Obstructive Sleep Apnea: Treatment Overview and Controversies
Nancy A. Collop
WHO TO TREAT?
Defining what constitutes obstructive sleep apnea (OSA) can be challenging. Possible definitions may include the following: use of a polysomnographically defined threshold respiratory disturbance index (RDI) or apnea-hypopnea index (AHI), combining an RDI or AHI with an assessment of subjective sleepiness, or the use of an RDI or AHI with some evidence of end-organ dysfunction such as hypertension. Different definitions will be useful depending upon the purpose. When deciding to treat individual patients, there are a number of considerations that may come into account, which will be outlined in this chapter. The comments in the beginning of the chapter pertain to adult OSA; later sections will deal with pediatric OSA.
Disordered Breathing Indices
The severity of OSA is typically defined by the use of disordered breathing indices (1). There are a number of different types of breathing events, and they may have different significance with regard to physiologic effects. The strict definitions of these events have varied over the years; however, in 2007, the American Academy of Sleep Medicine released “The AASM Manual for the Scoring of Sleep and Associated Events” (2). This was important as the manual defined recommended standards for sleep centers on equipment, filter settings, and scoring of sleep studies. Adoption of these standards should decrease the variability in scoring events between laboratories. Nonetheless, counting events to define severity remains problematic on several fronts. There is little correlation between these respiratory disturbance indices and sleepiness (3). Furthermore, it has not been shown to correlate well with the quality-of-life measure or other disease-specific outcomes (4). This may in part be related to the equivalence of the events in the index. All events may not result in comparable physiologic responses, for example, a 45-second apnea in rapid eye movement (REM) may result in cardiac arrhythmias, severe oxygen desaturation, and marked blood pressure fluctuation; however, it would have equal weight with a hypopnea that caused an oxygen desaturation from 95% to 91%.
Another issue is that sleep centers may use different equipments to measure respiratory variables. Again, the manual should be very helpful in standardizing the equipment between sleep centers (2).
To summarize, using a polysomnographically defined AHI alone is fraught with problems and should not be used in isolation to determine the diagnosis and management of a patient with OSA.
REM/Positional OSA
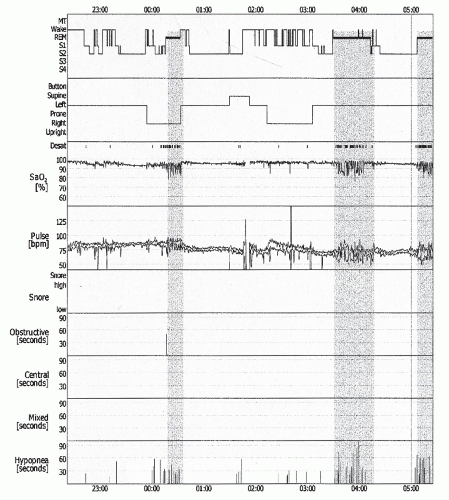
Another issue relates to treating disease that may be confined or particularly severe in one stage of sleep (usually REM), but is not significant overall, based on total sleep time (TST). REM-related OSA is an understudied phenomenon. It is well known that obstructive sleep-disordered breathing (SDB) is worse (longer events and lower oxygen desaturations) in REM sleep because of a more collapsible upper airway (muscle atonia) and a blunted response to chemical stimuli (5). It is clear that some patients have most of their SDB during this stage of sleep (Fig. 19-1). This phenomenon of REM-related OSA is
three times more common in women than in men (6,7). This is likely due to inherent differences in the upper airway between men and women (8). It is also more likely to occur in younger populations and less-obese patients (9). There are conflicting data as to whether REM-related OSA alone can result in significant daytime sleepiness (10,11). It has been shown that pulmonary artery pressures are more elevated during REM- than nonrapid eye movement (NREM)-related events, even after adjusting for oxygen saturation levels (12). However, no data exist as to whether REM-related OSA can cause long-term morbidity or mortality. Therefore, there is little to guide us as to how to treat this condition.
three times more common in women than in men (6,7). This is likely due to inherent differences in the upper airway between men and women (8). It is also more likely to occur in younger populations and less-obese patients (9). There are conflicting data as to whether REM-related OSA alone can result in significant daytime sleepiness (10,11). It has been shown that pulmonary artery pressures are more elevated during REM- than nonrapid eye movement (NREM)-related events, even after adjusting for oxygen saturation levels (12). However, no data exist as to whether REM-related OSA can cause long-term morbidity or mortality. Therefore, there is little to guide us as to how to treat this condition.
Similar to REM-related OSA, it is commonly observed that patients have worsening of both frequency and number of SDB events when they are in the supine position. There are subgroups of patients that have OSA only when supine (13). They tend to be both thinner and younger than “nonpositional” patients with OSA, which leads one to wonder whether, with time, some of these patients may progress to the “nonpositional” status. Although there are significantly more data on this phenomenon than on REM-related OSA, little data exist on long-term effects on those patients whose SDB is predominantly in the supine position. There are treatment options aside from nasal continuous positive airway pressure (CPAP) in these patients, as will be discussed later.
Symptoms
Sleepiness
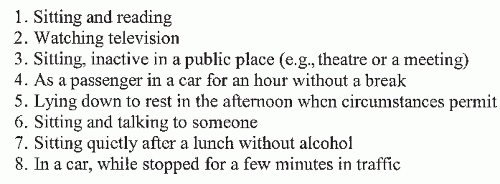
Another way to determine the “severity” of a patient’s OSA, aside from measurement of events during polysomnography (PSG), is to evaluate his or her degree of symptomatology (Table 19-1). Since many patients with OSA are sleepy, one method of evaluating the severity of disease is by either subjectively or objectively measuring sleepiness. Subjective measures of sleepiness include validated patient questionnaires such as the Stanford sleepiness scale (14) or the Epworth sleepiness scale (ESS) (15,16) (Fig. 19-2). These scales allow the physician to see how sleepy the patient feels and loosely correlate this with the degree of sleepiness as measured by objective measures (17). The multiple sleep latency test (MSLT) and the maintenance of wakefulness test (MWT) are two such objective measures of sleepiness. The MSLT measures
how long it takes the patient to fall asleep during a series of four to five daytime naps after overnight PSG documenting adequate sleep the prior night. If the mean sleep latency is <5 minutes, it is consistent with severe daytime sleepiness present. If the mean sleep latency is from 5 to 10 minutes, it is also considered abnormal and suggestive of excessive sleepiness. Mean sleep latencies >10 minutes are considered normal. Interestingly, it has been shown that with effective treatment, many patients with OSA will improve but not “normalize” their MSLTs (18,19).
how long it takes the patient to fall asleep during a series of four to five daytime naps after overnight PSG documenting adequate sleep the prior night. If the mean sleep latency is <5 minutes, it is consistent with severe daytime sleepiness present. If the mean sleep latency is from 5 to 10 minutes, it is also considered abnormal and suggestive of excessive sleepiness. Mean sleep latencies >10 minutes are considered normal. Interestingly, it has been shown that with effective treatment, many patients with OSA will improve but not “normalize” their MSLTs (18,19).
TABLE 19-1 COMMON SYMPTOMS ASSOCIATED WITH ADULT OSA | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
The MWT measures the ability of the patient to stay awake rather than fall asleep. This test is often used for patients with sleep disorders working in occupations that require vigilance, such as truck drivers and airplane pilots. The test is performed similar to an MSLT, except that the patient is monitored for sleep onset over a 40-minute period. Normative values suggest that a patient should be able to stay awake for all 40 minutes (20). Unfortunately, comparison studies of Epworth and MWT have not shown good concordance in OSA (21). The degree of motivation likely plays an important role in the MWT results, which brings its usefulness into question (22).
Other tools used to assess neurophysiological detriment related to OSA include functional outcome of sleep questionnaire (FOSQ) (23), symptoms of nocturnal obstruction and related events (SNORE 25) (24), and Calgary sleep apnea quality of life index (SAQLI) (25). These are often used to follow the response to therapy.
It has been shown that at-fault motor vehicle accidents occur more frequently in patients with OSA (26,27). One may assume that significant sleepiness might select out those who drive as part of their profession, but one study showed that 8.6% of professional truck drivers had OSA (28). Simulated driving tests in patients with OSA have shown worse performance compared with controls, which can be improved with the use of CPAP (29,30). It may be possible to stratify patients with OSA for driving risk by using these devices; however, the results to date are conflicting (31,32). At any rate, it is imperative that physicians screening patients for OSA query them about falling asleep or nodding while driving (33).
In summary, subjective or objective measures of sleepiness may be helpful in assisting the clinician to determine who to treat, especially if the degree of SDB is low, and also, to follow response to therapy.
Other
Many patients are referred to sleep clinics for sleep apnea by their bed partner. The theory behind this is simple but unproven. Most sleep apnea patients are male (3:1 by most epidemiologic studies). Women, in general, are lighter sleepers; therefore, a snoring bed partner with apneas will be more likely to disrupt their sleep. Indeed the “spousal arousal syndrome” has been described (34). In addition, bed partner observation of breath pauses is one of the most sensitive historical items for OSA (35). It has also been shown, however, that if patients are referred by their spouse, they are less likely to be compliant with CPAP (36).
Although daytime sleepiness is the most common and clearly the most prominent complaint of OSA sufferers, other symptoms have been described. Chronic fatigue and tiredness, rather than true sleepiness, may be more common in females (37). Diminished neurocognitive function including the inability to maintain attention is frequently present in OSA. Studies have shown that measures of psychomotor vigilance are affected in OSA, and the degree of the decrement correlates with the AHI (38,39 and 40). Insomnia may be an underappreciated prevalent symptom of OSA (41). Morning headaches are found more frequently in patients with OSA, compared with other sleep disorders, presumably related to the hypoxemia and concomitant hypercapnia (42). Hypercapnia causes vasodilation of cerebral vessels, which may predispose to headaches. Sinus disease has been linked to SDB. Allergy sufferers are 1.8 times more likely to have SDB (43). Impotence is well described in OSA. In one study of over 1,000 men with
erectile dysfunction, almost 44% had an AHI of >5 (44). The reason for impotence in OSA is not well understood, although one study did suggest that it could be related to nerve dysfunction (45). Signs and symptoms of OSA, aside from sleepiness, may be present and should be looked for in the assessment of individual patients.
erectile dysfunction, almost 44% had an AHI of >5 (44). The reason for impotence in OSA is not well understood, although one study did suggest that it could be related to nerve dysfunction (45). Signs and symptoms of OSA, aside from sleepiness, may be present and should be looked for in the assessment of individual patients.
Cardiovascular Disease
In the past decade, a number of cardiovascular diseases have been shown to occur frequently in association with OSA (Table 19-2). Although these are mostly associations, epidemiologic studies would suggest that many of these associations are more than coincidental. Perhaps the most studied cardiovascular disease associated with OSA is systemic hypertension. It has been shown that approximately 30% of the patients in essential hypertension clinics have OSA (46,47 and 48), and it is estimated that 50% to 60% of patients with OSA have hypertension (49). The difficulty with showing causality, that is, OSA can cause hypertension, lies in the fact that the population having hypertension is similar to the population having OSA: middle-aged, overweight males. Animal models have been instructive in showing that both recurrent apneas and hyporemia during sleep will result in elevated blood pressure over time (50,51 and 52). Two large epidemiologic studies, one longitudinal and the other cross-sectional, showed an increasing dose response for the severity of OSA, defined by AHI and the presence of hypertension (53,54). Another study showed that patients with refractory hypertension, defined by persistent elevation of blood pressure, despite the use of three or more antihypertensives, had a very high prevalence of OSA—96% of men and 65% of women (55).
It is generally agreed upon that treatment of OSA improves hypertension. Two meta-analyses from reviewed randomized, controlled trials compared CPAP with placebo. Bazzano et al. (56) evaluated 16 trials ranging from 2 to 24 weeks in length. They found an overall mean net change of -1.83 mm Hg (95% CI: -3.05 to -0.61) in diastolic blood pressure (DBP) and a mean net change of -2.46 mm Hg (95% CI: -4.31 to -0.62) in systolic blood pressure (SBP). Haentjens et al. (57) evaluated 12 trials, 10 of which were included in the Bazzano article, and found a mean net change of -1.79 mm Hg (95% CI: -2.87 to -0.71) in DBP and of -1.77 mm Hg (95% CI: -3.00 to -0.54) in SBP. In general, most articles suggest that patients with a higher AHI had a more marked change in blood pressure.
TABLE 19-2 CARDIOVASCULAR DISEASES ASSOCIATED WITH ADULT5 OSA | |||||
|---|---|---|---|---|---|
|
Another cardiovascular disease associated with OSA is pulmonary hypertension. This has been shown to be present in approximately 15% to 20% of the patients with OSA (58,59). In patients with OSA, it tends to be mild (average mean pulmonary artery pressures of 20-25 mm Hg) or exercise induced. It is controversial whether pulmonary hypertension can occur in OSA independent of obesity or underlying lung disease (60,61). It has, however, been shown that the treatment of OSA can improve pulmonary hemodynamics (62,63 and 64). The long-term effects of pulmonary hypertension on the course of patients with OSA are unknown.
Aside from systemic and pulmonary hypertension, other cardiovascular diseases have been associated with OSA, including coronary artery disease (CAD) and stroke. It has been shown that patients with OSA have elevated levels of risk markers such as C-reactive protein (65), leptin (66), and homocysteine (67), all of which have been associated with increased risk of cardiovascular disease. Case control studies of male and female patients who have had recent acute coronary syndrome show an association between the conditions with significantly elevated odds ratios (68,69). Nocturnal arrhythmias are also common in patients with OSA. The risk of arrhythmia with OSA appears to be related to severity. Analysis of electrocardiographic recordings during sleep studies in >450 patients showed a 58% (vs. 42% in patients without OSA) prevalence of arrhythmias in patients with OSA, with most arrhythmias occurring in those with an AHI of >40 per hour (70). Bradycardia, sinus pauses, and nocturnal paroxysmal asystole are the most common arrhythmias seen, and these increase in frequency with increasing severity of the syndrome. Nonsustained supraventricular tachycardias may also occur in patients with severe OSA; however, ventricular arrhythmias are very uncommon (71). Treatment of OSA with CPAP improves most nocturnal arrhythmias (72).
The risk for stroke appears to be even more compelling than the risk for CAD in patients with OSA. In the Sleep Heart Health study in which overnight PSG was done in >6,000 adults, the relative odds ratio of self-reported stroke was elevated when comparing the upper AHI quartiles with the lower ones (1.58) (73). It has also been shown that the prevalence of SDB is very high in patients with recent stroke or transient ischemic attack, in some series as high as 95% (74,75). Patients with concomitant OSA and stroke have been shown to have early neurologic worsening and oxygen desaturation compared with controls (76). One study suggests that those with stroke and OSA are at risk for higher mortality. Sahlin et al. (77) diagnosed OSA in 23 of 132 patients admitted for stroke rehabilitation and using those with an AHI of <15 as controls, individuals with OSA had a higher 10-year mortality, with an adjusted hazard ratio of 1.76.
In conclusion, deciding on when to treat a patient with SDB requires several considerations: (1) the severity of the condition as defined by the disordered breathing indexes or oxygen desaturation, understanding that there
is considerable variability from one sleep laboratory to the next; (2) the symptoms the patient has, and how those symptoms impact on day-to-day functioning; and (3) the presence of concomitant diseases, particularly cardiovascular diseases, namely, systemic hypertension, pulmonary hypertension, heart disease, and stroke.
is considerable variability from one sleep laboratory to the next; (2) the symptoms the patient has, and how those symptoms impact on day-to-day functioning; and (3) the presence of concomitant diseases, particularly cardiovascular diseases, namely, systemic hypertension, pulmonary hypertension, heart disease, and stroke.
OVERVIEW OF TREATMENT OPTIONS
This section will provide a brief overview of the various treatments that have been attempted in OSA (Table 19-3). Later chapters will provide a more in-depth review of specific treatments.
Positive Pressure Devices
Nasal CPAP has become the current treatment of choice for the majority of adult patients with OSA. The mechanism by which nasal CPAP works is predominantly by creating a “pneumatic splint” in the upper airway, hence, preventing collapse (78). Other effects of CPAP include diminishing muscle tone in the upper airway and increasing functional residual capacity (79,80). The pressure required by an individual patient is usually determined during a sleep study, in which the pressure is gradually increased until obstructive events and snoring are eliminated and oxygen saturation is maintained above 90%. Nasal CPAP has been shown to be very successful in the treatment of OSA. Approximately 95% of the patients can be definitively treated with this device, including patients with mild disease (81). Nasal CPAP has been shown to improve many aspects of the OSA syndrome including daytime sleepiness (82) and quality of life (83), and after the initiation of CPAP, patients with OSA have fewer hospitalizations (84). An excellent review of all the randomized trials comparing CPAP with placebo or other treatments in adults is published in the Cochrane Library (85). This review concluded that although CPAP is more effective than placebo in improving sleepiness, multiple quality of life measures, and health status, further work is required to determine which specific groups of patients are most likely to benefit, how much benefit can be obtained, and at what cost.
TABLE 19-3 TREATMENTS FOR ADULT OSA | ||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||
The biggest drawback of nasal CPAP is the adherence to nightly usage. Originally, physicians had to depend upon patient’s report regarding usage. However, with the advent of CPAP machines containing timers to measure hours of usage, it was found that the apparatus is used an average of 5 hours per night (86,87 and 88). Depending on the definition of compliance to therapy, 46% to 89% of the patients continue to use their nasal CPAP after obtaining it (89,90 and 91). A number of techniques have been used to try to improve adherence to CPAP. However, no one measure has been shown to consistently do so. Such efforts include the following: giving patients proper instruction and follow-up on the use of the apparatus (92,93), assuring mask fit and comfort is maximal (94), and humidification to decrease dryness (95). A new feature for many CPAP devices is expiratory pressure relief. Internal monitoring that senses when the patient switches from inhalation to exhalation allows a decrease in the CPAP level during exhalation without any substantial impact on the efficacy of CPAP. Studies have shown improved tolerance of CPAP and increased usage over the short term, but longer-term acceptance has not been proven in studies to date (96,97).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree