Condition
Percentage of neurological deficit
Cervical disc prolapse
0.07
Myelopathy
1.38
Thoracic myelopathy
5.59
Lumbar disc prolapse
0.38
Lumbar canal stenosis
0.63
Deformity
2.25
Spinal osteotomies are inherently high-risk surgeries for neurological deficit, and the incidence varies from 0.06 to 11 % depending upon the series and the nature of osteotomy (Table 19.2). It is mandatory that the possibility of a postoperative deficit is discussed with the patient in every case. Intraoperative spinal cord monitoring must also be utilised to identify any untoward cord accident at the earliest possible, as early identification and immediate action can result in reversal of the deficit.
The reason for a neurological deficit is sometimes obvious but many times not (Fig. 19.1). Spinal osteotomies are complex surgical procedures which can cause neurological deficit in many different mechanisms. Inadvertent placement of the implants is a well-known cause for neurological deficit. Although the injury due to intracanal placement of screws and wires is ever present in any spine surgery, this risk is more in patients requiring osteotomy due to the presence of three-dimensional deformity and different pedicle orientations at each segment of the deformed segments (Fig. 19.2). The process of correcting the deformity involves mobilisation and distraction of the cord, which can either cause a direct neurological deficit or compromise the vascular supply to the cord. Intraoperatively, the laminae at the margins of the decompression, especially the lower border of the upper laminae, can compress the cord during correction. Any movement or mobilisation of the dura can also compromise the blood supply and result in deficit.
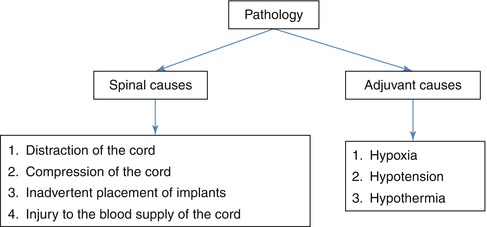

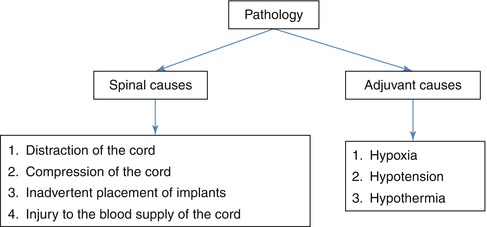
Fig. 19.1
Common causes for neurological deficit in spinal osteotomies

Fig. 19.2
Severe congenital kyphoscoliotic deformity. Note that each vertebral segment is in different orientation
19.2 Blood Supply to the Spinal Cord
The main blood supply to the spinal cord is derived from the anterior spinal trunk and a pair of posterior spinal arteries. These arterial trunks are further reinforced by the segmental arteries arising from vertebral arteries in the neck and aorta in thoracic and lumbar spine. The segmental arteries divide into multiple branches at the level of intervertebral foramen and have anastomotic connection with adjoining levels. The second network of anastomoses occurs within the spinal canal. So, whenever ligation of a segmental vessel is necessary, it is preferable to do it away from the neural foramen so as not to interfere with the anastomoses (Fig. 19.3).
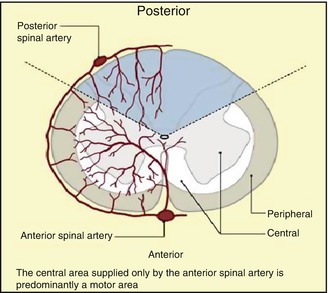
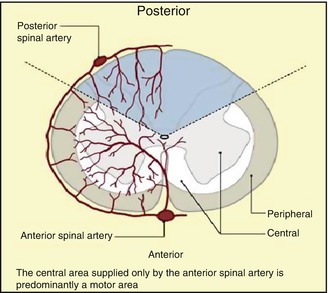
Fig. 19.3
Cross section of the spinal cord and distribution of blood supply (Reprint with permission from Stephen and Caroline [22])
When compared to other regions, the thoracic cord has the least blood supply. There is a large medullary feeder, the artery of Adamkiewicz, which usually arises on the left side at any segment between T6 and T9 segments and reinforces the blood supply to the thoracic cord. There is still lack of clarity on the deleterious effects of ligating the segmental vessels and artery of Adamkiewicz. However, it is preferable to avoid ligation of segmental vessels whenever possible.
Kato and Kawaraha et al. [3] studied in a dog model the effect of spinal cord blood flow secondary to interruption of segmental vessels which supply the artery of Adamkiewicz. They found that ligation of more than four consecutive segmental arteries which supply the artery of Adamkiewicz can cause interruption of spinal cord blood flow. Murakami and Tomito et al. [4] reported that interruption of artery of Adamkiewicz may not always end in neurological deficit. In their retrospective study, in 15 patients out of 180 who underwent total en bloc spondylectomy, when the artery of Adamkiewicz had to be resected, none of the patients had neurological deterioration. In their experience, sacrificing even up to three pairs of segmental vessels did not cause neurological deterioration.
Most osteotomies will result in spinal column shortening to variable extent. Ji et al. [5] had studied the effect of spinal cord shortening over the spinal cord blood flow in a canine model. Shortening of the spinal cord up to half of the vertebral body caused reversible changes in SSEP. They noticed temporary increase in spinal cord blood flow when the shortening is up to two-thirds of the vertebral segment. But the blood flow progressively decreased when the shortening exceeded more than two-thirds of the vertebral segment. Kawahara et al. [6] studied the effect of spinal cord shortening in a dog model. They divided the shortening into three phases. Phase 1 – safe range, shortening up to one-third of the vertebral segment; phase 2 – warning range, shortening of one-third to two-thirds of the vertebral segment; and phase 3 – dangerous range, shortening more than two-thirds of the vertebral segment.
Neurological deficit ranges from 0.06 to 11 % and is often partial. There are some clinical types of partial neurological deficit that are commonly encountered with spinal trauma; still they can occur after deformity corrective surgery.
1.
Central cord syndrome
The centrally placed proximal fibres are more involved than the distal fibres. Recovery will be good. About 50 % of the patients will have normal bladder and bowel function. This type of syndrome may occur in cervicothoracic deformity correction.
2.
Brown-Sequard’s syndrome
This syndrome occurs due to hemisection of the cord and occurs rarely after spinal osteotomy. There will be ipsilateral motor weakness and contralateral loss of pain and temperature sensation. Recovery is often good. Nearly all patients will obtain ambulatory power and bladder function.
3.
Anterior spinal cord syndrome
Anterior spinal cord syndrome can occur due to stretching of anterior spinal artery after osteotomy closure. There will be complete motor loss, loss of pain, and temperature sensation. The posterior column will be preserved. Significant recovery rarely occurs in this syndrome.
4.
Posterior spinal cord syndrome
This syndrome is relatively rare and can occur due to impingement by bone or ligamentum flavum from posterior aspect. There will be loss of position and vibratory sense. Other sensations and motor function are preserved.
5.
Cauda equina syndrome
Cauda equina syndrome occurs due to injury to nerve roots below the conus medullaris. It is characterised by asymmetric loss of motor function, loss of sensation, and areflexia. In complete cauda equine syndrome there will be loss of bladder and bowel function. Usually it presents as incomplete pattern.
6.
Conus medullaris syndrome
It occurs due to injury to sacral cord and adjacent nerve roots. Loss of bladder, bowel function and perineal muscle weakness will occur. There may be involvement of adjacent nerve roots causing various amounts of lower limb muscle weakness.
7.
Mixed syndromes
This is combination of above-mentioned injuries patterns and it is only rarely found in clinical practice.
19.3 Preoperative Causes
It is important to understand that certain preoperative conditions are more prone for postoperative neurological deficits. Also, it is important that these are identified by thorough clinical and radiological investigations, so that appropriate counselling and intraoperative preventive measures can be taken. Although MRI is generally performed before all surgeries requiring osteotomy, it is however mandatory in patients with congenital scoliosis, atypical curves and revision spine surgeries. There are specific conditions which are associated with high incidences of post-op neurological deficits. Deformities with hyperkyphosis, acute kyphosis, rigid deformities, neurofibromatosis, spinal dysplastic conditions, and congenital spinal cord anomalies are prone for neurological deficits. Kyphosis associated with neurofibromatosis, achondroplacia, and mucopolysaccharidosis is usually an acute deformity. So the chance of neural deficit is high with these conditions (Table 19.3).
Table 19.3
Conditions associated with increased risk of neurological deficit
Conditions associated with increased neurological deficit |
|---|
1. Deformities with hyperkyphosis |
2. Acute kyphosis |
3. Severe kyphosis |
4. Rigid kyphosis
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





