Classical executive function tests
The most frequent classical executive function tests used in patients with bvFTD are: the backward digit span [5], Letters and Numbers [5], word fluency tests; design fluency tests [40], Trail Making Test Part B [7], Wisconsin Card Sorting Test [41], Tower Tests [42], Hayling Test [43], D-KEFS (The Delis–Kaplan Executive Function System) [44], among others.
- Backward digit span:
Participants are presented with sequences ranging from two to eight digits in length and are asked to repeat the digits in the reverse order. This task assesses mental manipulation and working memory. It is expected that bvFTD patients exhibit deficits in these types of tasks especially in mild and moderate stages of the disease.
- Letters and Numbers:
Participants are presented with an increasing number of letters and digits and are asked to repeat them in a way such that numbers are ordered in an ascending fashion and letters arranged alphabetically. This test also assesses mental manipulation. Studies by our group looking at executive measures in bvFTD patients showed that early high functioning bvFTD patients had significantly lower scores than normal controls in this test [9].
- Word fluency tests:
The purpose of these tests is to assess spontaneous production of words beginning with a given letter or of a given semantic class in a limited amount of time. For letter fluency (phonetic association), participants were asked to verbally produce as many words as possible beginning with a given letter for 60 seconds (“F”, “A,” or “S”). For category (semantic association) fluency, participants were asked to produce as many animal nouns as possible within the same time frame. Performance on verbal fluency tasks is one of the most frequently noted means of discriminating between AD and FTD clinically, and even among FTD subtypes [45]. FTD patients tend to generate less words beginning with a specific letter in comparison to the total of words generated with a given semantic category (animals). Also, FTD patients in general (and bvFTD patients in particular) showed more generation of “bad words” during letter fluency testing [46] and have more trouble in action fluency [47] in comparison to AD patients.
- Trail Making Test Part B:
Participants were asked to join 25 randomly arranged numbers and letters in an alternating fashion. These tests are designed to assess speed of attention, sequencing, mental flexibility, visual search, and set-shifting. Patients with bvFTD have shown a faster performance on this test than patients with AD or SD, but with a greater number of errors [48]. Studies have also shown that patients whose symptoms have progressed over time (bvFTD), in comparison with those whose clinical symptoms remained stable (phenocopy group), exhibit more deficits on this test [49].
- Wisconsin Card Sorting Test:
This test evaluates the ability to shift from one cognitive set to another. In this test, the subject has to sort cards containing geometric forms which differ in color, shape, and number. The participant’s first sorting choice becomes the correct feature, and once a criterion of six consecutive correct sorts is achieved, the subject is told that the rules have changed, and cards must be sorted according to a new feature. After all three features have been used as sorting criteria; subjects must cycle through them again in the same order as they did before. Each time the feature is changed, the next must be discovered by trial and error. Patients with bvFTD present more impairment in the ability to shift from one cognitive set to another, especially making more perseverative errors [9].
- Tower of London Test:
This is a neuropsychological measure of executive planning and problem-solving based on the original Tower of London (TOL) [50]. The TOL measures executive planning that involves the ability to conceptualize change, respond objectively, generate and select alternatives, and sustain attention. Previous studies have found that patients with bvFTD require greater numbers of moves, make more rule violations, and take more time to completion than AD patients [45].
- Hayling and Brixton Test:
This test evaluates inhibition of a prepotent response by employing a sentence completion task, with two sections including 15 sentences each. In the first section, subjects are required to complete a sentence with a word that gives a meaningful sense to the sentence. In the second section, the participant completes a sentence with a word that is unconnected to the sentence, which requires inhibiting an automatic response. Errors are recorded for words that do not follow these rules and the time taken to respond. Patients with bvFTD have shown more inhibitory errors on sentence completion, making this test one of the most sensitive ones to discriminate between bvFTD and AD [14]. Previous studies have also shown that patients whose symptoms have progressed over time (bvFTD), in comparison with those whose clinical symptoms remained stable (phenocopy group), have more deficits on this particular test [49].
- D-KEFS (The Delis–Kaplan Executive Function System):
This is a battery of nine standardized executive function tests (Trail Making, Verbal Fluency, Design Fluency, Color-Word Interference, Sorting, Twenty Questions, Word Context, Tower, and Proverb Interpretation) designed to comprehensively assess higher cognitive functions. Many studies have proven this battery useful in detecting executive dysfunction in patients with FTD, and in distinguishing them from other types of dementias [36]. Possin and colleagues showed that patients with bvFTD made significantly more design repetitions than other dementia groups [51].
Social cognition tests
Theory of mind tests
Theory of mind (ToM) refers to the capacity to infer others’ emotions and mental states. Deficits in ToM are widely regarded as one of the key defining features of bvFTD [9, 52, 53]. The ToM difficulties in bvFTD are significantly larger than the ToM difficulties reported in people with AD [53]. These point to the importance of using a ToM test during the diagnostic process of bvFTD in the early phases of this type of dementia.
The most frequent tests used to assess ToM ability in patients with bvFTD are: the Faux Pas Test [54], the Mind in the Eyes Test [55], Mind in the Voice (e.g., [56]), Face task [57], and first- and second-order false belief tasks [58].
- Faux Pas Test of Cognitive and Affective ToM:
In this test the subject is read a story that may or may not contain a social faux pas. In 10 of the stories, there is a faux pas, involving one person unintentionally saying something hurtful or insulting to another. Performance is scored regarding the adequate identification of the faux pas (hits) and the adequate rejection of those stories which did not contain a faux pas (rejects). After recognizing the faux pas, the subject is asked both intentionality and an emotion attribution question, which assess cognitive and affective ToM, respectively. Recent studies [9, 39, 53] reported ToM impairment in bvFTD patients using these tasks (Figure 9.2).
- Mind in the Eyes Test:
This test consists of 36 photographs showing only the eyes of different actors/actresses portraying different complex mental states. For each set of eyes, the subject is asked to choose one out of four words that best describes what the person on the picture was thinking or feeling. As a control, the subject is asked to judge the gender of each person in each photograph. The maximum obtainable score is 36. Multiple studies [9, 39, 53, 59] have reported ToM impairments in bvFTD patients using this test (Figure 9.2).
- Mind in the Voice:
The final version of this test includes 25 items, which consist of neutral content sentences recorded with a particular intonation referring to a particular emotion. The subject must hear every item and then choose from the four answer choices. For example, for the verbalization ‘‘Yeah, well, I know nothing about that,’’ in the original task, the four answers were “Defensive” (correct), “Joking” (incorrect), “Unconcerned,” and “Indignant” (e.g., [58]). Although no studies have been reported using this test in bvFTD patients, its utilization could be interesting for detecting deficits in this domain.
- Face task:
This task consists of 20 photographs of the same actress, who portrayed different complex mental states. For each set of faces, participants are asked to choose one out of two words best characterizing the feeling or thoughts expressed by the face. Correct answers are rated one, incorrect answers are rated zero. The maximum score of the test is 20. Although no studies have been reported using this test in bvFTD patients, its utilization could be interesting for detecting deficits in this domain.
- First- and second-order false belief tasks:
The first-order false belief tasks were designed to test subjects’ ability to infer that someone can have a mistaken belief that is different from their own true belief (of the form ‘‘A thinks X’’). The second-order false belief tasks were used to test the ability to understand what someone else thinks about what another person thinks (of the form ‘‘A thinks B thinks X’’). Four types of questions are asked per story (false belief, inference, fact, and memory) in an order from least to most explicit, to prevent cueing. Recent studies (e.g., [59]) have reported impairment in ToM in bvFTD patients using this task. The only exception is the study from Fernandez-Duque and colleagues [60], in which the authors found a preserved performance in first-order false belief tasks.
- Theory of mind cartoons:
Two sets of cartoon jokes are used – one set (physical) can be understood in physical terms, while the jokes in the other set (ToM) require the participants to perceive the mental state of the main character. The two sets are intermixed in a randomized order and given in a single test session. Participants are required to explain the jokes using the question “Why might someone find this funny?” In explaining the ToM jokes, patients have to use language to indicate that they have correctly perceived the mental state inferred in the cartoon for the interpretation of the joke to be accepted as correct. Each set is scored from a total of 10 with 1 point awarded for each acceptable explanation. Several studies (e.g., [61]) reported impairment in ToM in bvFTD patients using this task.
- Theory of mind stories:
The task consisted of participants reading 16 stories describing naturalistic social situations and being asked why the characters behaved as they did [62]. Half of the stories required ToM accounts to give a correct explanation, while the other eight required specifically a physical explanation. Each set of eight was scored with one point awarded for each acceptable explanation. Various studies (e.g., [61]) reported impairment in ToM in bvFTD patients using this task.
Other tests that are frequently used together with the ToM tests are those utilized to examine the ability to recognize emotions, such as the Awareness of Social Inference Test – Revised (TASIT-R) [63], the Emotional Morphing Test [64, 65], and the Interpersonal Reactivity Index (IRI) questionnaire [66], among others.
- The Awareness of Social Inference Test – Revised (TASIT-R):
This is a sensitive test of social perception comprising videotaped vignettes of everyday social interactions. This task introduces contextual cues (e.g., prosody, facial movement, and gestures) and additional processing demands (e.g., adequate speed of information processing, selective attention, and social reasoning) which are absent when viewing static displays. The brief version comprises a series of 20 short (15–60 seconds) videotaped vignettes of trained professional actors interacting in everyday situations. All scripts are neutral in content and do not lend themselves to any particular emotion. After viewing each scene, the test participant is instructed to choose from a forced-choice list the emotion expressed by the focused actor (fearful, surprised, sad, angry, and disgusted). Savage et al. [67], Rankin et al. [68] and Kipps et al. [69] reported impairment in emotional recognition in bvFTD patients using this task.
- Emotional Morphing Test:
This is a facial expression recognition task featuring six basic emotions (happiness, surprise, sadness, fear, anger, and disgust) taken from a pictures-of-affect series [64]. The pictures have been morphed for each prototype emotion and for a neutral state [65]. Facial morphing is generated by taking a variable percentage of the shape and texture differences between the two standard images: 0% (neutral) and 100% (full emotion). Participants are asked to respond as soon as they recognize the facial expression, and then to identify the facial expression from a forced-choice list of six options. This task measures the accuracy of emotion recognition and reaction times (RTs). Emotion recognition deficits in bvFTD and SD are known to be amodal, with patients demonstrating impaired recognition of verbal and non-verbal stimuli more consistently demonstrated in negative emotions [70]. Diehl-Schmid and colleagues investigated whether the Ekman 60 Faces Test was capable of differentiating between patients with mild FTD and healthy subjects, concluding that it can discriminate between them with 97% diagnostic accuracy (sensitivity: 94%; specificity: 100%) [71].
- Interpersonal Reactivity Index (IRI):
This is a standardized, 28-item questionnaire of empathy that yields a total score, as well as 4 subscale scores (perspective-taking, fantasy, empathic concern, and personal distress). Contrasting the perspective-taking and empathic concern subscales can help comparing cognitive and emotional aspects of empathy. Following the procedure of Perry et al. [72], two versions of the IRI can be administered – one to the caregiver and one to the patient with bvFTD – and by this method any perceived change over time in the patient´s empathy could be quantified, and the patient’s insight into the changes perceived by the caregiver can be rated. Various studies (e.g., [4, 73]) have reported impairment in empathy measures in bvFTD patients using this task.
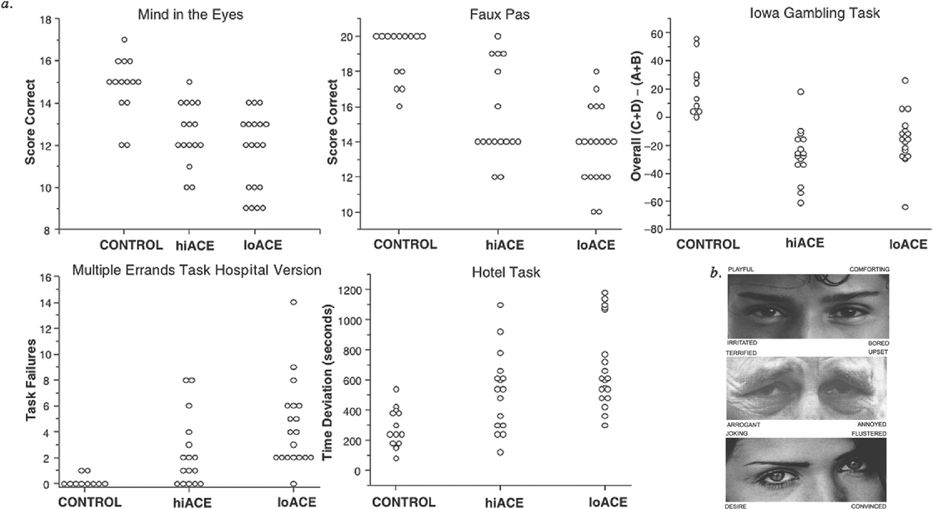
Individual patient scores on the tasks of the Executive and Social Cognition Battery (ESCB) [9].
More complex ecologically valid executive function tests
There is a group of tests that it is important to include in order to capture the sometimes-subtle deficits that bvFTD patients present in the early stages of the disease. Some of them are the MET-HV [74], the Hotel Task [75], and the Iowa Gambling Task [76].
- Multiple Errands Test Hospital Version (MET-HV):
This test, which is frequently administered at the hospital and its surroundings, requires participants to carry out a number of tasks simulating “real-life” situations where minor inconveniences can take place. While still inside the hospital, the patient is given a card with 4 sets of simple tasks totaling 12 subtasks. Nine rules are clearly stated in the instruction sheet. Errors in this test are categorized as: (1) inefficiencies; (2) rule breaks; (3) interpretation failure; (4) task failures; and (5) total failures. In our study [10] (Figure 9.2) bvFTD patients made more errors than healthy controls (inefficiencies), acting more impulsively (rule breaks), with no apparent planning, and poor organization of the tasks (task failures).
- The Hotel Task:
This multitasking task comprises five activities that would plausibly need to be completed in the course of running a hotel. The main goal is to attempt to do each of the 5 tasks in 15 minutes. The materials needed to perform these activities are arranged on a desk and randomly distributed between participants and sessions. The details for each of the following tasks are clearly described. In our study [9] (Figure 9.2) bvFTD patients differed significantly from healthy controls in the optimal time deviation of the task, which is a measure closely associated with planning and flexibility (two of the hallmarks of executive functioning).
- Iowa Gambling Task (IGT):
This is one of the most frequently used decision-making tests in patients with bvFTD. The computerized version of the IGT mimics real-life personal decision-making activities in real time. Participants are asked to continuously select cards from four decks (A, B, C, and D) in order to make as much money as possible in the game. The task is completed after 100 selections. Following card selection, participants receive a certain amount of reward, but some choices also result in loss of money (penalties). Decks A and B are ultimately risky (large rewards and large punishments) while C and D are more conservative (small rewards and small penalties). In Table 9.1 a summary of studies of decision-making cognition in FTD from the Gleichgerrcht et al. 2010 paper is presented [73], suggesting that the IGT could be used to provide complementary information to a frontal test battery, especially in the early stages of the disease before severe dementia develops.
| Study | Participants | Decision-making paradigm | Correlation with EF | Other multivariate comparison? | Brain and/or peripheral biomarker? | Main results |
|---|---|---|---|---|---|---|
| Rahman et al. (1999) | 8 FTD, 8 controls | CGT | No | No | No | Deficit in risk adjustment and risk-taking behavior, and increased deliberation times in patient group |
| Rahman et al. (2005) | 8 FTD | CGT | No | No | Yes: cardiovascular | Attenuation of risk-taking behavior following single dose (40 mg) of methylphenidate |
| Torralva et al. (2007) | 20 FTD, 10 controls | IGT | No | Yes: no correlations | No | Poor performance on IGT independent of ToM deficits |
| Torralva et al. (2009) | 35 FTD, 14 controls | IGT | Yes: impaired mental flexibility on WCST | Yes: no correlations | No | Poor performance on IGT |
| Manes et al. (2010) | FTD (1) | IGT | No | No | No | Genuine risk-taking behavior |
Some new batteries have emerged, combining different tests, that have proven to be sensitive to early changes in bvFTD patients. Because of space constraints, only two of them will be detailed here: the SEA (Social cognition and Emotional Assessment) [77] and the Executive and Social Cognition Battery (ESCB) [9].
- The SEA (Social cognition and Emotional Assessment):
The SEA is an easy tool that has been recently proposed to diagnose and assess emotional recognition and ToM deficits in bvFTD. It consists of five subtests: (1) a facial emotion recognition test (from Ekman pictures), (2) a shortened version of the Faux Pas recognition test evaluating theory of mind, (3) a behavioral control test in which patients must learn to apply a strategy of choice and to modify their choice based on monetary reward, (4) a reversal learning and extinction test where patients must reverse a pattern of reinforced choice after contingencies are unexpectedly reversed, and (5) an apathy scale. A study conducted by Bertoux and his collaborators demonstrated that both the SEA and mini-SEA (a shortened version) scores distinguished early bvFTD from depression with sensitivity and specificity rates above 94% [78]. Unlike standard executive neuropsychological tests, the SEA and the mini-SEA are capable of differentiating depression from bvFTD in the early stages of the disease.
- Executive and Social Cognition Battery (ESCB):
This new proposed battery consists of a group of tests that measure performance of “daily life” activities within a “real-life” environment: the Multiple Errands Test; the Hotel Task; complex decision-making (Iowa Gambling Task); and social cognition (ToM tests). We demonstrated that bvFTD patients with an apparent high performance on a standard neuropsychological test do not differ significantly from controls in their performance on basic cognitive domains or classical tests of executive function, but fail in this battery [9]. Our results suggest that this battery is more sensitive in detecting executive and social cognitive impairment deficits in early bvFTD dementia than classical cognitive measures (see case presentation in Figure 9.3).
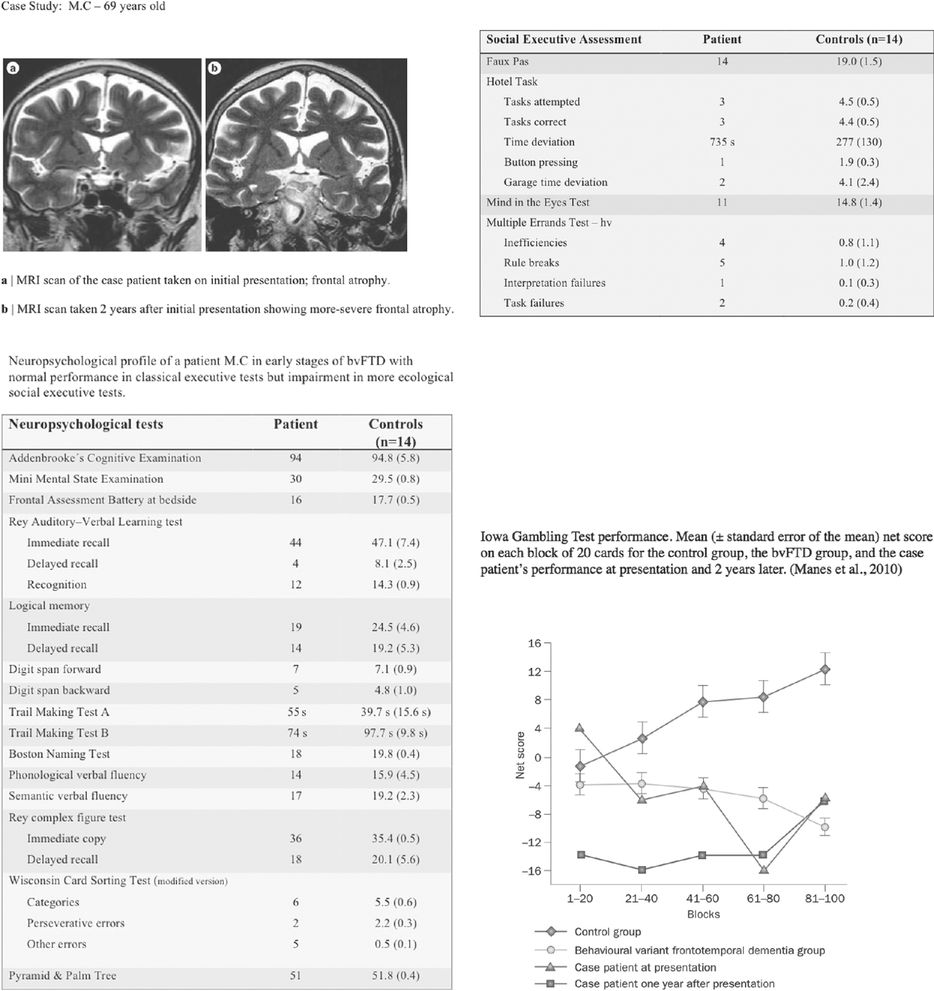
bvFTD Case Study M.C (MRI scan and neuropsychological profile).
Language
It is by now clear that the greatest deficits in bvFTD patients appear to be in the domains of executive functions, attention, and some types of memory but it is important to check also other domains such as language. Although the language variants of FTD have the greatest deficits in the language domain, patients with bvFTD should be assessed with a short language battery too. It is important to consider that if any of the language tests appear to be impaired, a more comprehensive language battery should be utilized to understand the profile more fully. No specific tests will be explained in this section as they will be explained in detail in the next section of this chapter.
Language variants of FTD
As described in detail in Chapter 5, three variants of primary progressive aphasia (PPA) are described: PNFA, semantic variant progressive aphasia (svPPA), which is also referred to as “semantic dementia” (SD), and LPA [79]. In recent years many tests and batteries have been developed to assess patients with suspected PPA. Patients with PPA may present with very different linguistic abnormalities. They may have difficulties in word retrieval, in understanding the meaning of words, or in speech patterns or the production of grammatically correct sentences. Thus, tests of word comprehension, speech production (fluency, naming, and repetition), and also oral reading (to detect surface dyslexia) and writing (to detect surface agraphia) should be assessed in the three variants of PPA.
Semantic memory
This long-term memory system is severely affected in SD, in contrast with PNFA and LPA (e.g., [79, 80]). Semantic tests assess long-term memory for facts, objects, and concepts as well as words and their meaning [81]. Semantic memory is usually assessed with tasks such as picture naming, defining spoken or written words, picture matching, category fluency tests, semantic judgments, analogies, or associative semantic tests [81].
The most frequent tests used to assess semantic memory skills are the Pyramids and Palm Trees Test [82], Cambridge Semantic Memory Test Battery [83], Repeat and Point [84], Kissing and Dancing Test [85], or the Words and Sentences (oral or written) Picture Matching tasks from the Psycholinguistic Assessment of Language Processing in Aphasia (PALPA) [86].
- Pyramids and Palm Trees Test (PPT):
This is the most widely used test to assess semantic memory. The aim of this assessment is to associate a picture (or a word) with another picture; for example, a pyramid is associated with a palm tree rather than a pine tree. This test contains 52 specimens, and has different administration modalities: pictorial, verbal, and combined. The three-picture modality is, however, the most commonly used. This is very useful to detect semantic problems. SD patients will have many problems in this test, also, in the early stages of the diseases. LPA and PNFA will resolve this test without problems.
- Cambridge Semantic Memory Test Battery:
This is a battery specifically developed to diagnose a specific semantic category deficit. Nevertheless, this battery fails to differentiate between patients with SD and AD. The authors use 64 items, 32 living things (animals and fruits) and 32 man-made (e.g., transport). The same items are used to evaluate conceptual information across different input and output modalities. The different subtests are: category fluency, picture naming, matching word–picture, pictures and words sorting according to different semantic complexity levels, and a word definition task. This battery also includes an associative semantic test, the Camel and Cactus Test (CCT). This test is similar to the PPT, but it has several differences: in the PPT the subject has to choose one of the two possibilities, instead in the CCT, subjects have to select one of four possibilities, so they have less chances of selecting without knowledge. Another advantage of this test is that this subtest assesses the same 64 items and it has colored pictures. This is a notable difference from other semantic tests because color is an important semantic attribute [87].
- Repeat and Point Test:
This is a quick measure to differentiate between SD and PNFA. This test contains 10 items and has 2 aims. First of all, participants have to repeat a word (which represents a concrete noun). Once they repeat it, they have to select a picture that represents the target word. The subject has to choose between seven pictures that are semantically and perceptually similar. SD patients could repeat words without problems but they will fail in the matching part. PNFA patients have the opposite pattern. They have repetition problems but they could match word–picture correctly [84].
- Kissing and Dancing Test (KDT):
This is another associative semantic test and contains the same number of triads as the PPT. The aim of this test is to assess the knowledge of actions and verbs. The authors considered the KDT to be an extension of the PPT. A comparison between the two tests allows the diagnosis of possible dissociations between grammatical categories (nouns/verbs) and semantic categories (objects/actions). Bak and Hodges compared SD in PPT and KDT, and found that patients had poor performance on both batteries [85].
- Word (oral or written) Picture Matching. Psycholinguistic Assessment of Language Processing in Aphasia (PALPA):
This is another kind of test assessing concrete knowledge. The patient must match a word (oral or written) with a picture that represents it out of five possibilities (the target, a near-related semantic distracter, a distant-related semantic distracter, a visual distracter, and an unrelated picture). The picture selected can allow different types of semantic impairments to be identified [86].
- Sentences (oral or written) Picture Matching. Psycholinguistic Assessment of Language Processing in Aphasia (PALPA):
These tasks allow for the assessment of sentence comprehension. Different grammatical structures are presented. LPA patients, because of the problems in auditory verbal short-term memory, will have deficits in sentences comprehension [80]. PNFA patients also have difficulty with grammatical comprehension for complex grammatical constructions [88].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






