Cranial
1. What is the characteristic angiographic appearance of vessels in fibromuscular disease (FMD)?
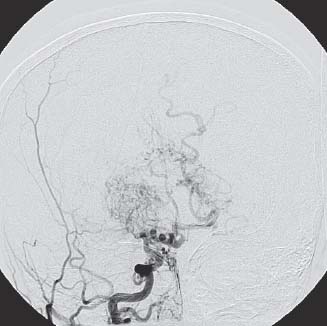
FMD is an angiopathy that affects medium-sized arteries predominantly in young women of childbearing age. FMD most commonly affects the renal arteries and can cause refractory renovascular hypertension. Of patients with identified FMD, renal involvement occurs in 60 to 75%, cerebrovascular involvement occurs in 25 to 30%, visceral involvement occurs in 9%, and arteries of the limbs are affected in ~5%. The classic “beads on a string” appearance is typical of medial fibroplasia, the most common type of FMD (Fig. 9.1).1

Fig. 9.1 Carotid angiogram demonstrating findings in fibromuscular dysplasia.
2. What are the three anatomic appearances of normal pineal gland on contrast-enhanced imaging?
A normal pineal gland could appear as a nodule (52%), or have a crescent (26%) or ring-like (22%) shape.2
3. What is the common computed tomographic (CT) finding both in pseudotumor cerebri and in ventriculoperitoneal (VP) shunt overdrainage?
Slit-like ventricles. These are small ventricles, sometimes so small that they are barely visible on CT or magnetic resonance imaging (MRI) scans. Slit ventricles can occur after severe head injury or viral infection of the brain. In the case of a VP shunt, the ventricles become completely decompressed due to very low draining pressure. Pseudotumor cerebri is characterized by increased intracranial pressure without hydrocephalus, mass or meningitis, or hypertensive encephalitis. The problem is cerebrospinal fluid (CSF) malabsorption causing cerebral edema.3
4. What is the angiographic finding of mass effect due to a brain tumor on an anteroposterior (AP) view?
The pericallosal arteries are seen as a bayonet- or stairstep-shaped bend under the falx cerebri. This phenomenon is called square shift. The same type of shift is observed in the displacement of callosomarginal artery under the anterior falx.
5. What is the most common nontumoral MRI finding in patients with complex partial epilepsy?
Chronic temporal lobe seizures are typically associated with atrophy of the hippocampus and, less commonly, the parahippocampal gyrus. This type of atrophy is associated with sclerosis most of the time.4
6. In what forms can hemangioblastomas appear on CT or MRI?
Vascular nodule on the side of the cyst, vascular nodule encompassing the cyst, or solid vascular mass are the types encountered on contrast-enhanced CT or MRI. However, a cyst with a nodule on the side is most commonly seen (60%).5
7. What can be seen in the anterior vascular MRI/MRA in relation to a presellar versus a postsellar tumor?
A presellar localization causes elevation of A1 segments of anterior cerebral arteries, whereas a postsellar tumor does not generally displace them.
8. What is the normal expected range of the diameter of an internal acoustic opening to assess any abnormal widening due to acoustic neuroma on a CT scan?
Most acoustic neurinomas enlarge the ostium of the internal acoustic canal; only 3 to 5% of these tumors do not cause enlargement. An internal acoustic opening more than 5 to 8 mm in diameter should raise a question whether this is caused by an intracanalicular neuroma.6
9. What is the differential diagnosis for a spherical hypointense mass in the suprasellar region in the MRI?
The most important two are Rathke cleft cyst and aneurysm due to the flow void. If a vascular lesion is suspected, a formal angiogram must be performed. Cystic microadenoma and epidermoid cysts are also considered among the differential diagnosis.7
10. What is the enhancement pattern of a pituitary adenoma with contrast relative to a normal gland?
Normal gland will enhance immediately after the contrast injection as opposed to adenoma that remains unchanged; however, 30 minutes postinjection, the normal gland loses its enhancement and tumor enhances.8
11. What are the MRI signs of acute intracranial hypotension?
Diffuse pachymeningeal (dural) enhancement, bilateral subdural effusion/hematomas, downward displacement of brain, enlargement of the pituitary gland, engorgement of the dural venous sinuses, prominence of spinal epidural venous plexus, venous sinus thrombosis, and isolated cortical vein thrombosis9
12. What type of imaging is most helpful to detect diffuse axonal (shearing) injury?
Diffuse axonal injury is notorious for poor visualization on CT. When it is nonhemorrhagic, it is best demonstrated with T2-weighted (T2W) MRI. When it is hemorrhagic, long echo time (TE) gradient-echo (GRE) MRI shows the injury best.10
13. What are the findings of Dandy-Walker malformation on a coronal T2W MRI?
Dandy-Walker malformation is characterized by cystic dilatation of the 4th ventricle, complete or partial agenesis of the cerebellar vermis, and an enlarged posterior fossa. Keyhole formation in the large 4th ventricle and inverted Y due to elevated tentorium and torcula are highly suggestive of the disease.11
14. What are the best diagnostic clues for Sturge-Weber syndrome in MRI?
Cortical calcification, atrophy, and enlarged ipsilateral choroid plexus are the typical MRI findings. In skull radiography, tram-track calcification is also considered a typical sign.12
15. What are the best diagnostic tools and the findings they provide to confirm the diagnosis of traumatic extracranial arterial dissection?
MRI and CT angiography (CTA) are the modalities of choice. MRI reveals a crescentic hyperintensity. On CTA, a tapered narrowing with or without a block is highly suggestive of dissection. Vertebral arteries are the most common location.
16. What are the diagnostic clues on CT and MRI in a patient with suspected traumatic carotid-cavernous fistula?
Enlarged superior ophthalmic vein on contrast CT and dilated cavernous sinus as flow voids on T1W MRI, along with marked proptosis and swelling of eyelids13
17. What are the components of an infundibulum seen on cerebral angiography?
The most common location is the posterior communicating artery; it arises directly from its apex. It is conical in shape and less than 3 mm in size.
18. What are the image characteristics of multiple sclerosis (MS) on MRI?
Multiple perpendicular callososeptal hyperintensities along the penetrating venules (Dawson fingers), bilateral asymmetric ovoid FLAIR (fluid attenuated inversion recovery) hyperintensities, and transient enhancement during active demyelination.14
19. How is cerebellopontine angle (CPA) arachnoid cyst differentiated from an epidermoid cyst?
Epidermoid cysts present restricted diffusion in diffusion weighted image (DWI) sequence, whereas arachnoid cysts do not. An arachnoid cyst is the closest differential diagnosis that carries similar MRI features, except for the restricted diffusion on DWI.
20. What is the term “Medusa head” used to describe on MRI or angio?
A developmental venous anomaly is characterized by dilated medullary veins that course in the white matter, resembling “caput meduse” or “medusa head.” These anomalous venous structures tend to coincide with cavernomas (Fig. 9.2). The risk of bleeding is lower than for the other vascular malformations such as arteriovenous malformations (AVMs) or cavernous malformations.15
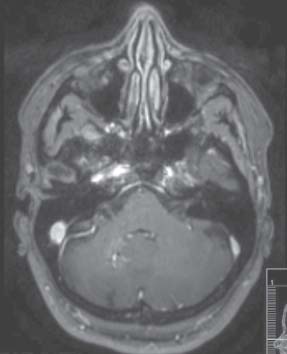
Fig. 9.2 Axial T1-weighted magnetic resonance image demonstrating cavernous angioma (or cavernoma) of the cerebellar hemisphere with associated venous angioma.
21. What are the MRI findings of Wilson disease?
Wilson disease is suggested mainly in T2W images by brain atrophy (focal/diffuse), high signal intensity at the lentiform nuclei with bilateral symmetrical and concentric lamellar putaminal pattern, thalamic and caudate nuclei, substantia nigra, periaqueductal gray matter, pontine tegmentum, and cerebellum, cortical, and subcortical areas with frontal lobe predilection.16
22. What is the best imaging tool for cavernous malformations and what are the most common findings.
T2W GRE MRI is the best tool for cavernous malformations. Hypointense “blooming” and numerous punctuate hypointense foci (“black dotsrdquo;) if the lesion is greater than 3 cm are the most common findings on T2W GRE.15
23. What are the commonly accepted angiographic criteria for AVMs with a relatively higher risk of bleeding?
Stenotic venous drainage, single draining vein, intranidal aneurysm, smaller nidus, and deep location are the features seen in the AVMs that are more likely to bleed.17
24. What is the chronologic order of angiographic findings in moyamoya disease?
A narrowing in the circle of Willis and the internal carotid artery is the earliest finding. Then, lenticulostriate and thalamoperforator collaterals develop in the intermediate phase. Transdural external carotid-internal carotid (EC-IC) collaterals emerge in the late phases of the disease (Fig. 9.3).18