Operations and Procedures
 Intraoperative Dyes
Intraoperative Dyes
1. Matching. Match the intraoperative dyes with their characteristics. |
| G7 p.144:70mm |
Dyes: |
|
|
|
| |
Characteristic: |
|
|
a. carries a small risk of seizures when administered intrathecally |
|
|
b. is cytotoxic and should not be used at all |
|
|
c. can be used to demonstrate arteriovenous malformation (AVM) vessels intraoperatively |
|
|
d. used to identify cerebrospinal fluid (CSF) leaks and is considered safe |
|
|
 Surgical Hemostasis
Surgical Hemostasis
2. Bone wax inhibits_____formation. | bone | G7 p.146:82mm |
3. True or False. The following chemical hemostatic agent exerts its effect by promoting platelet aggregation: |
| G7 p.146:100mm |
a. Gelfoam (gelatin sponge) | false |
|
b. Oxycel (oxidized cellulose) | false |
|
c. Avitene (microfibrillar collagen) | true (Avitene, that is, microfibrillar collagen, provides platelet adhesion and aggregation. It loses its effectiveness with severe thrombocytopenia less than 10,000/mL.) |
|
d. thrombin | false | |
4. Matching. Match the surgical hemostasis substance with its trade name. |
| G7 p.146:100mm |
Trade name: |
|
|
|
|
|
Substance: |
|
|
a. gelatin sponge |
|
|
b. oxidized cellulose |
|
|
c. regenerated cellulose |
|
|
d. microfibrillar collagen |
|
|
e. thrombin |
|
|
5. Complete the following about surgical hemostasis. |
| G7 p.146:139mm |
a. What may thrombin cause if placed on the brain? | significant edema |
|
b. If the_____has been_____. | the pia; disrupted |
|
 Intraoperative Brain Swelling
Intraoperative Brain Swelling
6. Complete the brain swelling intraoperative checklist. |
| G7 p.147:25mm |
Hint: decompress |
|
|
a. d_____ _____ | drain CSF |
|
b. e_____ _____ | elevate head |
|
c. c_____(_____) | CO2 (hypercarbia) |
|
d. o_____of_____ _____ | obstruction of jugular veins |
|
e. m_____ | mannitol |
|
f. p_____ | pyperventilate |
|
g. r_____ _____ | remove bone |
|
h. e_____ _____ | excise brain (temporal or frontal lobes) |
|
i. (s) |
|
|
j. (s) |
|
|
 Craniotomies
Craniotomies
7. Complete the following regarding the risks of craniotomy: |
| G7 p.147:140mm |
a. increased neurological deficit _____% | 10% |
|
b. postop hemorrhage_____% | 1% |
|
c. infection_____% | 2% |
|
d. anesthetic complications_____% | 0.2% |
|
8. Complete the following regarding anticonvulsants. |
| G7 p.148:117mm |
a. True or False. Maintain their use if cortical incision is anticipated. | true (use Keppra) |
|
b. Describe the method of loading. | 500 mg PO or IV q 12 hours |
|
c. For supratentorial craniotomy maintain for_____. | 2 to 3 months | |
d. For cortical incision maintain for_____. | 2 to 3 months |
|
e. For aneurysm, AVM, or meningioma maintain for_____. | 6 to 12 months |
|
f. For head injury (see Head Injury guidelines) use for_____. | 1 week |
|
9. True or False. The following might be caused by pneumocephalus: |
| G7 p.149:48mm |
a. lethargy | true |
|
b. confusion | true |
|
c. headache | true |
|
d. nausea | true |
|
e. vomiting | true |
|
f. seizures | true |
|
10. True or False. Simple pneumocephalus (the presence of air in the cranium not apparently under pressure) can cause neurologic symptoms postoperatively. | true | G7 p.149:52mm |
11. Possible symptoms include l_____, c_____, h_____, n_____, v_____, and s_____. | lethargy, confusion, severe headache, nausea, vomiting, and seizures (Obviously, other etiologies, including subclinical seizures, and metabolic causes should be ruled out.) | G7 p.149:52mm |
12. Symptoms usually improve over_____days. | 1to3 | G7 p.149:62mm |
13. If postoperative seizures occur, consider the following: |
| G7 p.149:100mm |
Hint: abci |
|
|
a. a_____ _____ | anticonvulsant level—draw blood |
|
b. b_____ | bolus—additional anticonvulsants |
|
c. c_____ _____ | CAT scan—to identify if any cause |
|
d. i_____ | intubate—to protect airway |
|
 Posterior Fossa Craniotomy
Posterior Fossa Craniotomy
14. True or False. The correct treatment for air embolism sustained during a craniotomy performed with the patient in a sitting position is |
| G7 p.153:120mm |
a. to find and occlude site of entry or rapidly pack wound with sopping wet sponges | true |
|
b. bilateral or right-sided jugular venous compression | true | |
c. ventilation with 100% O2 | true |
|
d. rotating the patient right side down | false (Patient should be turned left side down to trap air in the right atrium.) |
|
e. aspirating air from central venous pressure (CVP) catheter | true |
|
f. avoiding positive end-expiratory pressure (PEEP), which is ineffective and may worsen the risk of paradoxical air embolism | true |
|
15. Complete the following about posterior fossa craniectomy and air embolism: |
| G7 p.153:130mm |
a. Effect of air in right atrium is |
|
|
i. h_____ | hypotension due to impaired venous return |
|
ii. a_____ | arrhythmias |
|
b. Paradoxical air embolism may occur if |
|
|
i. p_____ f_____ o_____ | patent foramen ovale |
|
ii. p_____arteriovenous (AV) f_____ | pulmonary AV fistula |
|
c. Incidence in sitting position is_____%. | 7 to 25% |
|
d. Precautions require |
|
|
i. D_____ _____ _____ | Doppler precordial ultrasound |
|
ii. C_____ _____ _____ _____ _____ | CVP catheter in right atrium |
|
e. Earliest clue to occurrence is_____. | fall in end tidal pCO2 |
|
16. How does air embolism cause problems? |
| G7 p.153:130mm |
a. Air becomes trapped in the_____ _____, | right atrium |
|
b. impairs_____ _____, and | venous return |
|
c. produces_____. | hypotension |
|
17. Outline the intraoperative treatment for air embolism during a craniotomy. |
| G7 p.153:145mm |
Hint: occlude |
|
|
i. o_____ | occlude entry site |
|
ii. c_____ | cover with wet laps |
|
iii. c_____ | compress jugular veins |
|
iv. l_____ | left side down lower head |
|
v. u_____ | ventilate/increase volume |
|
vi. d_____ | discontinue nitrous |
|
vii. e_____ | evacuate air |
|
18. Earliest clues to occurrence include |
| G7 p.154:20mm |
a. fall in_____ _____ _____ | end tidal pCO2 |
|
b. sound on Doppler is_____ _____ | machinery sound |
|
c. blood pressure_____ | hypotension | |
19. True or False. The following approach is most applicable for a vertebral endarterectomy. |
| G7 p.155:22mm |
a. midline suboccipital craniotomy | false |
|
b. extreme lateral posterior fossa approach | false |
|
c. paramedian suboccipital craniotomy | true (Paramedian suboccipital craniotomy gives decent access to the vertebral artery and to the posterior inferior cerebellar artery [PICA] and the vertebrobasilar junction.) |
|
d. subtemporal craniotomy | false |
|
20. Consider the concept of “5-5-5.” |
| G7 p.155:90mm |
a. i. This relates to the_____incision | skin |
|
ii. for a linear_____incision | paramedian |
|
iii. for access to the_____. | CPA |
|
b. |
|
|
i. The first number relates to the mm medial to the_____ _____. | mastoid notch |
|
ii. The second number relates to the_____ _____ the notch. | cm above |
|
iii. The third number relates to the _____ _____the notch. | cm below |
|
21. Matching. Match the incision with the objective. |
| G7 p.155:90mm |
Incision: |
|
|
|
|
|
a. the fifth nerve |
|
|
b. hemifacial spasm |
|
|
c. glossopharyngeal neuralgia |
|
|
d. microvascular trigeminal decompression |
|
|
e. vestibular schwannoma |
|
|
22. Location of the inferior margin of the transverse sinus can be estimated |
| G7 p.156:20mm |
a. to be_____f_____ _____ above the | two finger breadths |
|
b. m_____n_____. | mastoid notch |
|
23. Describe the Frazier burr hole. |
| G7 p.156:90mm |
a. It is used |
|
|
i. p_____ | prophylactically |
|
ii. to relive p_____ swelling | postoperative |
|
iii. due to h_____ or | hydrocephalus |
|
iv. e_____. | edema |
|
b. It is located |
|
|
i. _____to_____cm from the midline | 3 to 4 |
|
ii. _____to_____cm above the inion in adults | 6 to 7 |
|
iii. _____to_____cm above the inion in children | 3 to 4 | |
24. Complete the following regarding posterior fossa postop complications: |
| G7 p.157:120mm |
a. Respiratory: prevent by_____ | keeping patient intubated |
|
b. Hypertension: maintain SBP below with | 160 with nitroprusside |
|
c. Acute hydrocephalus: treat_____with_____ | ventricular tap—external ventricular drain (EVD) |
|
d. Meningitis: prevent by prompt repair of any_____ _____ _____ | cerebrospinal fluid (CSF) leak |
|
25. Blood pressure above_____is dangerous for the postoperative posterior fossa patient. | 160 mm Hg systolic | G7 p.157:148mm |
26. Complete the following regarding the posterior fossa: |
| G7 p.157:160mm |
a. Posterior fossa increased pressure is heralded by changes in |
|
|
i. b_____p_____ | blood pressure (increase) |
|
ii. r_____p_____ | respiratory pattern |
|
b. not by |
|
|
i. p_____i_____ | pupillary inequality |
|
ii. m_____s_____ | level mental status |
|
iii. l_____c_____ | ICP changes |
|
27. Considerations for postoperative posterior fossa emergency include |
| G7 p.158:20mm |
a. clinically |
|
|
i. blood pressure (BP)_____ | high |
|
ii. respirations_____ | labored |
|
b. recommended treatment |
|
|
i. i_____ | intubate |
|
ii. t_____ _____ | tap ventricle |
|
iii. o_____ _____ | open wound |
|
c. Should you |
|
|
i. obtain a computed tomographic (CT) scan first? | no |
|
ii. wait for operating room availability? | no |
|
28. Indicate whether increased pressure in the posterior fossa or supratentorial compartment produces a change in the following: |
| G7 p.158:30mm |
a. pupillary reflexes | supratentorial compartment |
|
b. level of consciousness | supratentorial compartment |
|
c. increase in intracranial pressure (ICP)_____ | supratentorial compartment |
|
d. changes in respiration_____ | posterior fossa |
|
e. rise in blood pressure_____ | posterior fossa |
|
 Pterional Craniotomy
Pterional Craniotomy
29. Matching. Match the head position with the location of the aneurysm. |
| G7 p.159:70mm |
Head position: |
|
|
|
|
|
Location of aneurysm: |
|
|
a. ICA P-comm |
|
|
b. carotid terminus |
|
|
c. middle cerebral artery |
|
|
d. basilar bifurcation |
|
|
e. A-comm |
|
|
30. Name the artery(ies) that cross the sylvian fissure. | none cross | G7 p.161:92mm |
 Temporal Craniotomy
Temporal Craniotomy
31. True or False. A temporal craniotomy can allow access to the following structures. |
| G7 p.162:120mm |
a. foramen ovale | true |
|
b. Meckel cave | true |
|
c. labyrinthine and upper tympanic portion of the facial nerve | true |
|
32. A temporal lobectomy |
| G7 p.163:115mm |
a. can safely resect_____cm in the dominant hemisphere | 4 to 5 (before injury to Wernicke area) |
|
b. and_____cm in the nondominant hemisphere. | 6 to 7 (before injury to optic radiations) |
|
 Frontal Craniotomy
Frontal Craniotomy
33. Complete the following regarding the superior sagittal sinus (SSS): |
| G7 p.163:170mm |
a. The risk in sacrifice of the SSS is_____ _____. | venous infarction |
|
b. True or False. It almost always occurs with sacrifice of |
|
|
i. the posterior third | true |
|
ii. the middle third | true |
|
iii. the anterior third | false |
|
 Skull Base Surgery
Skull Base Surgery
34. The Dolenc approach is |
| G6 p.609:95mm |
a. designed to remove the_____ _____ _____ | anterior clinoid extradurally |
|
b. and provide access to the_____ _____ _____ | proximal carotid artery |
|
 Decompressive Craniectomy
Decompressive Craniectomy
35. Indications for decompressive craniectomy are |
| G7 p.165:55mm |
a. |
|
|
i. m_____m_____cerebral artery occlusion | malignant middle |
|
ii. Primarily for the n_____- d_____ hemisphere | non-dominant |
|
b. p_____ i _____hypertension | persistent intracranial |
|
c. True or False. It is necessary to open the dura. | true | G7 p.165:110mm |
d. Skull reimplantation can be considered after_____to_____weeks | 6to12 | G7 p.165:140mm |
e. |
| G7 p.165:147mm |
i. A _____opening is best | large |
|
ii. Approximately_____ by_____cm or larger | 12 by 12 |
|
 Approaches to the Third Ventricle
Approaches to the Third Ventricle
36. Study Chart. |
| G7 p. 168:110mm |
a. t_____ | transcortical |
|
b. t_____ | transcallosal |
|
i. a_____ | anterior |
|
ii. p_____ | posterior |
|
c. s_____ | subfrontal |
|
i. s_____ | subchiasmatic |
|
ii. o_____ | opticocarotid |
|
iii. l_____ t_____ | lamina terminalis |
|
iv. t_____ | transsphenoidal |
|
d. t_____ | transsphenoidal |
|
e. s_____ | subtemporal |
|
f. s_____ | stereotactic |
|
37. What is the risk of postoperative seizures after a transcortical approach to the anterior third ventricle (e.g., for a colloid cyst)? | 5% | |
38. What are the principles of tumor removal |
| G7 p.168:170mm |
a. Veins must be preserved at all_____. | costs |
|
b. First remove the tumor from within the _____ | capsule | G7 p.168:180mm |
c. If adhesions seem unyielding the most likely cause is i_____ i_____ evacuation. | incomplete intracapsular | G7 p.169:15mm |
39. Complete the following: |
| G7 p. 170:180mm |
a. True or False. A disconnection syndrome (split-brain syndrome) is common with |
|
|
i. posterior callosotomy through splenium | true (where more visual information crosses) |
|
ii. anterior callosotomy | false |
|
iii. callosotomy < 2.5 cm in length from a point 1 to 2 cm behind the tip of the genu. | false |
|
b. Which of the above approaches avoids the disconnection syndrome best? | callosotomy < 2.5 cm in length from a point 1 to 2 cm behind the tip of the genu |
|
40. Describe the transcallosal approach to the third ventricle. |
| G7 p.169:170mm |
a. The superior sagittal sinus (SSS) is often to the _____ of the sagittal suture. | right |
|
b. The cranial opening should be |
| G7 p.170:40mm |
i. anterior to the coronal suture | two third |
|
ii. and _____ behind it. | one third |
|
c. The two cingulate gyri may be adherent in the midline and can be mistaken for c_____ c_____. | corpus callosum | G7 p.170:130mm |
d. |
|
|
i. The corpus callosum has a distinct _____ color. | white |
|
ii. It is located beneath the paired _____ arteries. | pericallosal |
|
e. The opening is usually made between the p_____ p_____ arteries. | paired pericallosal | G7 p.170:155mm |
f. The trajectory of dissection is from the |
|
|
i. c _____ s_____ | coronal suture |
|
ii. the e_____ a_____ m_____. | external auditory meatus |
|
iii. The f_____ of M _____ lies along this line. | foramen of Monro |
|
g. |
| G7 p.170:173mm |
i. It is helpful to fenestrate the s _____ P_____ | septum pellicidum |
|
ii. to prevent it from b_____ into the ventricle | bulging |
|
iii. especially in a case of c_____ c_____. | colloid cyst | |
41. How can you tell which ventricle you are in? |
| G7 p.171:38mm |
a. The foramen of Monro is located m_____ | medially |
|
b. If the choroid plexus goes to the left to enter the foramen of Monro you are in the _____ ventricle. | right |
|
c. If you see no choroid plexus and no veins you may be in a c_____ s_____ p _____ | cavum septum pellucidum | G7 p.171:80mm |
d. The safe way to enlarge the foramen of Monro is posteriorly between the _____ _____ and the _____. | choroid plexus; fornix | G7 p.171:115mm |
42. Complete the following about approaches to the third ventricle: |
| G7 p.172:145mm |
a. The interhemispheric approach runs risk of injury to _____ _____ _____ | bilateral cingulate gyrus |
|
b. which may produce _____ _____. | transient mutism |
|
c. The anterior transcallosal approach runs risk of injury to _____ _____ | bilateral fornices |
|
d. which may produce problem with s_____-t_____ m_____ and n_____ l_____. | short-term memory and new learning | G7 p.172:135mm |
e. The transcortical approach is |
| G7 p.172:98mm |
i. made through the_____ _____ gyrus. | middle frontal |
|
ii. This is about the same spot used for e_____v_____d_____. | external ventricular drain |
|
iii. called_____point. | Kocher |
|
43. Localizing levels in spine surgery. Most patients have _____ presacral vertebra. | 24 | G7 p.173:175mm |
44. The aortic bifurcation is at the mid-body of _____. | L3 | G7 p.175:90mm |
 Transoral Approach to Anterior Craniocervical Junction
Transoral Approach to Anterior Craniocervical Junction
45. Complete the following regarding transoral approach to anterior craniocervical junction: |
| G7 p.176:125mm |
a. What percent of patients need posterior fusion after a transoral odontoidectomy? | 75% |
|
b. The patient must be able to open the mouth at least mm. | 25 | G7 p.177:115mm |
c. |
| G7 p.177:140mm |
i. The tubercle of the_____ | atlas |
|
ii. can be palpated through the posterior _____ | pharynx |
|
iii. in order to locate the _____. | midline |
|
d. If C1 sparing is not done the central _____ cm of the _____ is removed. | 3; atlas | |
e. i. There is about to _____ mm working distance | 20 to 25 | G7 p.177:175mm |
ii. between the _____ _____ _____ where | two vertebral arteries |
|
iii. they enter the f_____ t_____ at the inferior aspect of | foramen transversarium |
|
iv. the lateral masses of _____ | C2 |
|
46. Complete the following regarding anterior access: |
| G7 p.178:110mm |
a. To T3 use a s_____ s_____ approach. | sternal splitting |
|
b. At T10 the attachment of the increases the difficulty of this approach. | diaphragm | G7 p.179:45mm |
c. The location of the bifurcation of the vena cava is from just above to just below the _____ disc. | L4-L5 | G7 p.179:90mm |
 Surgical Fusion of the Cervical Spine
Surgical Fusion of the Cervical Spine
47. What are the disadvantages of occipitocervical fusion? | G7 p.179:140mm | |
a. r _____range of motion | reduces (movement at the occipitocervical junction) |
|
b. _____ is higher than_____ | nonunion rate; C1-C2 fusion |
|
48. True or False. The following is an indication for occipitocervical fusion: |
| G7 p.179:150mm |
a. congenital absence of C1 arch | true |
|
b. upward migration of the odontoid into the foramen magnum | true |
|
c. congenital anomalies of occipitocervical joints | true |
|
d. type II odontoid fracture | false |
|
49. Complete the following regarding occipitocervical fusion: |
| G7 p.179:145mm |
a. Patient will lose about _____% of neck flexion. | 30% |
|
b. |
| G7 p.180:80mm |
i. Keel plate must be placed at the | thickest |
|
ii. Region of the_____ occipital bone. | midline |
|
iii. It is advisable to _____ it pre-operatively. | measure |
|
50. True or False. After occipito-cervical fusion we use a halo for |
| G7 p.181:64mm |
a. severe fractures | true |
|
b. elderly patients | true |
|
c. unreliable patients | true |
|
d. smokers | true |
|
e. 8 to 12 weeks | true | |
51. True or False. The C1-C2 complex is responsible for the following percentage of axial rotation: |
| G7 p.181:89mm |
a. 10% | false |
|
b. 15% | false |
|
c. 25% | false |
|
d. 50% | true |
|
e. 75% | false |
|
52. Complete the following regarding anterior odontoid screw fixation: |
| G7 p.181:89mm |
a. C1-C2 complex is responsible for _____ % of head rotation. | 50% |
|
b. Stability depends on the integrity of the |
| G7 p.181:101mm |
i. o_____ p_____and the | odontoid process |
|
ii. a_____ t_____ligament | atlantoaxial transverse |
|
c. Indicated in patients who have a type _____ odontoid fracture and an intact _____ligament | II, transverse | G7 p.181:130mm |
d. Contraindicated if there is a fracture |
| G7 p.181:140mm |
i. of the _____ _____ | vertebral body |
|
ii. and if the fracture is less than _____ months old | 6 | G7 p.181:162mm |
e. |
| G7 p.183:80mm |
i. The immediate postop strength is only _____%. | 50% |
|
ii. Therefore a brace is recommended for weeks. | 6 |
|
iii. If the patient has osteoporosis use a _____. | halo |
|
53. Complete the following regarding anterior odontoid screw fixation: |
| G7 p.181:101mm |
a. The most important structure holding the odontoid in position against the anterior arch of C1 is the_____ ligament. | transverse |
|
b. aka the _____ligament. | atlantoaxial |
|
c. It is the horizontal limb of the_____ ligament. | cruciate |
|
54. True or False. The following condition is an indication for anterior odontoid screw fixation: |
| G7 p.181:130mm |
a. pathologic odontoid fracture | false |
|
b. type III odontoid fracture where the fracture line is in the caudal portion of body of C2 | false |
|
c. type I odontoid fracture that is reducible | false |
|
d. type II irreducible odontoid fracture | false |
|
e. type II reducible odontoid fracture | true |
|
f. age of fracture is less than 6 months | true | |
55. What are indications for odontoid screw? |
| G7 p.181:131mm |
a. Fracture must be_____ | reducible |
|
b. Type_____ fracture | II |
|
c. Which ligament must be intact? | transverse |
|
56. True or False. The following are contraindications for anterior odontoid screw fixation: |
| G7 p.181:140mm |
a. disruption of atlantal transverse ligament | true |
|
b. disruption of apical ligament | false |
|
c. fracture of C2 vertebral body | true |
|
d. reducible odontoid type II fracture | false |
|
57. Indications for odontoid screw fixation include |
| G7 p.181:160mm |
a. type of fracture:_____ | II odontoid |
|
b. age of fracture: less than_____ _____ old | 6 months |
|
c. ligament: t_____ l_____ i_____ | transverse ligament intact |
|
d. judged by: |
|
|
i. _____ and | MRI |
|
ii. _____ of _____ | rule of Spence |
|
e. |
|
|
i. The immediate postop strength is only _____% | 50% | G7 p.183:80mm |
ii. Therefore a brace is recommended for _____ weeks | 6 |
|
iii. If the patient has osteoporosis, use a halo _____ |
| |
58. Provide fusion rates with age of fracture. |
| G7 p.181:162mm |
a. Fusion rates in fractures more than 18 months old: _____% | 25% |
|
b. Fusion rates in fractures less than 6 months old: _____% | 90% |
|
 Atlantoaxial Fusion (C1-C2 Arthrodesis)
Atlantoaxial Fusion (C1-C2 Arthrodesis)
59. Characterize atlantoaxial fusion (C1-C2 arthrodesis). |
| G7 p.183:125mm |
a. The patient will lose about _____%of head rotation | 50% |
|
b. Transarticular screws |
| G7 p.184:150mm |
i. Danger is to the v_____ a_____ | vertebral artery |
|
ii. Provides i_____ s_____ | immediate stabilization |
|
iii. Requires preop _____ to study vertebral arteries | CT | |
60. True or False. The following is an indication for atlantoaxial fusion: |
| G7 p.183:140mm |
a. type I odontoid fracture | false |
|
b. disruption of alar ligament of dens | false |
|
c. disruption of apical ligament of dens | false |
|
d. vertebrobasilar insufficiency with head turning | true (Disruption of alar or apical ligament of dens does not render the spine unstable as long as the transverse ligament is intact.) |
|
61. Characterize bow hunter’s sign. |
| G7 p.183:82mm |
a. What is bow hunter’s sign? | vertebrobasilar insufficiency with head turning |
|
b. What is the treatment for bow hunter’s sign? | atlantoaxial fusion (C1-C2 arthrodesis) |
|
62. Characterize a C1-C2 fusion. |
| G7 p.183:125mm |
a. What mobility is lost? |
| Also |
i. head rotation _____% | 50% | G6p.623:170mm |
ii. lateral mobility_____ % | 35% |
|
b. Which technique produces less loss of mobility? |
|
|
i. Brooks | All are the same in regard to loss of mobility. |
|
ii. Gallie | All are the same in regard to loss of mobility. |
|
iii. Sonntag | All are the same in regard to loss of mobility. |
|
63. Describe the fusion technique and differentiate. |
| G7 p.184:75mm Also |
a. Brooks fusion |
| G6p.624:120mm |
i. sublaminar to_____ | C1 and C2 sublaminar wiring |
|
ii. with _____ grafts | two-wedge bone |
|
b. Gallie fusion |
|
|
i. sublaminar to_____ | C1 only |
|
ii. with _____ graft | “H” graft wired into place to C1 only |
|
c. Sonntag fusion |
|
|
i. sublaminar to | C1 only |
|
ii. with _____ graft | bicortical graft wedged between C1 and C2 |
|
64. Characterize C1-C2 transarticular facet screw |
| G7 p.184:175mm |
a. Special preop test needed is a thin cut CT scan from the |
|
|
i. _____ _____ | occipital condyles |
|
ii. through to C_____ | C3 |
|
iii. to look for the location of the _____ _____. | vertebral arteries |
|
b. A fusion rate of up to _____% has been reported. | 99% | |
65. With postoperative immobilization: |
| G6 p.625:25mm |
a. The use of what apparatus is considered optimal immobilization of the cervical spine? | halo brace |
|
b. It reduces cervical motion by_____ %. | 95% |
|
c. It is mandatory for use in |
|
|
i. r_____ _____ | rheumatoid arthritis |
|
ii. o_____ | osteopenia |
|
d. The next best apparatus is the_____- _____ -_____ _____ _____. | sternal-occipital-mandibular immobilizer (SOMI) brace |
|
e. Use this apparatus for_____weeks. | 12to16 |
|
f. Follow with a_____ for_____ weeks. | hard collar for 4 to 6 |
|
g. Use _____-_____ _____ to determine if this treatment was satisfactory. | flexion-extension films |
|
66. Give the frequency of osseous fusions for the listed techniques. |
| G6 p.625:60mm |
a. Brooks _____% | 70 to 85% |
|
b. Gallie _____% | 70 to 85% |
|
c. Sonntag_____ % | 97% |
|
67. True or False. The following is associated with nonunion in atlantoaxial fusion: |
| G6 p.625:80mm |
a. rheumatoid arthritis | true |
|
b. cigarette smoking | true |
|
c. osteoporosis | true |
|
d. nonsteroidal antiinflammatory drugs (NSAIDs) |
| true |
68. What are modifying correctible risk factors for a C1-C2 arthrodesis? |
| G6p.625:100mm |
a. c_____ s_____ | cigarette smoking |
|
b. m _____-o_____ | malnutrition-osteoporosis |
|
c. N_____ | stopping suppressive drugs (NSAID) 1 week before and 2 weeks after surgery |
|
d. s_____ | steroids |
|
e. i_____ | immunosuppressives |
|
f. a _____b_____ | use autologous bone |
|
69. Complete the following: |
| G6p.625:105mm |
a. How does smoking produce nonunion of fusions? | interferes with vascularization of healing bone grafts |
|
b. What is the responsible chemical? | nicotine |
|
c. Will it help if patients stop smoking by using nicotine patches? | no |
|
70. Complete the following concerning an anterior odontoid screw: |
| G7 p.183:85mm |
a. After placement what postop treatment is recommended? | immobilization in cervical brace |
|
b. How long? | 6 weeks |
|
c. If patient has osteoporosis, use_____ | halo | |
71. Complete the following concerning a C1-C2 transarticular facet screw: |
| G7 p.184:140mm |
a. Indication—used in conjunction with _____ _____ | Sonntag fusion |
|
b. Benefit |
|
|
i. provides immediate_____ | stabilization |
|
ii. avoids postoperative_____ | external orthosis |
|
iii. A major risk of the procedure is _____ _____ _____. | vertebral artery injury |
|
72. Characterize atlantoaxial-axial fusion (C1-C2arthrodesis). |
| G7 p.183:125mm |
a. The patient will lose about _____% of head rotation. | 50% |
|
b. Transarticular screws |
| G7 p.184:150mm |
i. Danger is to the v_____ a_____ | vertebral artery |
|
ii. Provides i_____ s_____ | immediate stabilization |
|
iii. Requires preop _____ to study vertebral arteries | CT | G7 p.184:175mm |
73. Complete the following regarding surgical fusion of lumbar and lumbosacral spine: |
| G7 p.191:103mm |
a. True or False. A lumbar fusion that includes L1 |
|
|
i. Should not be terminated at L1 | true |
|
ii. Should not be terminated at T12 | true |
|
b. Pedicle screws |
| G7 p.191:145mm |
i. Should be _____ to _____ % of pedicle | 70 to 80% |
|
ii. Should be greater than mm in the adult | 5.5 |
|
iii. The length should be _____ to _____ % of the vertebral body | 70 to 80% |
|
iv. typically_____ to _____mm long | 40 to 50 |
|
c. Medial angles for lumbar pedicle screws |
| G7 p.192:15mm |
i. L1 level—medial angle should be _____ degrees | 5 |
|
ii. L2 level—medial angle should be _____degrees | 10 |
|
iii. L3 level—medial angle should be _____degrees | 15 |
|
iv. L4 level—medial angle should be _____degrees | 20 |
|
v. L5 level—medial angle should be _____degrees | 25 |
|
vi. S1 level—medial angle should be _____degrees | 25 |
|
vii. S2 level—medial angle should be _____degrees | 45 | |
d. On AP view if screw tip |
|
|
i. Crosses the midline there is a _____ breech | medial |
|
ii. Does not pass medial to the medial edge of the pedicle there is likely a _____ breech | lateral |
|
e. Posterior lumbar interbody fusion (Plif and Tlif) |
| G7 p.193:15mm |
i. Not appropriate if _____height is preserved | disc |
|
ii. Usually supplemented with_____ _____ | pedicle screws |
|
f. Anterior lumbar interbody fusion |
| G7 p.195:18mm |
i. has a risk of_____ _____ | retrograde ejaculation |
|
ii. of from _____ to _____% | 2 to 45% |
|
74. True or False or Unreliable. In assessing lumbar fusion the following tests can suggest success: |
| G7 p.198:40mm |
a. static x-rays | false |
|
b. flexion—extension views | true |
|
c. technetium 99 bone scan | false |
|
d. good clinical outcome | unreliable |
|
e. CT scan | true |
|
75. Components necessary for bone graft fusion are |
| G7 p.198:100mm |
Hint: IGC |
|
|
a. Osteoinduction is _____ of mesenchymal cells. | recruitment |
|
b. Osteogenesis is the process of forming _____ _____. | new bone |
|
c. Osteoconduction structure adds _____ _____ and acts as a _____. | new vessels, scaffold |
|
| Hint: |
|
| Induces mesenchymal cells to |
|
| transform |
|
| Generates bone cells |
|
| Constructs bone scaffold |
|
76. Allograft provides only osteo- _____. | conduction | G7 p.199:92mm |
77. DBM |
| G7 p.199:92mm |
a. aka as d_____ bone m_____ | demineralized; matrix |
|
b. has _____ and _____ properties | inductive and conductive |
|
78. BMP |
| G7 p.199:145mm |
a. aka bone m_____ p_____ | morphogenic protein |
|
b. has _____ properties | inductive |
|
c. may cause e_____ b_____ | ectopic bone |
|
d. approved by FDA only for_____ | Alif | |
79. Complete the following regarding graft procurement: |
| G7 p.200:73mm |
a. Anterior iliac bone graft |
|
|
i. Obtain _____to _____cm | 3to4 |
|
ii. _____to the anterior superior iliac crest | lateral |
|
iii. To avoid the l_____ f_____ c_____ nerve | lateral femoral cutaneous |
|
iv. Also need to avoid injury to the i_____ and i_____ | ilioinguinal and iliohypogastric |
|
b. Posterior iliac crest bone graft |
| G7 p.200:103mm |
i. Obtain from the_____ | medial |
|
ii. _____to _____cm of the iliac crest | 6 to 8 |
|
iii. To avoid the s_____ c_____ nerves | superior cluneal |
|
iv. If injured, they cause b_____ n_____ or p_____ n_____ | buttock numbness or painful neuromas |
|
c. The “dimple of Venus” lies directly |
| G7 p.200:133mm |
i. above the s_____ joint. | sacro iliac |
|
ii. Incise a little _____to it. | lateral |
|
iii. Avoid mistaking the s_____ | sacrum |
|
iv. and the i_____ s_____ | iliac spine |
|
 Lumbar Punctures
Lumbar Punctures
80. Complete the following regarding lumbar punctures: |
| G7 p.201:175mm |
a. For lumbar puncture (LP) the platelet count should be higher than_____. | 50,000/mm3 |
|
b. In SAH, LP might increase the_____ pressure and precipitate aneurismal rupture. | transmural | G7 p.202:15mm |
c. An LP in patients with spinal block may produce deterioration in as many as _____%. | 14% | G7 p.202:25mm |
81. The spinal cord ends at the given location for what percentage of adults? |
| G7 p.202:45mm |
a. between T12 and L1 | 30% |
|
b. between L1 and L2 middle thirds | 51 to 68% |
|
c. between L2 and L3 | 10% |
|
d. between T12 and L2 | 94% |
|
82. The intercristal line |
| G7 p.202:60mm |
a. connects the superior border of the_____ _____ | iliac crests |
|
b. occurs in most adults between the spinous processes of _____ and _____ | L4 and L5 | |
83. Complete the following statements: |
| G7 p.202:95mm |
a. When an LP is performed, we must always advance the needle with _____ _____ in place. | the stylet |
|
b. Otherwise we may introduce_____ _____, | epidermal cells |
|
c. which could produce an iatrogenic _____ _____. | epidermoid tumor |
|
84. Describe the Queckenstedt test and expected results. |
| G7 p.202:180mm |
a. What do you compress? | the jugular vein |
|
b. One or both? | one then the other, while measuring ICP |
|
c. If no block what will happen with compression? | pressure should rise 10 to 20 cm from baseline |
|
d. If no block what happens upon release of compression | return to the original level within 10 seconds |
|
e. If there is a block what will happen? | no rise in pressure from baseline |
|
85. Complete the following about lumbar punctures: |
| G7 p.203:85mm |
a. Incidence of severe postpuncture headache is _____%. | 0.1 to 0.5% |
|
b. Severe means_____. | lasting longer than 7 days |
|
86. Complete the following about lumbar punctures: |
| G7 p.203:155mm |
a. Can a sixth nerve (abducens nerve) palsy occur after lumbar puncture? | yes |
|
b. If so when? | after 5 to 14 days |
|
c. If it occurs when does it resolve? | 4 to 6 weeks |
|
87. True or False. Regarding fundus exam for papilledema: |
| G7 p.204:25mm |
a. It is a reliable test to assure safety of LP. | false |
|
b. It is an unreliable test. | true |
|
c. It takes 6 to 24 hours for papilledema to occur. | true |
|
d. A better test of safety would be a C_____s_____. | CT scan |
|
88. True or False. If you suspect meningitis but cannot promptly get a CT scan |
| G7 p.204:85mm |
a. you may do an LP without a CT scan | true (very small risk) |
|
b. even if there is papilledema | true (risk is still low) |
|
c. and if there are unequal pupils and/or hemiparesis | false (suggests an hemiparesis asymmetrical mass; do not do LP) |
|
89. You suspect meningitis but cannot promptly get a CT scan. If the patient deteriorates during LP the anecdotal recommendation is to immediately ________ ________ ________. | replace the fluid | |
90. True or False. The following may reduce the frequency of post-LP headache: |
| G7 p.204:135mm |
a. Use a small-size needle. | true |
|
b. Orient the bevel longitudinally. | true |
|
c. Position the patient flat in bed. | false (not shown to be truly beneficial) |
|
d. Remove only a little fluid. | false (not shown to be truly beneficial) |
|
e. Replace the stylet before removing the needle. | true |
|
f. Hydrate the patient after the LP. | false (not shown to be truly beneficial) |
|
 C1-C2 Punctures
C1-C2 Punctures
91. What condition makes lateral cervical puncture contraindicated? | Chiari malformation | G7 p.205:125mm |
 Ventricular Catheterization
Ventricular Catheterization
92. True or False. Sites that may be used for ventricular catheterization are |
| G7 p.207:80mm |
a. Keen point | true |
|
b. Dandy point | true (but may injure visual pathways) |
|
c. occipital-parietal region | true |
|
d. Kocher point | true |
|
93. Keen point |
| G7 p207:168mm |
a. is about_____ cm superior to the PINNA | 3 |
|
b. is about _____ cm posterior to the PINNA | 3 |
|
c. places catheter into the_____ | trigone |
|
 Ventriculostomy/ICP Monitors
Ventriculostomy/ICP Monitors
94. True or False. The site most commonly used for ICP monitoring is |
| G7 p.207:180mm |
a. occipitoparietal region | false |
|
b. Frazier burr hole | false |
|
c. Keen point | false |
|
d. Dandy point | false |
|
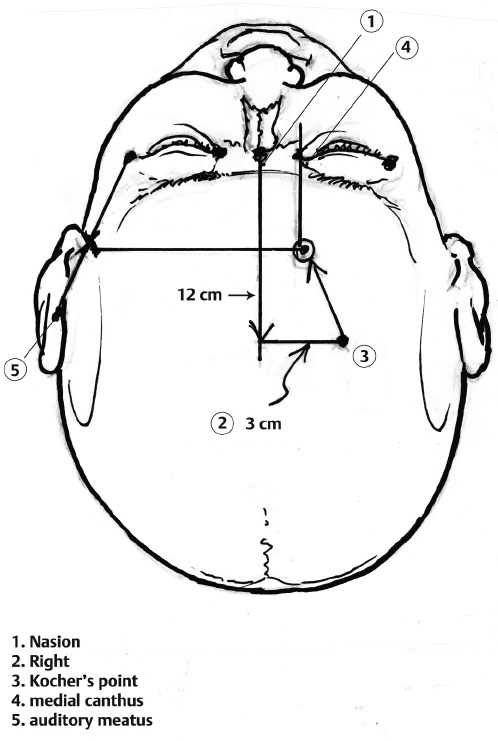
e. Kocher point | true (2 to 3 cm from midline, approximate midpupil line; 1 cm anterior to coronal suture; aim toward ipsilateral inner-canthus and external auditory canal) | |
95. Another technique: Hint: Easy as 1-2-3 |
| G7 p.208:72mm |
| ||
Fig. 7.1 |
|
|
|
| Illustration by Tony Pazos |
a. Measure 12 cm up the midline from the_____. | nasion |
|
b. Measure 3 cm to the_____. | right |
|
c. This is the approximate site of _____ point. | Kocher |
|
d. Drill opening, puncture dura, aim catheter medially toward ipsilateral _____ _____ | medial canthus |
|
e. on a plane halfway between the contralateral lateral canthus and external _____ _____. | auditory meatus | (Thanks to Dr. Thomas Stilp, Chicago) |
 Ventricular Shunts
Ventricular Shunts
96. List the layers to traverse in the placement of peritoneal catheter. Hint: samp3 |
| G7 p.210:20mm |
a. s_____ _____ | subcutaneous fat |
|
b. a_____ _____ | anterior sheath |
|
c. m_____ | muscle |
|
d. p_____ _____ | posterior sheath |
|
e. p_____ _____ | preperitoneal fat |
|
f. p_____ | peritoneum |
|
97. Ventriculoatrial shunt should be revised when the catheter tip is above _____. | T4 | G7 p.211:110mm |
98. The needle to use in ommaya reservoir is a b_____ _____ or smaller gauge. | butterfly 25 | G7 p.21 2:160mm |
99. During third ventriculostomy |
| G7 p.213:70mm |
a. The opening is made |
|
|
i. _____ to the mammillary bodies. | anterior |
|
ii. This site is _____ to the basilar artery. | anterior |
|
b. After puncturing the floor be certain that the m_____ of L_____ is also perforated. | membrane of Liliequist | G7 p.213:100mm |
 Sural Nerve Biopsy
Sural Nerve Biopsy
100. Nerve biopsy has a role in diagnosing the following: Hint: aCdHmv |
| G7 p.214:125mm |
a. a_____ | amyloidosis |
|
b. C_____-M_____-T_____ | Charcot-Marie-Tooth |
|
c. d_____a_____ | diabetic amyotrophy |
|
d. H_____d_____ | Hansen disease |
|
e. m_____l_____ | metachromatic leukodystrophy |
|
f. v_____ | vasculitis |
|
101. Sural nerve biopsy |
| G7 p.214:153mm |
a. At the level of the ankle the sural nerve |
|
|
i. lies between the_____tendon | Achilles |
|
ii. and the_____malleolus. | lateral |
|
b. A tourniquet distends the_____ _____ vein. | lesser saphenous |
|
c. To biopsy only a portion of the fascicles open the_____and tease out a few fascicles. | epineurium |
|
d. |
| G7 p.215:115mm |
i. Sensory loss is_____ | expected |
|
ii. but may not last more than a_____ _____. | a. few weeks |
|
 Nerve Blocks
Nerve Blocks
102. True or False. The following are risks of bilateral stellate ganglion block: |
| G7 p.215:170mm |
a. glossopharyngeal nerve injury bilaterally | false |
|
b. respiratory compromise | true |
|
c. hypoglossal nerve injury bilaterally | false |
|
d. bilateral laryngeal nerve injury | true (Glossopharyngeal and hypoglossal nerves are higher in the cervical region.) |
|
103. The palpable landmark at C6 is called |
| G7 p.216:23mm |
a. C_____ t_____ | Chassaignac’s tubercle |
|
b. also known as a_____ t_____ of t_____ p_____ of C_____ | anterior tubercle; transverse process of C6 |
|
c. also known as_____ _____ | carotid tubercle |
|
104. True or False. The following are signs of a successful stellate ganglion block: |
| G7 p.216:40mm |
a. unilateral vocal cord paralysis | false |
|
b. hoarseness | false |
|
c. unilateral Horner syndrome | true |
|
d. upper extremity weakness from brachial plexus effect | false |
|
e. increased warmth of ipsilateral hand | true |
|
f. anhidrosis of the ipsilateral hand | true |
|
105. Complete the following concerning the intercostal nerve block: |
| G7 p.216:115mm |
a. A good site for injection is the p_____a_____l_____. | posterior axillary line |
|
b. How many nerves need to be blocked to produce some anesthesia? | three |
|
c. Why so many? | overlap |
|
d. Order of structures from top down is _____ _____ _____ _____.(Hint: rvan) | rib, vein, artery, nerve |
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 indigo carmine;
indigo carmine;  methylene blue;
methylene blue;  fluorescein
fluorescein



 Thrombostat;
Thrombostat;  Gelfoam;
Gelfoam;  Oxycel;
Oxycel;  Surgicel;
Surgicel;  Avitene
Avitene




 5-6-4,
5-6-4,  5-5-5,
5-5-5,  5-4-6 Objective: approach for
5-4-6 Objective: approach for




 angled 30 degrees,
angled 30 degrees,  angled 45 degrees,
angled 45 degrees,  angled 60 degrees
angled 60 degrees