Chapter 15 15.1 Thyroid Disease Hyperthyroidism is caused by diseases of the thyroid gland that result in the production of too much thyroid hormone. These include Graves disease, thyroiditis, thyroid nodules, and ingestion of too much iodine or thyroid medication. Less often, in perhaps 1% of cases, hyperthyroidism is caused by a thyroid-stimulating hormone (TSH)–secreting adenoma of the anterior pituitary. In hyperthyroidism, the excessive thyroid hormone results in general symptoms and sleep-related symptoms and findings, which are described in Table 15.1-1, Boxes 15.1-1 and 15.1-2, and Figures 15.1-1 to 15.1-4. Table 15.1-1 Figure 15.1-1 The “thyroid stare.” Figure 15.1-2 Graves ophthalmopathy. Figure 15.1-3 Polysomnogram of sweat artifact. The clinical features of hypothyroidism are those related to a hypometabolic state and those related to the effect on the cardiovascular and respiratory systems; these are described in Boxes 15.1-3 through 15.1-5, and Figures 15.1-5 to 15.1-8. Hypothyroidism is a risk factor for the development of sleep apnea and is much more common in women than in men. In particular, patients who have been diagnosed with Hashimoto thyroiditis are at risk. Figure 15.1-5 “Burned out” Graves disease. Figure 15.1-6 This figure shows the development of hypothyroidism over time. Figure 15.1-7 Features of hypothyroidism. These lesions are detected either by inspection or palpation. In patients with thyroiditis, the gland may be tender. Refer to Boxes 15.1-6 and 15.1-7 and Figure 15.1-9. Bozkurt, NC, Karbek, B, Cakal, E, et al. The association between severity of obstructive sleep apnea and prevalence of Hashimoto’s thyroiditis. Endocr J. 2012; 59(11):981–988. Misiolek, M, Marek, B, Namyslowski, G, et al. Sleep apnea syndrome and snoring in patients with hypothyroidism with relation to overweight. J Physiol Pharmacol. 2007; 58(Suppl 1):77–85. Neal, JM, Yuhico, RJ. “Myxedema madness” associated with newly diagnosed hypothyroidism and obstructive sleep apnea. J Clin Sleep Med. 2012; 8(6):717–718. Resta, O, Carratù, P, Carpagnano, GE, et al. Influence of subclinical hypothyroidism and T4 treatment on the prevalence and severity of obstructive sleep apnoea syndrome (OSAS). J Endocrinol Invest. 2005; 28(10):893–898. Resta, O, Pannacciulli, N, Di Gioia, G, et al. High prevalence of previously unknown subclinical hypothyroidism in obese patients referred to a sleep clinic for sleep disordered breathing. Nutr Metab Cardiovasc Dis. 2004; 14(5):248–253. 15.2 Diseases of the Pituitary Gland The pituitary gland is located near several structures that are involved in the regulation of sleep (Fig. 15.2-1). Above the pituitary is the hypothalamus, which contains centers involved in the regulation of sleep and temperature, and the suprachiasmatic nucleus, which is the master controller of the circadian rhythm. Figure 15.2-1 An enlarging pituitary tumor compresses structures in and around the pituitary gland. Hypersecretion of growth hormone can result in metabolic abnormalities and anatomic changes of skeletal and soft tissue structures that may result in obstructive sleep apnea (OSA). The most common cause of excess secretion of growth hormone is a pituitary tumor (see Fig. 15.2-1). The clinical presentation (Box 15.2-1) is related to the age of the patient, the local effects of the enlarging tumor on the structures in and around the pituitary gland, and the resulting metabolic and anatomic changes. When these result in orofacial changes (Figs. 15.2-2 and 15.2-3), the patient may develop OSA. Figure 15.2-2 Acromegaly evolved slowly in this patient, who developed sleep apnea. Figure 15.2-3 Acromegaly. Patients with acromegaly or gigantism generally require multispecialty management, especially if they are initially untreated. Collaboration between specialists in endocrinology and neurosurgery is usually necessary. Sleep specialists are often involved when sleep symptoms develop. Usually they are the classical ones of OSA and require polysomnography (see Chapter 13.2). Confirmation of sleep apnea is generally identical to what is done for the typical OSA patient. Borgers, AJ, Romeijn, N, van Someren, E, et al. Compression of the optic chiasm is associated with permanent shorter sleep duration in patients with pituitary insufficiency. Clin Endocrinol (Oxf). 2011; 75(3):347–353. Hernández-Gordillo, D, Ortega-Gómez Mdel, R, Galicia-Polo, L, et al. Sleep apnea in patients with acromegaly: frequency, characterization and positive pressure titration. Open Respir Med J. 2012; 6:28–33. Romeijn, N, Borgers, AJ, Fliers, E, et al. Medical history of optic chiasm compression in patients with pituitary insufficiency affects skin temperature and its relation to sleep. Chronobiol Int. 2012; 29(8):1098–1108. Sze, L, Schmid, C, Bloch, KE, et al. Effect of transsphenoidal surgery on sleep apnoea in acromegaly. Eur J Endocrinol. 2007; 156(3):321–329. Tolis, G, Angelopoulos, NG, Katounda, E, et al. Medical treatment of acromegaly: comorbidities and their reversibility by somatostatin analogs. Neuroendocrinology. 2006; 83(3–4):249–257. van Haute, FR, Taboada, GF, Corrêa, LL, et al. Prevalence of sleep apnea and metabolic abnormalities in patients with acromegaly and analysis of cephalometric parameters by magnetic resonance imaging. Eur J Endocrinol. 2008; 158(4):459–465. Vallette, S, Ezzat, S, Chik, C, et al. Emerging trends in the diagnosis and treatment of acromegaly in Canada. Clin Endocrinol (Oxf). 2013; 79(1):79–85. Watson, NF, Vitiello, MV. Management of obstructive sleep apnea in acromegaly. Sleep Med. 2007; 8(5):539–540.
Other Medical Disorders
Hyperthyroidism
CAUSES
FEATURES
Graves disease
Hyperthyroidism, goiter, ophthalmopathy, pretibial myxedema; may remit
Toxic goiter
A result of hypersecretion of thyroid-stimulating hormone, but does not usually remit
Thyroiditis
Hyperthyroidism during acute phase; may “burn out”
Related to drugs
Lithium and amiodarone


A, The patient appears startled. This finding is the result of eyelid retraction likely caused by sympathetic overactivation; it does not mean that Graves disease is present. B, Hyperthyroidism is much more common in females.




A, Corneal injection and proptosis. Extraocular muscle weakness on left lateral gaze (B), right lateral gaze (C), and upward gaze (D). The patient reported double vision.
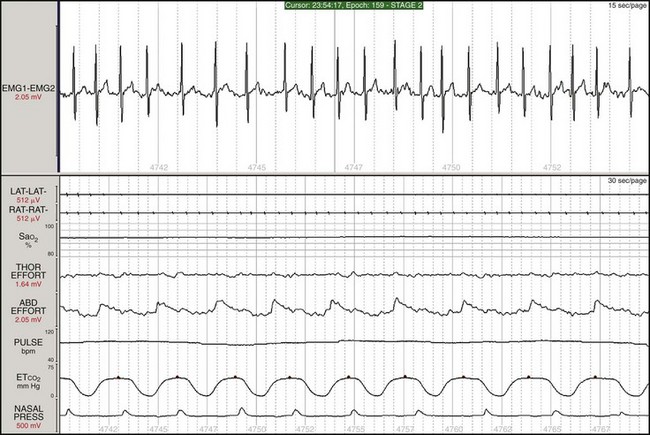
Note the high-amplitude swings in all the electroencephalogram channels in synchrony with breathing. This patient had night sweats. Hyperthyroidism was first suspected from this finding and from the newly noted atrial fibrillation. Top and bottom windows are 30-second epochs.
Hypothyroidism



A, This patient, who had been treated for Graves disease, developed severe hypothyroidism with obesity and sleepiness and was found to have severe obstructive sleep apnea. Note the conjunctival injection and the droopy lids. B, When the patient is focused and alert, the eye signs of proptosis and the asymmetry of eye movements become apparent. C, The characteristic bulging eyes (exophthalmos) of Graves disease.
The patient developed coarse facial features, puffy eyes, and cold intolerance. Note that the patient is wearing a scarf indoors.
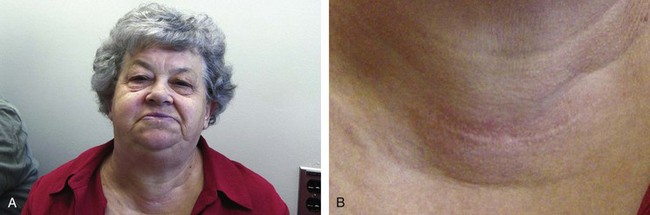


A, Puffy eyes. B, Fullness in the neck and a scar from thyroid surgery. C, A large tongue (macroglossia) fills up the mouth, impinging on the oropharyngeal airway. D, Brittle, sparse hair, receding hairline, and loss of hair in eyebrows.
Thyroid Mass Lesions
Anatomy
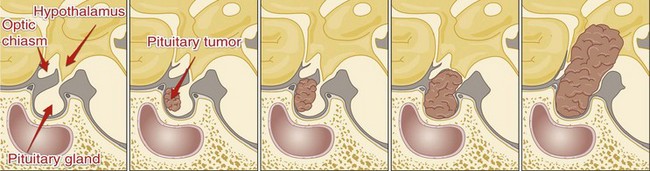
These structures have an effect on the regulation and timing of sleep.
Growth Hormone Hypersecretion
Pathophysiology
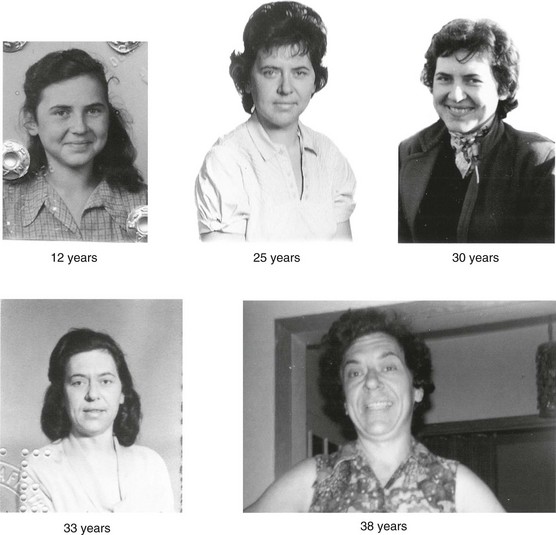
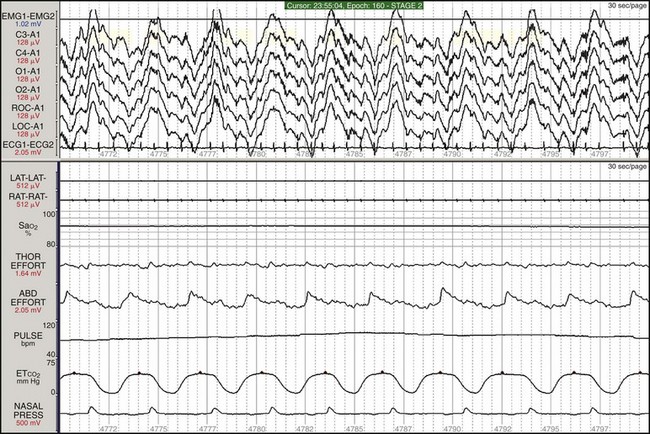
These photographs show the changes in facial features over many years. Between ages 33 and 38, a marked coarsening of the features occurs. Note the distance between the eyebrows and that the eyes increased in size because of the bossing of the forehead. Sleep apnea symptoms also developed slowly.





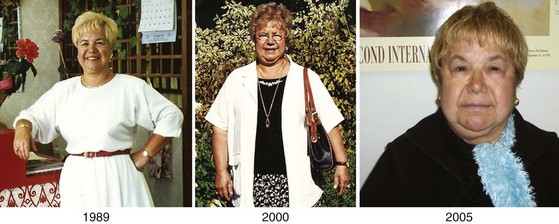
A, This is the same patient as shown in Figure 15.2-2, now in her 60s. A large jaw and nose, frontal bossing, coarse facial features, thick skin, and deep facial creases are apparent. The sleep apnea is believed to be due to the anatomic changes, including the enlarged tongue (B) and the abnormal jaw structure. This patient has severe obstructive sleep apnea and has been on nasal continuous positive airway for several years. C, Examination of the lower jaw and dental structures reveals increased space between the teeth caused by enlargement of the jaw. D, Note the frontal bossing and the healed scar from surgery to treat the pituitary tumor. In some patients, the lower jaw juts forward (prognathism). E, One of the first signs the patient noted was enlargement of her hands.
Diagnosis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Other Medical Disorders
Only gold members can continue reading. Log In or Register to continue