Obsessive–compulsive disorder
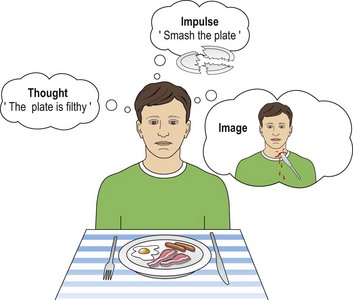
Obsessions, also known as obsessional ruminations, are unpleasant or distressing thoughts, impulses or images that come to mind over and over again, despite conscious efforts to stop them (Fig. 1). They dominate the person’s mind and the sufferer is unable to distract themselves, leading to impairment of social and occupational function. Common themes for obsessional thoughts include violence, sex, contamination and blasphemy. Obsessional images may be of violent or gory scenes that come vividly to mind again and again, and cannot be ignored or suppressed. An obsessional impulse might be a recurrent impulse to hurt someone, usually someone the sufferer would not consciously wish to hurt. Such impulses are distressing and it is uncommon for people to act on them. It is important to distinguish obsessional thoughts from thought insertion, a first rank symptom of schizophrenia, in which the patient believes they are experiencing thoughts that are not their own. In contrast, obsessional thoughts are always recognised as arising from the patient’s own mind.
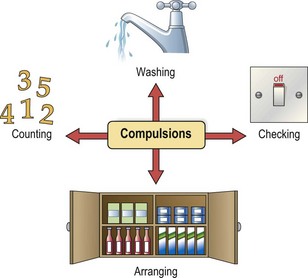
Compulsions consist of a strong urge to perform an action or complex series of actions repeatedly, even though they are recognised as unnecessary. Compulsions can often be resisted for short periods, but this is usually associated with increasing levels of anxiety that can only be relieved by performing the compulsive act. Compulsions can take very many forms (Fig. 2), but the commonest are:
 checking, e.g. returning home again and again to check the oven has been turned off or the door is locked
checking, e.g. returning home again and again to check the oven has been turned off or the door is locked< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree