18Ophthalmology
D At the junction of the left optic nerve and chiasm
A lesion at the junction of the left optic nerve and chiasm could affect the Wilbrand knee, which is a group of fibers supplying vision to the superior temporal field in the contralateral eye. In this case, the patient would have a central scotoma in the left eye due to the optic nerve involvement and a right superior temporal visual defect in the right eye. (A) A lesion in the left inferior optic radiations would produce a relatively congruous right superior quadrantanopsia. (B) A lesion in the right occipital pole would produce a left central homonymous hemifield deficit. (C) A lesion in the orbital portion of the left optic nerve would produce a central scotoma in the left eye. (E) A lesion in the optic chiasm would produce variable visual field deficits, and classically is described as producing a central bitemporal hemianopsia if only the decussating nasal-macular fibers are affected.
E Ability to turn head
In oculomotor apraxia, patients have difficulty with saccade initiation in addition to a blunted or absent vestibulo-ocular reflex. Patients must turn (and typically thrust) their heads to track objects and often overshoot the target. (A) The optokinetic reflex involves smooth pursuits of the eyes followed by saccadic movement. When an object moves by, the eyes track the object until it has left the visual field and then return to the initial position through a saccade. Think about being able to fixate on telephone poles while driving by them rapidly. (B) The ability to converge on an object has no role in assisting this patient. (C) In oculomotor apraxia, patients have a blunted or absent vestibulo-ocular reflex, which is the reflex enabling the eyes to maintain fixation on an object as the head makes slight turns and movements. (D) The tonic labyrinthine reflex is a primitive reflex that disappears by 6 months of age. It involves full-body extension except for flexion of the upper extremities when the head is extended in the supine position. It would not assist this patient.
D Sympathetic chain distal to the superior cervical ganglion but proximal to the off-take of the vasomotor fibers
A lesion of the sympathetic chain distal to the superior cervical ganglion proximal to the off-take of the vasomotor fibers results in a third-order Horner syndrome with anhydrosis of only the brow. The vasomotor fibers to the rest of the face emerge from the sympathetic chain proximal to the superior cervical ganglion at the level of the carotid bifurcation. Amphetamines would not cause pupillary dilation, as amphetamines cause a release of norepinephrine only in an intact neuron. (A, B) Lesions proximal to the synapse of central sympathetic fibers in the upper thoracic spinal cord result in a first-order Horner syndrome with miosis, ptosis, and anhydrosis of the ipsilateral face, arm, and trunk. Amphetamines would cause pupillary dilation, as the third-order neuron is intact. (C) A lesion of the proximal sympathetic chain results in a second-order Horner syndrome and in anhydrosis of the face as the vasomotor fibers decussate at the carotid bifurcation and follow the external carotid artery. The fibers innervating the arm and truck already have emerged from the sympathetic chain. Amphetamines would cause pupillary dilation, as the third-order neuron is intact. (E) A lesion of the sympathetic chain distal to the superior cervical ganglion distal to the offtake of the vasomotor fibers results in a third-order Horner syndrome without anhydrosis. Amphetamines would not cause pupillary dilation, as amphetamines cause a release of norepinephrine only in an intact neuron.
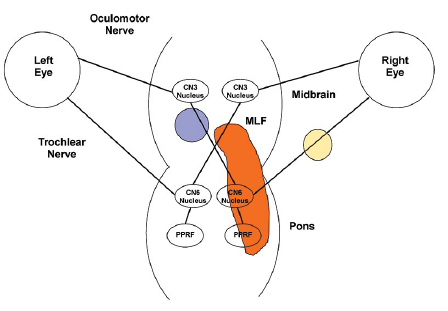
C Ipsilateral paramedian pontine reticular formation and the ipsilateral medial longitudinal fasciculus
B Painless, slowly progressive monocular vision loss
The typical diagnostic triad of optic nerve sheath meningiomas (ONSMs) is painless, slowly progressive vision loss with optic atrophy and optociliary shunt vessels. (A) ONSMs arise from the proliferation of meningoepithelial cells lining the intraorbital or intracanalicular optic nerve. They arise from the arachnoid and not the dural layer. (C) Optic atrophy is seen. (D) ONSMs account for one third of optic nerve tumors and are the second most common cause after benign optic nerve gliomas. They usually affect women in their 40s or 50s.
C Horner syndrome
In nuclear-fascicular syndrome with injury to the trochlear nucleus and fasciculus (the two almost always are injured together due to the short course of the midbrain trochlear fascicles), there may be injury to the descending sympathetic pathways through the dorsolateral tegmentum. This could manifest in a Horner syndrome contralateral to the observed trochlear nerve deficit. (A) The pupil would be miotic and not mydriatic with a Horner syndrome. (B) Although the extent of the infarction may extend into the pons and affect the abducens nucleus, it will affect other anatomy first. (D) Although the oculomotor nucleus is located in the midbrain, it is more likely that the patient would suffer other deficits prior to oculomotor involvement.
D Between the third and fourth neurons
The light-near dissociation disorder described is Adie syndrome, as the other two primary causes were ruled out. Adie syndrome results from a viral or bacterial infection of the ciliary ganglion. This is the synapse of the third and fourth neurons in the pupillary reflex pathway. (B) The first neurons in the pupillary reflex pathway originate in the retinal ganglion cells in the eye and project to the pretectal nucleus through the optic nerve. (C) The second neurons in the pupillary reflex pathway originate in the pretectal nucleus and synapse in the Edinger-Westphal nucleus of the rostral midbrain. The third neurons then emerge and run along the oculomotor nerves. (E) The fourth neurons in the pupillary reflex pathway run from the ciliary ganglion through the short ciliary nerves to innervate the iris sphincter muscle.
B A right olfactory groove meningioma
The patient has signs and symptoms consistent with Foster-Kennedy syndrome. The syndrome is defined as optic atrophy and a central scotoma (loss of vision in the middle of the visual field) in the ipsilateral eye, disk edema in the contralateral eye, and ipsilateral anosmia. These symptoms typically are caused by an olfactory groove lesion.
A Hunt-Hess score
More severe aneurysmal subarachnoid hemorrhage as identified by a greater Hunt-Hess score is the major predictor of the incidence of Terson syndrome. The syndrome is defined as intraocular hemorrhage associated with intracranial hemorrhage and elevated intracranial pressure and occurs in 10 to 50% of cases of aneurysmal subarachnoid hemorrhage. Visual acuity may or may not be affected. (D) There is no definite association with the occurrence of Terson syndrome and the location of a ruptured aneurysm.
A Myasthenia gravis
The relaxation of the orbicularis oculi after prolonged contraction fits well with the symptom manifestation of myasthenia gravis, in which muscles fatigue with sustained use. Symptoms tend to be worse with drowsiness and can be improved after a short period of ice application to the muscle. (B) Hemifacial spasm would manifest in a tonic or clonic contraction of the orbicularis oculi. It can be treated with botulinum toxin injections. (C) The orbicularis oculi demonstrates good strength at the start of the examination and thus is not paretic. (D) Disinsertion of the levator palpebrae would cause a ptosis. (E) Botulinum toxin injection into the orbicularis oculi would cause a sustained paresis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree