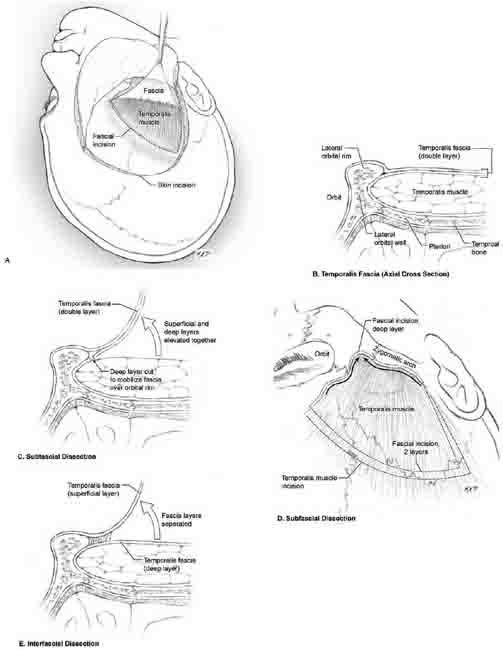
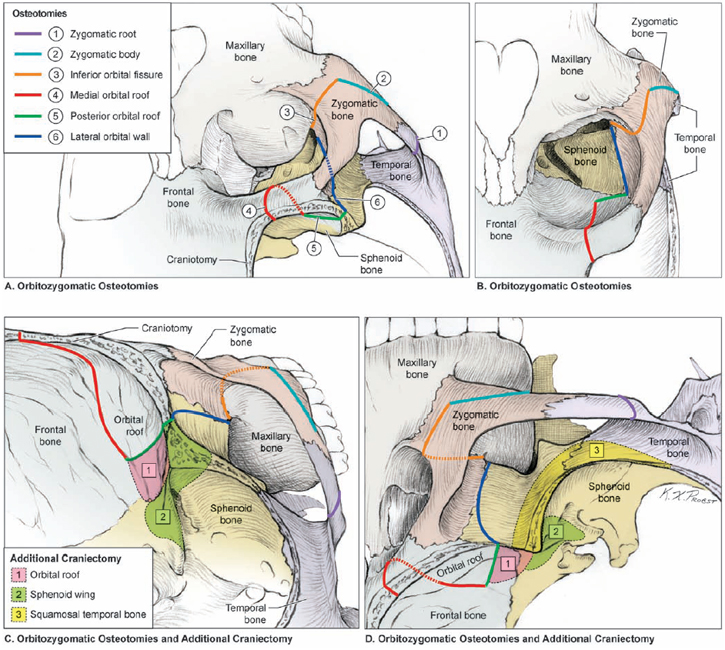
11 Orbitozygomatic Approach The orbitozygomatic approach dramatically enhances the standard pterional craniotomy. When a patient’s head is rotated away from the aneurysm and extended, the superior and lateral orbit becomes the roof of the operative corridor. Drilling down the pterion raises this roof, but not nearly as much as removing orbital walls completely and depressing the eye with the dural flap. Zygoma resection increases the mobilization of the temporalis muscle inferiorly, which opens the middle fossa to facilitate mobilization of the temporal lobe in a posterolateral direction. A widened operative corridor improves illumination, reduces brain retraction, and improves maneuverability. A good orbitozygomatic approach gives the neurosurgeon a wide sweep of surgical trajectories ranging from supraorbital to transsylvian to pretemporal to subtemporal. Surgical trajectory can then be tailored to the pathology. In addition, the orbitozygomatic approach extends the upward view of the basilar apex. The line of sight through the microscope intersects with the orbital rim and eye as the viewing target rises in the interpeduncular cistern. The orbitozygomatic approach eliminates the shadow that would otherwise be cast over high-riding basilar apex aneurysms with a pterional approach. The orbitozygomatic approach is routinely used for basilar apex aneurysms. It is used selectively in the anterior circulation, primarily with giant and complex aneurysms. Deep bypass procedures benefit from the additional working room of this approach. Enhanced exposure is always advantageous, but it can cause subtle orbital asymmetries that bother some patients. There are other risks, including frontalis nerve injury, pulsatile enophthalmos, orbital entrapment, diplopia from extraocular muscle or nerve injury, blindness, and communication with frontal or ethmoidal sinuses with potential routes of infection or cerebrospinal fluid (CSF) leakage. The incidence of these complications is low. Patient position and skin incision are the same with the orbitozygomatic approach as with the pterional approach. The first difference is the soft tissue dissection to expose the orbitozygomatic unit. The zygoma and orbital rim are ensheathed in two layers of temporalis fascia (Fig. 11.1A), and elevating the superficial layer exposes bone (Fig. 11.1B). Sub-fascial dissection elevates both fascial layers off the temporalis muscle, and then cuts the deep layer along the posterior edge of the lateral orbital rim and the superior edge of the zygoma, allowing it to mobilize with the superficial layer over the orbitozygomatic unit (Fig. 11.1C,D). Interfascial dissection separates these two layers, leaves the deep layer on the temporalis muscle, and mobilizes just the superficial layer over the lateral orbital rim and zygoma (Fig. 11.1E). The subfascial dissection is simple, fast, and preferred. Fig. 11.1 (A) Dissection of the temporalis fascia. The temporalis fascia is incised from the zygomatic arch to the superior temporal line along the skin incision, then anteriorly to the keyhole. The facial flap elevates easily when the muscle is not incised and is left attached to the skull. (B) Anatomy of the temporalis fascia. The zygoma and orbital rim are ensheathed by the fascial layers. The superficial temporalis fascia covers the zygoma and orbital rim, extending inside the orbit where it transitions to the periorbita. Deep temporal fascia envelopes the temporalis muscle in the temporalis fossa, remaining outside the orbit. These fascial layers are separated to expose the orbital walls and zygoma for osteotomies. (C) Subfascial dissection technique leaves the superficial and deep temporalis fascia together over the muscle, but cuts the deep fascia along the posterior edge of the lateral orbital rim and superior edge of zygoma. These cuts release the superficial fascia, allowing it to elevate over the orbital rim and zygoma. (D) The deep layer of the temporalis fascia is incised by following the superior edge of the zygoma to the maxilla (right arrow) with a sharp round knife or dissector. Similarly, the contours of the posterior edge of the lateral orbital rim are followed to the maxilla (left arrow) with a sharp round knife or dissector, joining the other fascial incision. (E) The interfascial dissection technique separates the superficial and the deep fascia over the muscle. The superficial fascia peels over the orbital rim and zygoma, and deep fascia remains around the temporalis muscle. The subfascial dissection is simple, faster, and preferred. Both layers of fascia are incised from the zygomatic arch to the superior temporal line along the skin incision, then anteriorly to the keyhole, running 1 cm below the superior temporal line (Fig. 11.1A). Temporalis muscle is not incised because the fascial flap elevates easily when underlying muscle remains attached to the skull. A round-tipped dissector with a sharp edge advanced along the superior edge of the zygoma to the maxilla, and along the posterior edge of the lateral orbital rim to the maxilla, cuts the deep fascial layer and releases the fascial flap. A deep fat pad lies beneath this fascial flap, with an outer layer that mobilizes with the fascial flap and an inner layer that travels under the zygoma with the temporalis muscle. These fat pads are separated with blunt dissection strokes from the zygoma superiorly into this plane. The orbitozygomatic unit consists of the orbital rim, orbital roof, lateral orbital wall, and zygomatic arch. This orbitozygomatic unit is removed in several ways: with the cranial flap as one integrated piece; separate from the cranial flap as two pieces; and separate from the cranial flap as two pieces, with a modified orbital unit that does not include the zygoma. The two-piece approach with the complete orbitozygomatic unit is the standard technique used most often. The one-piece orbitozygomatic approach gives a better cosmetic result but the osteotomies are more difficult to perform. The modified orbital approach is used when the zygoma resection would not add meaningfully to the exposure. The frontotemporal craniotomy resembles that of the pterional approach, but the anteromedial corner extends more medially beyond the supraorbital notch. Dura of the frontal lobe is elevated 3 cm posteriorly to visualize the orbital roof. The pterion does not need to be drilled because it is removed with the orbit. Before making any osteotomies, the inferior frontal dura and periorbita are protected from the saw blade with strips of Telfa. The orbitozygomatic unit is released by a series of six osteotomies (Fig. 11.2) made with a reciprocating saw, which minimizes bone loss from the cuts. The first cut is made across the root of the zygomatic process of the temporal bone (zygomatic root), angling the saw blade away from the temporomandibular joint that lies on the inferomedial surface of zygomatic root (Fig. 11.2, osteotomy 1). This cut in the root is made with two perpendicular cuts, creating a notch that seats the zygoma more securely than would one straight cut. A fixation plate is placed in the zygoma and registered with a drill hole in the root to improve the cosmesis of the repair. The second and third cuts are made across the temporal process of the zygomatic bone (malar eminence), first from the inferolateral margin of the zygomatic arch continuing halfway across the zygomatic bone (Fig. 11.2, osteotomy 2), and then from the inferior orbital fissure through the zygomatic bone to the same endpoint (Fig. 11.2, osteotomy 3). The inferior orbital fissure is difficult to visualize directly but can be palpated with a thin dissector, which also guides the tip of the saw blade into the fissure and protects the eye. When these two osteotomies connect, the resulting V in the zygomatic bone secures the fragment into position when replaced. The fourth cut is along the medial orbital roof in an anterior-posterior direction, just lateral to the supraorbital notch (Fig. 11.2, osteotomy 4). The frontal dura is protected with Telfa strips and gentle retraction, and the saw is angled as the cut deepens to keep the teeth at the heel of the blade from contacting dura. The eye is also protected with Telfa strips and gentle retraction. The fifth cut crosses the posterior orbital roof in a medial-to-lateral direction, approximately 2 to 3 cm posterior to the inner table of the frontal bone (to preserve the orbital roof), and finishes laterally in the thick bone of the sphenoid ridge and pterion (Fig. 11.2, osteotomy 5). The sixth cut crosses the lateral orbital wall, beginning in the inferior orbital fissure from outside the orbit and connecting in the sphenoid ridge and pterion with the previous cut (Fig. 11.2, osteotomy 6). The orbitozygomatic unit can then be removed as a single piece.
 Rationale and Indications
Rationale and Indications
 Extracranial Dissection
Extracranial Dissection
 Craniotomy and Osteotomies
Craniotomy and Osteotomies
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree