Neurology and psychiatry
Many neurological conditions may present with cognitive impairment or psychiatric symptoms. Those conditions which are usually dealt with by neurologists or neuropsychiatrists are discussed below. Those which are usually dealt with by old age psychiatrists (i.e. Alzheimer’s disease, vascular dementia, Lewy body disease and Pick’s disease) are discussed on pages 90–91, along with a description of the management of dementia. The principles of management discussed on page 91 are just as applicable to the causes of dementia described below
Creutzfeldt–Jakob disease (CJD)
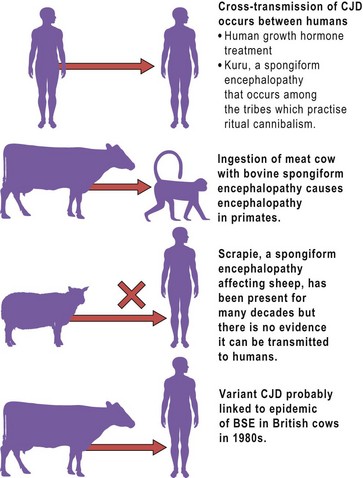
This rare infective form of dementia is the most common human form of the spongiform encephalopathies, so-called because of the sponge-like appearance of the brain at postmortem. It is caused by transmission of an abnormal prion protein that is found in plaques in the brain of affected cases. The risk of contracting CJD is thought to depend on the extent of exposure to the abnormal prion protein and genetic susceptibility factors in the exposed person. Following infection, it may be several decades before dementia develops, as evidenced by the adult-onset of dementia in people who had been treated with contaminated human growth hormone during childhood. Variant CJD (vCJD) is a new disorder, first described in 1996, and is strongly linked to exposure to beef products that have been infected with bovine spongiform encephalopathy (BSE). Some of the issues concerning transmission of CJD and other spongiform encephalopathies are summarised in Figure 1.
Parkinson’s disease
Depression occurs in up to 40% of cases of Parkinson’s disease. This is a higher rate than in conditions that cause a similar amount of disability, suggesting that changes in brain structure or function contribute to the depression. There is also a raised risk of dementia in patients with Parkinson’s disease, with many cases probably caused by Lewy body disease (p. 90).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree