
TEACHING THE PATIENT WITH MYELITIS
the disorder and its implications
medication administration, dosage, and possible adverse effects, and when to notify the physician
when to report changes in mental status, level of consciousness, or motor ability
types of therapy that may be beneficial, such as physical therapy, occupational therapy, or counseling
the importance of maintaining adequate nutrition
bowel and bladder training
exercises to maintain or improve muscle tone and function
signs and symptoms of complications
the importance of follow-up care
the benefit of utilizing available community support groups such as the local chapter of the Transverse Myelitis Association.
Assist with range-of-motion exercises and proper body alignment.
Reposition the patient every 2 hours, assess his skin condition, and provide appropriate skin care.
Monitor intake and output.
Initiate rehabilitation immediately. Assist the patient with physical therapy, bowel and bladder training, and lifestyle changes that his condition requires.
Provide appropriate education to the patient and his family before discharge. (See Teaching the patient with myelitis.)
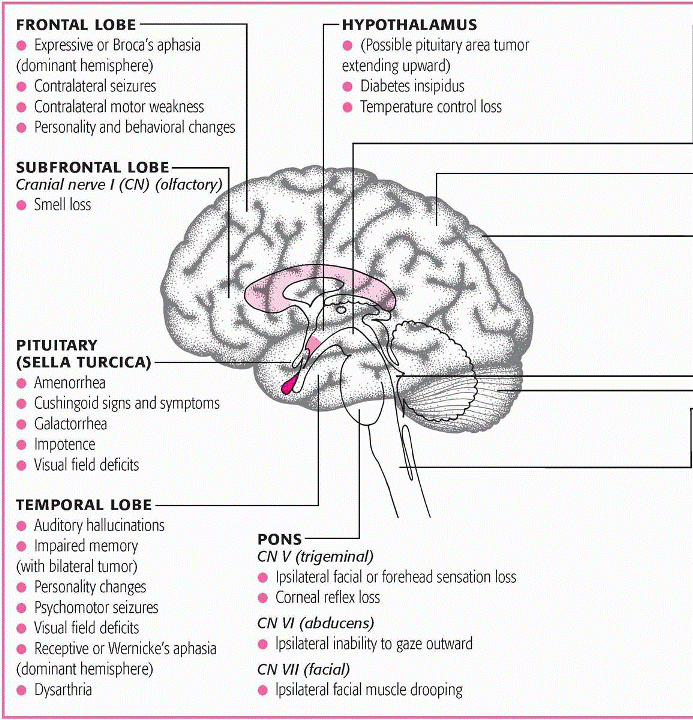
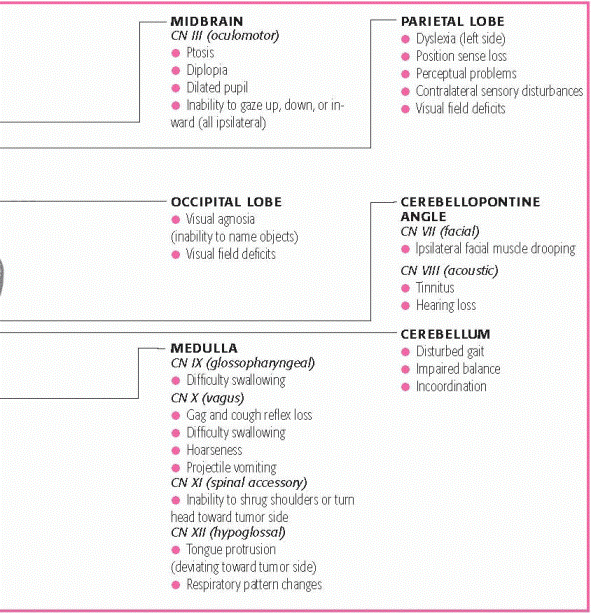
adults, the most common tumor types are gliomas and meningiomas, which usually occur above the covering of the cerebellum, or supratentorial tumors. In children, the most common tumor types are astrocytomas, medulloblastomas, ependymomas, and brain stem gliomas. The exact cause unknown, but risk factors include preexisting cancer, radiation or chemical exposure, and head trauma.
Radiation encephalopathy
Cerebral edema
Seizures
Neurologic deficits
Hydrocephalus
Brain herniation
Coma
Respiratory or cardiac arrest
Brain herniation
Headache
Nausea and vomiting
Signs and symptoms of increased ICP
Vision disturbances
Weakness, paralysis
Aphasia, dysphagia
Ataxia, incoordination
Skull X-rays confirm tumor.
Brain scan confirms tumor.
Computed tomography scan confirms tumor.
Magnetic resonance imaging evaluates tumor location, size, and vascularity and cerebral edema.
Cerebral angiography confirms tumor.
Positron emission tomography confirms tumor.
Tissue biopsy confirms the type of tumor.
Lumbar puncture may show increased cerebrospinal fluid (CSF) pressure, which reflects ICP, increased protein levels, decreased glucose levels and, occasionally, tumor cells in CSF.
(CeeNU), or procarbazine (Matulane) with radiation therapy is more effective than radiation alone.
|
|
TUMOR AND CHARACTERISTICS | ASSESSMENT FINDINGS |
|---|---|
GLIOBLASTOMA MULTIFORME (SPONGIOBLASTOMA MULTIFORME) | |
| GENERAL
LOCALIZING
|
ASTROCYTOMA | |
| GENERAL
LOCALIZING
|
OLIGODENDROGLIOMA | |
| GENERAL
LOCALIZING
|
EPENDYMOMA | |
| GENERAL
|
MEDULLOBLASTOMA | |
| GENERAL
LOCALIZING
|
MENINGIOMA | |
| GENERAL
LOCALIZING
|
SCHWANNOMA (ACOUSTIC NEUROMA, NEURILEMOMA, CEREBELLOPONTINE ANGLE TUMOR) | |
| GENERAL
LOCALIZING
|
nerve. Although schwannomas are moderately radioresistant, treatment still calls for postoperative radiation therapy.
 TEACHING THE PATIENT WITH A MALIGNANT BRAIN TUMOR
TEACHING THE PATIENT WITH A MALIGNANT BRAIN TUMOR
the disorder and its implications
medication administration, dosage, and possible adverse effects, and when to notify the physician
the importance of good nutrition
signs of infection or bleeding that may result from chemotherapy
adverse effects of chemotherapy and other treatments and actions that may alleviate them
physical and cognitive limitations that may occur
seizure precautions
early signs of tumor recurrence
wound care
types of therapy that would be beneficial, such as physical therapy, speech therapy, and occupational therapy
signs and symptoms of complications, espically increased intracranial pressure and infection
information regarding end-of-life care, such as advance directives and hospice
the importance of follow-up care
the benefit of available community support groups such as the local chapter of the National Brain Tumor Foundation.
Maintain a patent airway.
Document the occurrence, nature, and duration of seizure activity.
Take steps to protect the patient’s safety.
Give prescribed drugs and note any adverse reactions.
Monitor for changes in the patient’s neurologic status and observe for signs of increased ICP.
Monitor vital signs and pulse oximetry. Note changes in respiratory status and temperature.
After supratentorial craniotomy, elevate the head of the bed about 30 degrees.
After infratentorial craniotomy, keep the patient flat for 48 hours.
Monitor ICP and cerebral perfusion pressures, and provide measures to maintain adequate readings.
Monitor head dressings and provide wound care.
As appropriate, instruct the patient to avoid Valsalva’s maneuver and isometric muscle contractions when moving or sitting up in bed.
Consult with occupational, speech, and physical therapists.
Provide emotional support to the patient and his family. Encourage them to talk about their concerns. Listen carefully and answer their questions honestly and completely.
Provide appropraite education to the patient and his family before discharge. (See Teaching the patient with a malignant brain tumor.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree