, Wei Liu1, Shikun Zhan1, Qianqian Hao1, Dianyou Li1, Yixin Pan1, Yongchao Li2 and Guozhen Lin2
(1)
Department of Functional Neurosurgery, Ruijin Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
(2)
Department of Psychiatry, Ruijin Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
Abstract
Schizophrenia is a chronic, severe, and disabling psychiatric disease that is characterized by perturbations in cognition, affect, and behavior. Of the many available treatments, pharmaceutical interventions remain as first choice-treatments. However, about 20 % of patients with schizophrenia exhibit refractory schizophrenia that does not respond well to pharmaceutical treatments. As a result, neurosurgery performed for the treatment of refractory schizophrenia, also called psychosurgery, is an alternative treatment that has a long history. With the refinement and improved accuracy of neuroimaging techniques, modern psychosurgery has greater success with fewer risks. Nevertheless, these procedures are still invasive methods and the resulting lesions are irreversible. Therefore, we must keep in mind that surgical therapy should only be considered as a supplementary part of the comprehensive treatment of schizophrenia and the inclusion criteria for surgery must be strict.
16.1 Introduction
Schizophrenia, which was also called “dementia praecox” by Emil Kraepelin, a German psychiatrist in the late nineteenth and early twentieth century, is a chronic, severe, and disabling mental disorder characterized by perturbations in cognition, affect, and behavior. It is diagnosed on the basis of a series of clinical psychiatric symptoms such as auditory hallucinations, paranoia, or disorganized speech and thinking. Symptoms of schizophrenia typically emerge in adolescence and early adulthood, with a global lifetime prevalence of about 0.30–0.66 % [1]. Schizophrenia does not only affect mental health, but also negatively impacts physical health, shortening the life expectancy of patients with schizophrenia by 12–15 years compared to the general population; this gap has also widened over recent decades [2]. Therefore, schizophrenia causes more loss of life than most cancers and physical illnesses. Furthermore, it is one of the most burdening and costly illnesses worldwide [3–5].
The exact mechanisms underlying schizophrenia are still unclear. However, scientists have long known that genetic factors play an important role in the development of schizophrenia. The illness occurs in less than 1 % of the general population, but, interestingly, it occurs in about 10 % of people who have a first-degree relative with the disorder. Monozygotic twins have a concordance rate of about 50 % [6]. Besides genetic susceptibility, many environmental factors may be involved in the development of schizophrenia, such as exposure to viruses, difficulties during birth, and other unknown psychosocial factors. Therefore, most researchers believe that interactions between genes and the environment are necessary for the development of schizophrenia.
There are many hypotheses to explain the underlying mechanisms of schizophrenia. Rossum [7] first presented the dopamine (DA) hypothesis of schizophrenia based on the observation that antipsychotics may block DA receptors. Subsequently, accumulating evidence supported the idea that schizophrenia is associated with frontal-subcortical neuronal circuits, especially the orbito-frontal and anterior cingulate circuits [8–11]. The orbito-frontal circuit projects to the ventromedial caudate nucleus and the anterior cingulate circuit sends fibers to the ventral striatum, which includes the ventromedial caudate, ventral putamen, nucleus accumbens , and olfactory tubercle. These circuits primarily use DA as a neurotransmitter, and process cortical-subcortical emotional information. Disrupting these circuits can thus trigger the onset of schizophrenia’s positive symptoms. Besides the DA hypothesis, it was reported that the serotoninergic system plays an important role in the negative symptoms of schizophrenia. Serotoninergic neurons from the dorsal and median raphe nucleus project to the prefrontal cortex (PFC), and the PFC sends projections back to the raphe nuclei providing feedback control of cortical serotonin release. Serotonin could stimulate 5-HT2A receptors in the PFC that inhibits the activity of dopaminergic neurons in this area.
At present, pharmaceutical treatment is the first option pursued in schizophrenia. The first-line drugs used in schizophrenia include: Haloperidol, Perphenazine, Chlorpromazine, Risperidone, Aripiprazole, Clozapine, and Olanzapine. Among these drugs, Haloperidol, Perphenazine, and Chlorpromazine are first-generation antipsychotics, while the remainder are second-generation antipsychotics. Although controversy remains over the higher rate of effectiveness of second-generation antipsychotics, the use of drugs such as Clozapine and Olanzapine has grown due to their inducing fewer side effects. Medication usually shows good results in the treatment of positive symptoms of schizophrenia while negative symptoms are generally less receptive to similar treatment. Besides medication, family therapy, supported employment, skills training, and other psychosocial interventions may be helpful in the treatment of schizophrenia [12–15]. However, approximately 20 % of schizophrenics remain non-responsive to any of the aforementioned treatments [16]. For refractory schizophrenia, psychosurgery, also called neurosurgery for mental disorders, is considered as a last resort. In this chapter, we briefly introduce the history, indications, optimal surgical target, surgical procedure, and surgical results of psychosurgery applied in schizophrenia.
16.2 A Brief History of Psychosurgery
Psychosurgery, including the lesion and stimulation techniques, has a long and storied history which can be traced back to ancient times. A skull with a trepanation hole identified in France has been carbon dated to the Neolithic period of the Stone Age, or approximately 5100 BC [17]. Signs of healing in the skull indicate a surgical rather than a traumatic origin of the wound. Literature on trephination for the relief of neuropsychiatric symptoms stemming from mental disorders can be dated back to 1500 BC [18].
In the modern era, the links between the brain and behavior was brought into cultural awareness through the famous account of Phineas P. Gage, a railroad worker in Vermont. Gage experienced a terrible explosion that caused severe head trauma. He miraculously survived, but his personality was profoundly altered [19]. The first psychosurgical procedure was performed in 1888 by Swiss psychiatrist Gottlieb Burckhardt, who contributed widely to the birth of modern psychosurgery. The process involved the excision of cerebrum at multiple foci in frontal, parietal, and temporal cortices. The results of six cases ranged from success (in three patients) to failure (in one fatal case) [20]. Almost 50 years later, the Portuguese neurologist Egas Moniz, who is often regarded as the founder of psychosurgery, performed the first prefrontal lobotomy in 1935 with the help of neurosurgeon Almeida Lima. Different from the psychosurgical interventions performed by Burckhardt, Moniz’s surgery focused on the white matter of the brain and garnered great attention worldwide. He won the Nobel Prize for Medicine in 1949, which is still highly controversial today. In the United States, Freeman and Watts introduced the prefrontal lobotomy in 1942. There was an upsurge in surgical interventions between 1943 and 1954 because of the lack of effective psychopharmacological agents and the large social and financial burdens of psychiatric illness.
However, with the introduction of newer psychotropic medications, such as chlorpromazine, and the growing realization of severe surgical side effects, psychosurgery lost its popularity as a treatment [21]. Although stereotactic and functional neurosurgery for alleviating psychiatric disorders was maturing due to the development of stereotactic neurosurgical devices and neuroimaging , it is approved only in specific circumstances and performed only in a few specialized centers across the globe, largely as a precaution against widespread abuse similar to that of the prefrontal lobotomy. Several procedures including anterior capsulotomy , anterior cingulotomy , amygdaloidotomy, subcaudate tractotomy , and limbic leucotomy have been sparingly applied in schizophrenia patients [18, 22–26]. Different from the interventions used in the past, most procedures today are performed with the help of CT or MRI guidance. The high-resolution of MRI provides the exact location of the target, which has reduced the severe adverse effects. These procedures are relatively safe, minimally invasive, effective, and have fewer side effects and complications compared to the prefrontal lobotomy.
16.3 Patient Selection Criteria
Patient selection criteria are strict for treating refractory schizophrenia (TRS). A general consensus about the selection criteria for TRS surgery in our center is summarized below:
1.
Patients diagnosed with schizophrenia in the Department of Psychiatry by independent psychiatrists according to the DSM-IV.
2.
Refractory schizophrenia patients confirmed by a team of psychiatrists, neurosurgeons, and neurologists and proposed for neurosurgical treatment. In our center, refractory schizophrenia is defined as follows:
(I)
Illness severity with a score of ≥35 on the 18-item Brief Psychiatric Rating Scale (BPRS, scored 1–7) and a clinical global impression (CGI) >4.
(II)
At least three periods of treatment in the three preceding years with neuroleptic agents (at least two different chemical classes) at dosages equivalent to or greater than 500 mg/d of Chlorpromazine for a period of 8 weeks, each without significant symptomatic relief.
(III)
Duration of mental disorder >3 years and no period of good function.
3.
Patients or their representatives must be able and willing to give informed consent and have the support of their family.
4.
Patients are between the ages of 18 and 60 years old.
5.
Pregnant women are excluded.
6.
Patients are considered for psychosurgery only if there are no contraindications, such as severe organic brain damage.
16.4 Surgical Treatment
The advent of stereotactic and functional neurosurgery reemerged as an option for the most severe, chronic, and refractory schizophrenia patients after the decline of the classical lobotomy. As I mentioned above, the most common procedures have included anterior cingulotomy , subcaudate tractotomy , limbic leucotomy , anterior capsulotomy , and amygdaloidotomy. In our center, anterior capsulotomy and anterior cingulotomy are the most performed surgeries. They are described in more detail below.
16.4.1 Anterior Capsulotomy
In this procedure, lesions are made within the anterior limb of the internal capsule to cut the connective fibers between prefrontal cortex and subcortical nuclei (dorsomedial thalamus included). The lesions may be produced by thermal coagulation or focal gamma radiation guided by CT or MRI. Because of the large individual differences in the anterior capsule, MRI targeting became the best modality to identify the location of the structures. The target is identified with the visualization of the internal capsule on stereotactic MRIs. Usually, the target lies 15–17 mm anterior to the AC, 15–17 mm lateral to the midline, and 2–4 mm under the AC-PC line. Two bilateral trepanations are made immediately behind the coronal suture and the lesion is created by thermo-coagulation through radiofrequency probes reaching 80 °C for approximately 60 s. The first lesion is located 3–4 mm below the AC-PC line and extends up to 10-mm above the AC-PC line. During lesioning, neurological testing is carried out to ensure no impairment of motor or sensory functions. After adequate cooling, the electrode is withdrawn 2 mm and the ablation procedure is repeated 4–5 times to ensure the complete ablation of the target. Finally, a lesion 4-mm in diameter and 10-mm in length along the contoured target is produced [27] (Fig. 16.1).
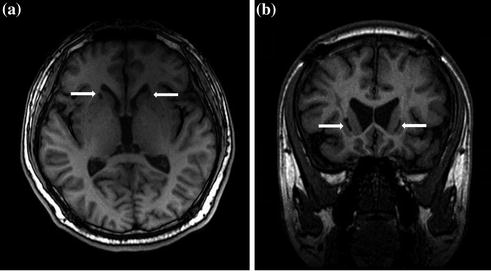
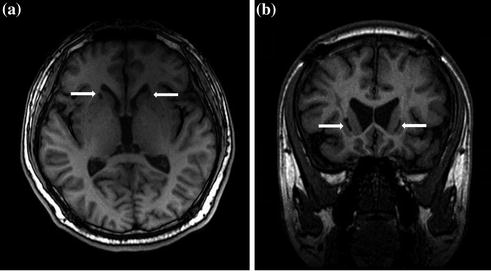
Fig. 16.1
MRI slices showing a typical lesion in the mid-third portion of the bilateral ALIC (arrows). a Axial view. b Coronal view
16.4.2 Anterior Cingulotomy
In the U.S., anterior cingulotomy is currently one of the most widely used psychosurgical procedures [28]. In our center, cingulotomy is usually performed together with capsulotomy to control the symptoms of some very severely refractory schizophrenia patients. In this procedure, MRI is also used to identify the location of the target structures. The initial targets are located 0.7 cm lateral to the midline bilaterally, 2 cm posterior to the most anterior portions of the frontal horns, and 1-mm above the roof of the ventricles. Typically, lesions are created by thermo-coagulation through radiofrequency probes reaching to 80–85 °C for 90 s. The electrode is then withdrawn 1 cm and the lesion is enlarged superiorly using the same lesion parameters. These steps are repeated for the opposite hemisphere. This produces bilateral symmetrical lesions in the anterior cingulate cortices [29] (Fig. 16.2).
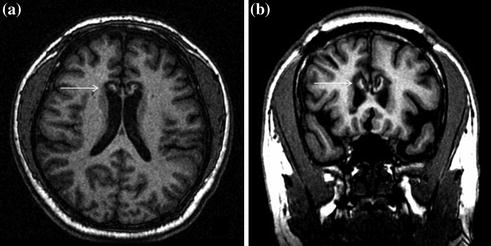
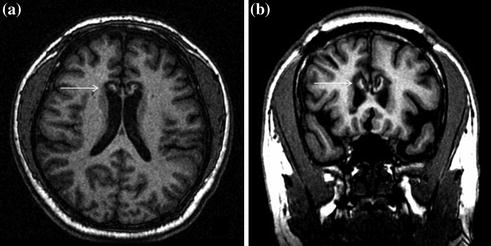
Fig. 16.2
MRI slices showing a typical lesion in the bilateral anterior cingulate gyrus (arrows). a Axial view. b Coronal view
16.5 Surgical Outcomes
The prognosis of schizophrenia in patients undergoing different types of psychosurgery varies widely. Frontal lobotomy was the most common psychosurgery; between the 1940s and the 1950s, over 40,000 Americans were lobotomized. If the surgery was performed before the development of severe schizophrenia, Freeman found that lobotomy reduced the likelihood of disease progression [30]. In contrast to the findings of Freeman, Dynes found that some patients remained hospitalized for more than a decade even after classical lobotomy [31]. Miller and Cummings [32] believed that psychosurgery should be applied in a limited fashion for more problematic and intractable psychological disorders considering the improvements found in violent behavior in schizophrenia patients. Some reviews have also focused on the role of lobotomy in the treatment of schizophrenia. By investigating more than 7,500 patients who received a frontal lobotomy in England from 1942 to 1952, Tooth and Newton found that only 18 % of patients showed signs of improvement [33]. Da Costa reported that frontal lobotomy reduced aggression and/or produced a marked to slight improvement in 16 schizophrenia patients.
Stereotactic and functional neurosurgery including anterior cingulotomy, subcaudate tractotomy , limbic leucotomy , anterior capsulotomy , and amygdaloidotomy were introduced later as an alternative treatment for refractory schizophrenia patients. Compared with lobotomy, these procedures are demonstrated to be relatively safe and have better outcomes. Among these modern procedures, patients who underwent cingulotomy had the best reported outcomes [34]. In 1987, Ballantine et al. reported a study involving 11 patients with schizophrenia who underwent anterior cingulotomy with a long-term follow-up, in which 4 of 11 patients experienced considerable improvement without deficits in intellectual or emotional function. In our center, cingulotomy is performed only on patients who do not respond well to treatment with capsulotomy . In our experience, the combination of cingulotomy and capsulotomy usually control the symptoms of severely refractory schizophrenia patients in spite of more complications. Similar to cingulotomy , stereotactic subcaudate tractotomy also has little impact on schizophrenia [35]. According to the studies of Talairach and Herner, the initial outcomes of anterior capsulotomy for the treatment of schizophrenia were disappointing, with only 27 % of patients having a positive response. However, we find better results with anterior capsulotomy in our schizophrenia patients. In our center, 100 refractory schizophrenia patients who met the inclusion criteria (see Patient Selection Criteria above) were treated with capsulotomy guided by MRI; 74 % of such patients demonstrated improvements. The accurate target localization with the help of MRI greatly contributes to the improved outcomes of capsulotomy . Amygdaloidotomy is usually used in schizophrenia patients with severely aggressive behavior and a large percentage of cases showed a marked reduction in aggressive behavior [36]. In our center, amygdaloidotomy is restricted to refractory schizophrenia patients with severely aggressive behavior. The results are consistent with the aforementioned study. Besides our center, many neurosurgeons in China have also applied stereotactic surgery in schizophrenia patients (see Table 16.1).
Table 16.1
Summary of the stereotactic neurosurgery in schizophrenia patients in China
Series (ref. no.) | No. of patients | Target area | Follow-up period | Patients with improvement | Complications |
|---|---|---|---|---|---|
Liu Weiqin et al. (2002) | 118 | Bilateral arterial limb of internal capsule + bilateral cingulate gyrus + amygdaloid nucleus | 6 months | Improvement: 108 No improvement: 10 | Hallucinations, mania: 16 Urinary incontinence: 6 Hemiplegic paralysis: 2 |
13 | Bilateral arterial limb of internal capsule + bilateral cingulate gyrus | Improvement : 6 No improvement: 7 | |||
7 | Bilateral anterior limb of internal capsule + bilateral cingulate gyrus + amygdaloid nucleus + hippocampus | Improvement: 7 | |||
Wang Xiaofeng et al. (2002) | 51 | Bilateral anterior limb of internal capsule + cingulated gyrus + amygdaloid nucleus | 6 months | PANSS evaluation P: p < 0.01 N: p < 0.01 G: p < 0.01 | a |
Xu Zhiju et al. (1996) | 18 | Cingulated gyrus | 10 years | Improvements: 9 No improvements: 9 | a |
Chen Chengyu et al. (2002)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|




