Oncologically Appropriate Surgery in the Treatment of Primary Bone Tumors of the Spine: Correct Terminology, Planning and Results
Stefano Boriani
Stefania Paderni
Michele Cappuccio
Alessandro Gasbarrini
Luca Boriani
Stefano Bandiera
ABSTRACT
Background
The so-called limb-salvage surgery based on the Enneking staging system allowed excellent results in the treatment of bone tumors of the limb.
Methods
We evaluated the possibility to extend to the spine the same oncologic criteria accepted for bone tumors of the limbs. A series of 125 en bloc resections for 467 primary tumors of the spine was reviewed to assess the relation among the tumor aggressiveness, the surgical margins, and the outcome
Results
The rate of local control after en bloc resection was 70.4% at 89 months’ average follow-up, ranging from 90.7% in intact cases to 54.8% in previously treated cases. For a better assessment of the results, these were explored by diagnosis. Full local control was achieved in 11 en bloc resections performed in a series of 31 stage 3 giant cell tumors (GCTs) at 6 to 172 months’ follow-up. In a series of 35 stage IA/B chondrosarcomas, full local control was achieved in 12 en bloc resections with appropriate margins at 6 to 168 months’ follow-up, whereas in eight cases with tumor contamination (intralesional margin), the success rate was 62.5% at 30 to 165 months. In osteosarcoma (osteogenic sarcoma; OGS), the combination of appropriate margin and a full course of multiple-drug chemotherapy is critical (six cases: no local recurrences at 24 to 108 months), whereas inappropriate margins, incomplete chemotherapy, and chemotherapy alone were always followed by a local recurrence.
Conclusions
En bloc resection is the procedure of choice in the treatment of aggressive benign and low-grade malignancies in the spine. High-grade tumors like OGS and Ewing sarcoma (ES) require combination of chemotherapy (in OGS and ES) and radiation (in ES) with en bloc resection to obtain the best results
INTRODUCTION
According to the criteria proposed by Enneking (7) and widely accepted among oncologists, “radical” resection is a thigh amputation when the tumor is located in the tibia. Unfortunately, many surgeons define “radical” as the excision they believe to be appropriate. These are mostly intralesional excisions performed without any consideration for oncologic principles. This incorrect use of the terminology prevents us from comparing results and sharing experiences.
The role of a common nomenclature in sharing information is obvious. Our proposal is to adopt the terminology proposed by Enneking (7) to describe surgical tumor excision, based on the margin achieved. The margin is a shell of healthy tissue all around the tumor mass, the width of which (marginal, only the tumor pseudocapsule; wide, a coverage of healthy tissue, like muscle or fascia, or layer, like pleura) is requested according to the oncologic stage (7).
The term radical means the resection of the whole compartment of tumor origin. In the spine, this is virtually impossible, as it should mean to resect en bloc the full vertebra (content of the canal included), provided that the tumor does not grow outside. In our series, even a five-vertebrae resection, including the cord, was performed, but it should be considered wide or even marginal, as in a small area, the tumor is covered only by the pleura. Further, the epidural space being an extracompartmental area, the tumor invasion of that space immediately makes inappropriate the term radical.
A full preoperative workup is mandatory for diagnosis and staging purpose and must be completed with a careful collection of clinical data and laboratory tests to confirm the patient’s suitability to major surgery. Advanced age and poor general conditions are relative contraindications and must be considered case by case with the anesthesiology team (6).
It is important to consider the role of magnetic resonance imaging (MRI) to evaluate the epidural extension and to find a cleavage between the tumor pseudocapsule and the dura. Some surgeons suggest (when needed) resection of the dura together with the tumor to enlarge the margins (1). The risk is to further increase the morbidity of such a long and difficult procedure, without absolute certainty of achieving an appropriate margin in case of epidural involvement of the tumor. Complications like cerebrospinal fluid (CSF) leakage, wound dehiscence, or infection may delay adjuvant treatments (like chemotherapy), which are mandatory in many conditions like ES or OGS.
The spillage of tumor in the tissues due to incisional biopsy may prevent adequate treatment, as it is seldom possible to resect the wound, especially the peridural scar. Previous surgery, as well as radioinduced fibrosis, increases the risk of intraoperative damage of structures in the perimeter of the tumor (ureter, vena cava, aorta, sympathetic chain).
The planning of the surgical treatment of a bone tumor of the spine must consider the extension of the tumor, the anatomic structures that cannot be resected or displaced, and the possibilities of different surgical approaches. Three surgical procedures have been identified and described according to an original surgical staging system (4), based on the division into 12 sectors and five layers of the transverse section of the vertebra, which should allow standardization of the approach to these tumors.
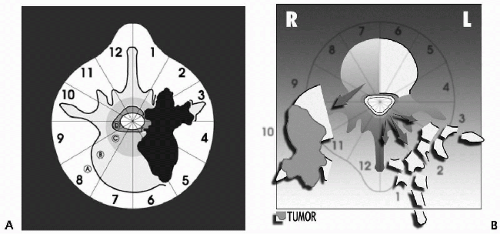
Vertebrectomy is a surgical procedure performed by double approach (first posterior, second posterior combined with anterior) (Fig. 12.1A and B), aiming to achieve en bloc
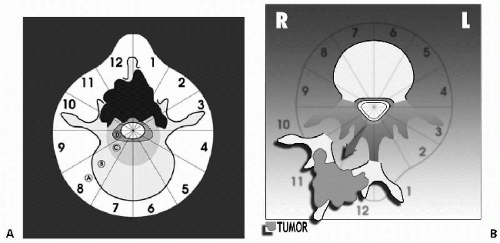
resection of the vertebral body (sectors 4 to 8 or 5 to 9). The vertebral body can be resected by a posterior approach alone (10,13) in the thoracic spine, but the procedure will be oncologically appropriate only if the tumor is not expanding in layer A (Fig. 12.2A and B). In this case, this technique (10,13) exposes to violate the margin. The anterior step of the procedure will permit leaving a sheet of continuous healthy tissue over the tumor (5).
resection of the vertebral body (sectors 4 to 8 or 5 to 9). The vertebral body can be resected by a posterior approach alone (10,13) in the thoracic spine, but the procedure will be oncologically appropriate only if the tumor is not expanding in layer A (Fig. 12.2A and B). In this case, this technique (10,13) exposes to violate the margin. The anterior step of the procedure will permit leaving a sheet of continuous healthy tissue over the tumor (5).
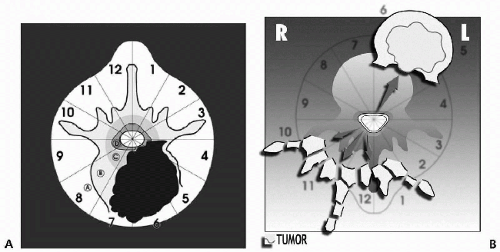 FIGURE 12.1 A: Indication for en bloc resection of the vertebral body according to the WBB system (4). The transverse extension of the tumor is described with reference to 12 radiating zones (numbered 1 to 12 in clockwise order, starting from the left side) and to five concentric layers (A to E). B: When the tumor invades layer A, a double approach is suggested to allow direct visualization of the tumor. |
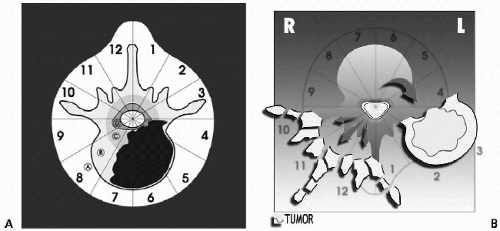 FIGURE 12.2 A, B: If the tumor is contained in the vertebral body (no layer A invasion), a single posterior approach (20,28) is appropriate. |
Sagittal resection is as well performed by a double approach: the target is to remove en bloc an eccentrically growing tumor (sectors 2 to 5/6 or 7/8 to 11) (Fig. 12.3A and B).
Posterior resection is performed by a simple posterior approach: the criterion for an appropriate margin is that sectors 4 and 9 must be free from tumor (Fig. 12.4A and B). The appropriateness of the procedures must be confirmed by the pathologist, who will dictate the margins achieved (wide, marginal, intralesional) for prognostic evaluation and for indications for adjuvant therapies.
The oncologic approach to bone tumor of the spine by en bloc resection was started in the 1970s by B. Stener (11) and R. Roy-Camille (10), who first described surgical techniques of en bloc resection in the thoracic and lumbar spine with an appropriate oncologic view. K. Tomita (13) later described a similar technique of vertebrectomy by posterior approach in the thoracic and lumbar spine. Recently, en bloc




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree