1 | Ossification of the Posterior Longitudinal Ligament: Anterior Cervical Approach |
 | Case Presentation |
History and Physical Examination
A 48-year-old woman presented to the office with chief complaints of neck pain, bilateral arm and leg numbness and weakness, and a feeling of “stiffness” in her extremities. She had increased difficulty with ambulation and repetitive use of her hands. These symptoms started approximately 5 weeks prior to her presentation and had rapidly progressed over the past 3 weeks. These symptoms were significantly inhibiting activities of daily living. She denied any changes in her bowel or bladder function. There was no history of inciting trauma. Her medical history was significant only for obesity.
Her physical examination was markedly positive for signs of cervical myelopathy. She was unable to ambulate unassisted in a straight line and had great difficulty performing repetitive hand motion. She had positive Hoffmann and Babinski signs as well as generalized hyper-reflexia bilaterally. She had sustained ankle clonus on the left and seven beats of ankle clonus on the right. She had decreased pinprick sensation in her bilateral C5, C6, and C7 dermatomes. Motor strength was 5/5 in all upper and lower extremity muscle groups bilaterally.
Radiological Findings
Plain anteroposterior and lateral radiographs of the cervical spine (Figs. 1–1A,B) show evidence of congenital cervical stenosis, with a spinal canal diameter measuring 11 mm. Plain radiographs also demonstrated degenerative disk disease at C4-5 and C5-6 with a reversal of the normal cervical lordosis. Ossification was seen posterior to the C4-5 and C5-6 vertebral end plates and disk spaces. The C6-7 disk space and C7 vertebral body were not well visualized. A computed tomographic (CT) myelogram was obtained that showed severe cervical stenosis from C3 to C7 with ossification of the posterior longitudinal ligament (OPLL) located posterior to the C4-5, C5-6, and C6-7 disk spaces and associated vertebral end plates (Figs. 1–2A,B).
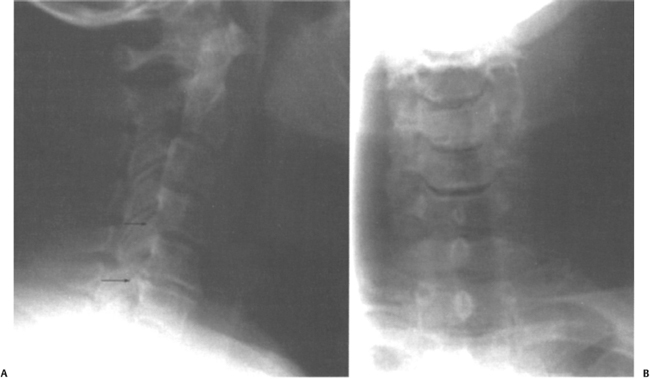
Figure 1–1 (A) Lateral and (B) anteroposterior cervical spine radiographs of the patient described in the case presentation. The anteroposterior view demonstrates areas of ossification posterior to the C4-5, C5-6, and C6-7 disk spaces and associated vertebral end plates (black arrows).
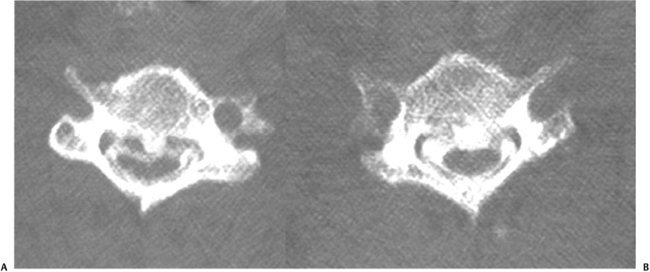
Figure 1–2 Axial computed tomographic cervical myelogram images of the patient described in the case presentation. Significant ossification of the posterior longitudinal ligament and associated cervical stenosis is noted posterior to (A) the distal C4 vertebral end plate and (B) the proximal C6 vertebral end plate.
Diagnosis
This patient was diagnosed with Nurick grade 4 myelopathy due to severe cervical stenosis from C3 to C7 with OPLL posterior to the C4-5, C5-6, and C6-7 disk spaces and associated vertebral end plates.
 | Background |
OPLL is a well described cause of cervical myelopathy and radiculopathy. Traditionally it has been considered a disease that affects those of Asian descent. More recently, however, studies have described OPLL as a significant cause of cervical myelopathy in North Americans, affecting up to 25% of patients who undergo cervical surgery for symptoms of myelopathy.1–3 Although environmental and genetic causes of OPLL have been reported, the true etiology remains unknown. There seems to be an association between OPLL and diffuse idiopathic skeletal hyperostosis, although this relationship is not fully understood. It affects males twice as commonly as females.
The pathogenesis of OPLL is not completely understood. The initial stage of the disease involves hypertrophy of the PLL, which is followed by progressive enchondral ossification of the ligament. OPLL has been classified into four types: (1) continuous (27%, i.e., behind multiple vertebral bodies and crossing disk spaces); (2) segmental (39%, i.e., disease limited to behind the vertebral bodies); (3) mixed continuous and segmental (29%); and (4) other (5%, i.e., disease limited to behind the disk spaces and vertebral end plates).2 This process often involves multiple cervical levels and may penetrate the dura, making anterior removal difficult and in creasing the risk of dural injury and cerebrospinal fluid (CSF) leakage (Figs. 1–3A,B). Neurological damage is thought to be the result of both direct compression and ischemic compromise from the hypertrophied, ossified PLL.
Patients usually present with OPLL in their fourth or fifth decade, frequently complaining of either or both upper extremity numbness and axial neck pain. Physical examination should include a thorough neurological examination for evidence of myelopathy. The diagnosis of OPLL can be made on plain cervical radiographs, which, in addition to disk space narrowing and spondylosis, can demonstrate OPLL posterior to the involved cervical levels. CT scan, however, better differentiates between OPLL and osteophytes of the posterior vertebral body and can show evidence of dural penetration of the ossified ligament (i.e., single-layer sign, C-sign, and double-layer sign4,5). Although it is not as good as CT at demonstrating OPLL, magnetic resonance imaging (MRI) does show the degree of cord compression and the presence of intrinsic changes within the cord (i.e., myelomalacia) that may have prognostic significance.
When treated conservatively, symptomatic OPLL does not tend to resolve. Matsunaga et al. reviewed 207 patients with cervical OPLL who were followed clinically for an average of 10 years and 3 months. Although 66% of patients remained free of myelopathy during the course of the study, 38% of those who presented with myelopathic signs had progression of their myelopathy and none had clinical improvement.6 For this reason, symptomatic OPLL is most often treated surgically. Numerous surgical approaches have been described for the treatment of OPLL, including laminoplasty, cervical laminectomy with or without posterior arthrodesis, and anterior decompression and arthrodesis. Successful clinical results have been reported with all of these approaches, although cervical laminectomy without posterior arthrodesis has been associated with an increased risk of postlaminectomy instability and kyphotic deformity and therefore is not recommended. Several studies that have compared anterior and posterior decompression for the treatment of OPLL report better outcomes using the anterior approach.2,7
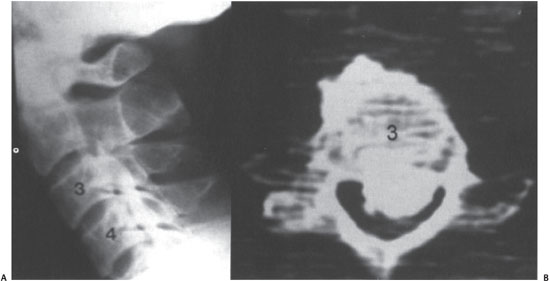
Figure 1–3 (A) A lateral cervical spine radiograph and (B) an axial computed tomographic cervical myelogram image at the level of the C3 vertebral body of a myelopathic patient with severe, continuous-type ossification of the posterior longitudinal ligament (OPLL) resulting in cervical stenosis. Note on the lateral radiograph the continuous, flowing ossification posterior to the C3 and C4 vertebral bodies. This is contrasted with the segmental type OPLL pattern seen in the patient described in the case presentation.
This chapter focuses the surgical treatment of OPLL with anterior decompression and arthrodesis. Several studies have reported a high rate of pain relief and neurological and functional improvement when treating symptomatic OPLL through this anterior approach. The extent of anterior decompression performed can range from anterior diskectomy and foraminotomy to subtotal corpectomy. This is dependent on the extent of involvement of the cervical spine as determined by the preoperative imaging modalities and clinical findings.
 | Authors’ Preferred Method of Surgical Management |
Our preferred surgical technique for the surgical treatment of symptomatic OPLL uses a left-sided Robinson-Smith approach. It allows excellent exposure of the cervical spine from C3 to C7. Whether to approach the cervical spine from the left or the right is dependent on the surgeon’s training and preference. The left-sided approach is advantageous because the left recurrent laryngeal nerve runs a consistent course between the trachea and esophagus and is therefore less susceptible to injury. Proponents of the right-sided approach site as benefits the avoidance of the thoracic duct and the favorable position for the right-handed surgeon.
Both anterior cervical diskectomy and fusion (ACDF) and anterior cervical corpectomy and fusion (ACCF) have been found to provide successful results when treating OPLL. The appropriate surgical technique is dependent on the extent of OPLL and neurological compression. The use of ACDF to treat OPLL is limited to patients who have focal disease located behind the intervertebral disk space. This type of OPLL, however (i.e., the “other” form of OPLL), makes up only 5% of cases.2 Overdistraction of the disk space to obtain visualization during an ACDF may lead to neurological injury. In our experience, ACCF is the safest approach to treating OPLL that ensures adequate exposure and thorough decompression. For this reason, the following surgical technique will focus on ACCF.
Technique for Anterior Cervical Approach
The patient is positioned supine on the operating table and general anesthesia is administered. A roll is placed underneath the patient at the midscapula level to ensure a neutral to slightly extended position of the cervical spine can be achieved. Excessive hyperextension should be avoided in patients with myelopathy or severe stenosis to prevent further canal stenosis and neurological injury. For an ACCF, Gardner-Wells tongs are placed with 5 lb of traction to assist with positioning and immobilization throughout the case. A brief period of additional traction through the Gardner-Wells tongs at the time of graft placement provides distraction that facilitates graft insertion. Heavy tape is used on both sides of the patient to pull the shoulders distally. This enables the surgeon to see the lower cervical spine on the intraoperative lateral radiograph when trying to determine the cervical level. The patient’s head is rotated slightly toward the right side (for left-sided approach). Continuous intraoperative somatosensory evoked potential (SEP) monitoring is applied and continued throughout the entire case.
Landmarks of the anterior neck that are visible or palpable prior to starting can help with placement of the incision. These include the angle of the mandible (C1–2), the hyoid (C3), the thyroid cartilage (C4–5), and the cricoid cartilage (C6). The carotid tubercle, which is a small prominence arising off of the anterior surface of the C6 transverse process, can be readily palpated just medial and deep to the sternocleidomastoid muscle (superficial) and the carotid artery (deep). The skin incision used for this approach depends on the extent of cervical involvement. A transverse to slightly oblique incision along a skin crease in the anterior neck is cosmetically pleasing and provides adequate exposure for up to a two-level corpectomy. An oblique incision placed along the medial border of the sternocleidomastoid muscle should be used when anticipating the need for a more extensive exposure. The foregoing landmarks and the involved cervical levels should be used to determine the caudal/cranial placement of the incision.
Following skin incision, superficial dissection first proceeds through the platysma, which is a broad muscle that originates from the superficial fascia of the lower neck and upper chest and inserts into the inferior border of the mandible and the superficial fascia of the face inferior to the mouth. Dissection through the platysma is performed perpendicular to the orientation of its fibers. Sharp dissection of the subcutaneous tissue from the anterior fascia of the platysma and the superficial layer of the deep cervical fascia from the posterior fascia of the platysma increases the mobility of the wound. Deep to the platysma is the superficial layer of the deep cervical fascia. This is sharply dissected from the medial border of the sternocleidomastoid muscle. Using blunt dissection through the remaining deep cervical fascia, the natural interval medial to the sternocleidomastoid (superficial) and carotid sheath (deep) and lateral to the trachea and esophagus is developed down to the pretracheal and prevertebral fascias (Fig. 1–4). The carotid pulse should be palpated deep to the sternocleidomastoid muscle during blunt dissection to ensure protection of the carotid artery. Dissection lateral to the carotid sheath places the sympathetic chain at risk and should be avoided. The pretracheal and prevertebral fascias are dissected bluntly using a Kittner dissector, exposing the anterior aspect of the vertebral bodies and intervertebral disks.8 An 18-gauge spinal needle is then placed within the exposed intervertebral disk and a lateral cervical radiograph is obtained to confirm operative level(s).
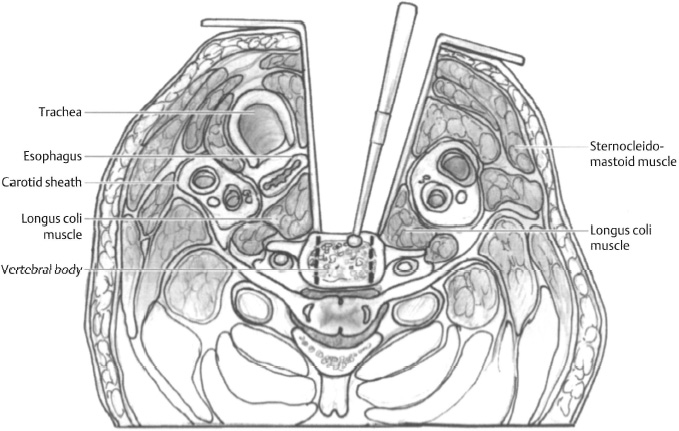
Figure 1–4 Cross-section of the neck at the level of C5 depicting the anterior approach to the cervical spine.



