Obstructive Sleep Apnea: Surgical Treatment
Kasey K. Li
The exact etiologic factors of obstructive sleep apnea (OSA) syndrome have not been clearly elicited. However, it is well recognized that a disproportionate anatomy of the upper airway exists in OSA, leading to obstruction during sleep (1,2). Although continuous positive airway pressure (CPAP) is the current mainstay of treatment, there are clear limitations to its use. Patient compliance remains a major problem, and the long-term use of CPAP is an unrealistic expectation for many patients (3,4 and 5). Surgery has always played an integral part in the management of OSA. In fact, the first treatment of OSA was the use of tracheostomy to bypass upper-airway obstruction in “Pickwickian” patients (6). Although tracheotomy remains the most successful surgical treatment, patient acceptance is extremely low due to the associated morbidity and social implications.
In 1979, Fijita et al. (7) reported the use of uvulopalatopharyngoplasty (UPPP) for the treatment of OSA. Although the procedure has proved to be an excellent method for improving the oropharyngeal airway obstruction, only approximately 40% of patients respond successfully to this procedure (8). The lack of success is primarily due to other untreated sites of obstruction in the airway. There are potentially three major regions of obstruction: the nose, the palate (oropharynx), and the tongue base (hypopharynx). In addition, the lateral pharyngeal wall has been increasingly recognized as one of the major factors in upper-airway collapse (9). Certain craniofacial features identified by cephalometric analysis have also been suggested as risk factors (10,11). In the early 1980s, several investigators reported that mandibular deficiency contributed to the development of OSA. With the increased recognition that hypopharyngeal airway obstruction is a major contributing factor of OSA, genioglossus and hyoid advancement (HA) were later developed to improve treatment outcomes (12,13). Subsequently, mandibular advancement by surgical means has been shown to improve airway obstruction (14,15). To maximize the extent of mandibular advancement, concurrent maxillary advancement was subsequently advocated (16). Today, many surgical procedures have been developed to expand the airway and/or to reduce the collapsibility of the airway (Table 21-1).
Despite the availability of numerous surgical procedures for the treatment of OSA, proper selection of the procedure(s) that would be the most beneficial for an individual patient remains difficult. Moreover, the complex interplay of the soft and hard tissues that contributes to upper-airway obstruction, the crucial role of this anatomic region to speech and swallowing, as well as the subsequent edematous response after surgical intervention present a formidable challenge to the sleep surgeon. Therefore, a logical and systematic approach to clinical evaluation, treatment planning, surgical execution, and perioperative management is necessary to maximize safety and improve outcomes.
CLINICAL EVALUATION
Clinical evaluation must include the overall body habitus (height, weight, and neck circumference), since it has been shown that the surgical outcomes can be influenced by these factors (17). Obviously, a detailed examination should be focused in the head and neck region to identify the potential sites of upper-airway obstruction, including the nose, the soft palate, the lateral pharyngeal walls, and the tongue base. The presence of nasal septal deviation, turbinate hypertrophy, nasal valve collapse, elongation of the soft palate/uvula, tonsillar hypertrophy,
enlargement of the tongue, and narrowing of the maxilla/mandible or mandibular/midface deficiency (small or hypoplastic) are some of the most common findings in patients with OSA.
enlargement of the tongue, and narrowing of the maxilla/mandible or mandibular/midface deficiency (small or hypoplastic) are some of the most common findings in patients with OSA.
TABLE 21-1 COMMON OSA SURGICAL PROCEDURES | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||
Fiberoptic Nasopharyngolaryngoscopy
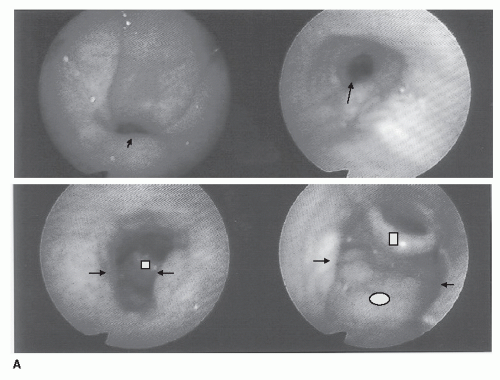
Airway examination by a fiberoptic scope is highly recommended in patients with OSA. This evaluation enables the examiner to directly visualize the entire upper airway from the nose to the larynx. The dimension of the nasal, retropalatal, and retroglossal airway can be fully assessed.
Furthermore, the prominence of the tongue base and the lateral pharyngeal wall and the pattern of obstruction, as well as their collapsibility, can be evaluated with the Muller’s maneuver (Fig. 21-1) (18).
Lateral Cephalometric Radiograph
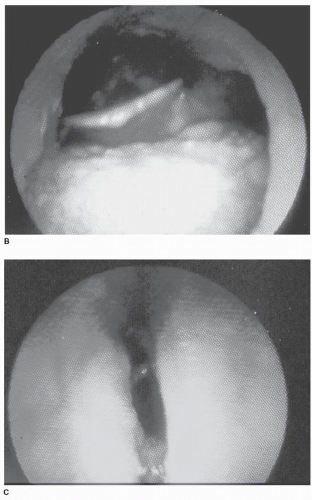
Many airway imaging methods are currently available. Computed tomography (CT) or magnetic resonance imaging (MRI) can precisely assess the dimension of the upper airway (9,19). However, because of cost constraints, none can be widely used in clinical practice, except the lateral cephalometric radiograph. Although lateral cephalometric radiograph is only a static two-dimensional method of evaluating a dynamic three-dimensional area, it is a valuable study to identify abnormal facial skeletal anatomy that may contribute to airway obstruction, as well as the relation of the hard and soft tissues of the airway (Fig. 21-2). Furthermore, lateral cephalometric radiograph provides useful information on the posterior airway space behind the soft palate and the tongue base. The posterior airway space measurement on lateral cephalometric radiograph has been shown to correlate with the volume of the hypopharyngeal airway on three-dimensional CT scans (20).
SURGICAL PLANNING
Since multiple sites of obstruction can be involved in OSA, surgical intervention must take place at different levels. Therefore, individual procedures for specific area(s) of obstruction have been developed. The ultimate goal of surgical management is to improve the entire upper airway, achieving total upper-airway reconstruction. Consequently, the identification of the sites of obstruction based on clinical examination, fiberoptic nasopharyngoscopy, and lateral cephalometric radiographs is essential for proper surgical planning.
OVERVIEW OF SURGICAL PROCEDURES
Tracheotomy
As stated earlier, tracheotomy is the first surgical treatment for OSA (6). Tracheotomy differs from all other surgical interventions for OSA because it bypasses the entire upper airway, thus achieving a success rate that is unsurpassed by any other procedures. However, because of poor patient acceptance, it is now performed only in patients with severe OSA when nasal CPAP/bilevel positive airway pressure or other surgical treatments have failed or as a temporary measure for airway protection while the patient is undergoing other airway reconstructive procedures.
Nasal Reconstruction
The patency of the nasal airway is important for normal respiration; furthermore, nasal obstruction has been implicated in OSA (21). Nasal obstruction during sleep may result in increased oral breathing and mouth
opening, thus leading to airway obstruction due to the rotation of the mandible and the retrodisplacement of the tongue base back to the pharynx. Nasal obstruction may also inhibit the optimal use of nasal CPAP. Therefore, the use of nasal surgery to improve nasal CPAP use should be considered. Three anatomic areas of the nose that require examination are the alar cartilage/nasal valve region, the septum, and the turbinates (Table 21-2). One of the least invasive procedures to improve nasal breathing has been the use of temperature-controlled radiofrequency (TCRF) energy to reduce hypertrophic turbinates (22). This technique alone may potentially improve nasal CPAP use.
opening, thus leading to airway obstruction due to the rotation of the mandible and the retrodisplacement of the tongue base back to the pharynx. Nasal obstruction may also inhibit the optimal use of nasal CPAP. Therefore, the use of nasal surgery to improve nasal CPAP use should be considered. Three anatomic areas of the nose that require examination are the alar cartilage/nasal valve region, the septum, and the turbinates (Table 21-2). One of the least invasive procedures to improve nasal breathing has been the use of temperature-controlled radiofrequency (TCRF) energy to reduce hypertrophic turbinates (22). This technique alone may potentially improve nasal CPAP use.
TABLE 21-2 CONSIDERATIONS FOR NASAL RECONSTRUCTION | |||
|---|---|---|---|
|
TABLE 21-3 CONSIDERATIONS FOR UPPP/UPF | |||
|---|---|---|---|
|
Oropharyngeal Reconstruction
Uvulopalatopharyngoplasty
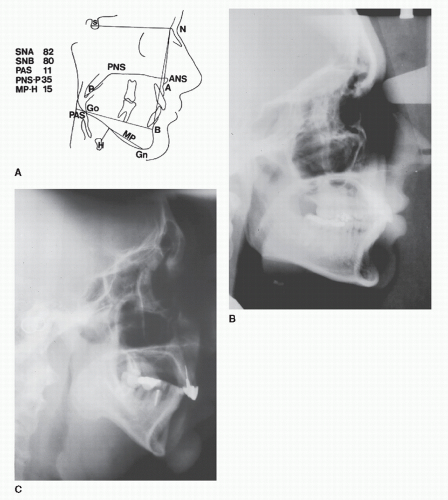
Popularized by Fijita (7), UPPP improves oropharyngeal obstruction (Table 21-3). This procedure was originally thought to be an alternative to tracheotomy in OSA. It is easily performed under general anesthesia and consists of the removal of a portion of the soft palate, the uvula, and a limited amount of the lateral pharyngeal wall (Fig. 21-3). The tonsillar tissues are also removed, if present. The temptation to improve results by removing an excessive amount of tissue should be resisted because the potential complications will dramatically increase. Since UPPP only addresses the oropharyngeal obstruction, its success rate is only approximately 40% (8).
Uvulopalatal Flap
The uvulopalatal flap (UPF) is a modification of the UPPP (Fig. 21-4) (23). The goal of the modification is to reduce the potential complications of UPPP, including nasopharyngeal incompetence, nasopharyngeal stenosis, and dysphagia. The procedure involves the retraction of the uvula superiorly toward the hard—soft palate junction after a limited removal of the uvula, the lateral pharyngeal wall, and the mucosa. This results in a widening of the oropharyngeal airway.
Laser-assisted Uvulopalatoplasty
Laser-assisted uvulopalatoplasty (LAUP) was introduced by Kamimi as an office-based surgical procedure for the treatment of snoring (24). The procedure involves the removal of the uvula and a portion of the soft palate by carbon dioxide laser incisions and vaporization. Most of the uvula is amputated and the soft palate, 1 to 2 cm lateral to the uvula, is incised and vaporized. In addition, mucosal or tonsillar pillar tissue is vaporized as needed.
Although many studies have evaluated the efficacy of LAUP in the treatment of OSA, most of the studies are flawed by methodologic discrepancies or statistical inadequacies, such as ill-defined criteria for response and lack of adequate follow-up. A recent American Academy of Medicine practice parameter paper stated that there was insufficient efficacy to recommend the LAUP in the treatment of OSA (25).
Hypopharyngeal Reconstruction
Genioglossus Advancement
The tongue and the lateral pharyngeal wall can significantly obstruct the airway during sleep. Genioglossus advancement (GA) was the first procedure to specifically address tongue obstruction in OSA (Table 21-4) (12). The initial rationale for this surgical approach was based on the findings that patients with OSAs have decreased posterior airway space and increased distance between the mandible and the hyoid.
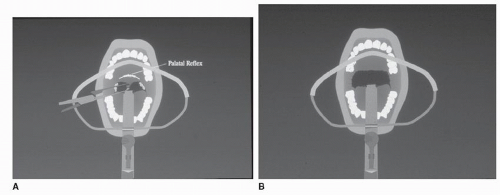
These measurements, along with the polysomnographic data, have been shown to improve after surgery. With increasing understanding that the genioglossus muscle plays an important role in nocturnal airway obstruction (26,27), an improved incorporation of the genioglossus muscle in the advanced portion of the mandible was developed (28). GA does not alter the shape of the mandible but only brings the attachment of the genioglossus forward. This advancement places tension on the tongue musculature, thus limiting the posterior displacement during sleep. The current GA procedure is performed completely intraorally. The mucosal incision is made just below the mucogingival junction, and a subperiosteal flap is reflected to expose the anterior mandible and mental nerves. The genial tubercle and genioglossus muscle can be identified by finger palpation in the floor of the mouth and with the aid of the lateral cephalometric radiograph. A rectangular osteotomy is made to incorporate the geniotubercle. The geniotubercle is advanced and partially rotated to prevent retraction back into the floor of the mouth (Fig. 21-5).
These measurements, along with the polysomnographic data, have been shown to improve after surgery. With increasing understanding that the genioglossus muscle plays an important role in nocturnal airway obstruction (26,27), an improved incorporation of the genioglossus muscle in the advanced portion of the mandible was developed (28). GA does not alter the shape of the mandible but only brings the attachment of the genioglossus forward. This advancement places tension on the tongue musculature, thus limiting the posterior displacement during sleep. The current GA procedure is performed completely intraorally. The mucosal incision is made just below the mucogingival junction, and a subperiosteal flap is reflected to expose the anterior mandible and mental nerves. The genial tubercle and genioglossus muscle can be identified by finger palpation in the floor of the mouth and with the aid of the lateral cephalometric radiograph. A rectangular osteotomy is made to incorporate the geniotubercle. The geniotubercle is advanced and partially rotated to prevent retraction back into the floor of the mouth (Fig. 21-5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree