Fig. 16.1
Dramatic curve correction achieved by using two-level PSO following bilateral total hip replacements (Chen et al. [5], published with permission)
Bridwell performed lumbar PSO for the treatment of fixed sagittal imbalance in 27 consecutive patients [6]. The mean C7 sagittal plumb line for all patients improved from 17.74 ± 7.95 cm preoperatively to 1.99 ± 3.91 cm at two months postoperatively (P < 0.0001). At the minimal 2-year final follow-up, it had increased to 4.23 ± 6.73 cm but was still significantly better than the preoperative value (P < 0.0001). Also, there was a significant increase in the mean standing height of the patients, from 156.87 cm preoperatively to 160.30 cm at the final follow-up.
These operations are not without potential complications, however. Many authors have restricted PSO’s use to cases with a kyphotic angle less than 40°, because more substantial correction may lead to buckling of the spinal cord. In treating thoracolumbar kyphosis with PSO, Lehmer et al. found that one-third of the patients who developed postoperative neurological deficits had dural buckling and their symptoms were alleviated after revision surgery [7]. He therefore concluded that “correction at any one level should not exceed approximately 35°,” which was the average correction degree at each osteotomy in his series [7].
After the “eggshell” technique, whereby the vertebral body is decancellated via the pedicle, was developed in the 1970s, it was merged with PSO in an attempt to treat complex spinal deformity more safely. The decancellation converts a solid vertebral body to a thin shell of cortical bone which can then be easily broken and the spinal alignment manipulated. Murrey et al. applied an “eggshell” PSO in 59 “complex” cases of deformity or osteopathy [8]. However, the immediate sagittal correction averaged 26.2°, which implies the limitation of “eggshell” PSO in dealing with severe deformity.
16.1.2 Clinical Outcomes
In Thomasen’s early report on PSO used for the treatment of AS in 11 patients, no fatal complications occurred [3]. There was one revision surgery for postoperative deterioration of neurological function due to osteotomy segment shifting. Six of the nine patients who responded to the satisfaction degree survey reported “satisfied” or “very satisfied.” At the final follow-up (2–23 years), four of the eight living patients were at work, the others received retirement/disability pension.
In Chen et al. (Taiwan)’s AS kyphosis series of 78 patients undergoing PSO, there were no vascular injuries [5]. Root injury caused by electrocautery occurred in one case and led to transient L2 paralysis. Cerebrospinal leakage was encountered in three and all resolved after appropriate drainage. Immediate implant loosening occurred in one patient with osteoporosis, who then received successful revision surgery and body cast treatment. A 5 % infection rate was reported but all the four patients were successfully treated by debridement or removal of implants and their initial correction was well maintained. At the final follow-up, 83 and 15 % of all patients reported “excellent” and “good” results, respectively.
Bridwell was one of the early users of validated outcome measurements in evaluating the clinical outcomes of lumbar PSO in 27 consecutive fixed sagittal imbalance patients, including before-and-after visual analog scale (VAS) pain score, Oswestry dysfunction index (ODI), and the Scoliosis Research Society (SRS) questionnaire [6]. The average VAS score was 6.96 preoperatively and 4.41 postoperatively (P = 0.0002). In 24 patients who completed the ODI questionnaires, the average ODI score was 51.21 preoperatively and 35.75 postoperatively (P < 0.0001), a clinically significant improvement in minimal clinically important difference (MCID). In SRS outcomes data, 25 of 26 patients believed that they looked better and 24 were “satisfied” with their treatment; 23 of the 26 patients would have the procedure again and three were not sure. The early and late complications were comparable to those of Chen (Taiwan)’s.
As mentioned above, Murrey et al. applied the “eggshell” PSO in 59 “complex” cases of spinal deformity, tumor, and infection [8]. Correspondingly, they assessed the procedure’s efficacy in achieving spinal canal decompression, fusion, deformity correction, and functional improvements. With neurological status, all the 31 neurological intact patients and the four complete cord injury patients remained unchanged after surgery in terms of neurological function. Fourteen patients with incomplete cord injury showed neurological improvement, with two patients improving three Frankel grades from B to E. No perioperative deaths occurred. The overall complication rate was 16.9 % (10 patients), including three respiratory complications and four hardware failures. Although preoperative pain data was not available, VAS scores at >2-year final follow-up averaged 3.7 ± 2.8 out of 10, with 60.4 % of the patients using no medication or nonsteroidal anti-inflammatory drugs only. The average score on the Modified Prolo Economic Scale was 3.6 (5 = best, 1 = worst) at follow-up, implying that patients were working but returned to a less demanding job. Modified Prolo Functional Scale measurements averaged 3.0, indicating that patients were self-sufficient but still frequently unable to return to preinjury activity level. SF-36 scores at >2-year follow-up were significantly worse than normal (P < 0.001, scores not reported). Nonetheless, at >2-year follow-up, 92.6 % of the patients were either “completely satisfied” or “relatively satisfied.”
In general, as a three-column osteotomy technique, PSO can thus be used to treat spinal deformity with subsevere curvature effectively and safely. It also has the capacity to correct some extremely severe deformity when performed over more than one level.
16.2 Outcomes of VCR in Severe Spinal Deformity
Compared with PSO, the more complicated osteotomies including VCR and VCD are better options in the treatment of severe spinal deformity. In 1997, Bradford et al. first reported their results using a combined approach of anterior–posterior VCR [9]. In 2002, Suk et al. introduced the technique of posterior-alone VCR (PVCR) to mitigate the technical difficulties and risks associated with a two-stage procedure [10]. PVCR has since become popular and widely used by many surgeons for correction of severe spinal deformity. There is also a range of VCR variations from the conservative version to the very aggressive version.
16.2.1 Radiological Outcomes
In Bradford et al’s first report of anterior–posterior VCR used in 24 patients with rigid coronal decompensation, scoliosis averaged 103° before surgery (range 44°–157°) and 49° at 2-year follow-up (range 8°–92°), representing 52 % improvement [9]. Coronal and sagittal decompensation were corrected an average of 82 and 87 %, respectively.
Suk et al. reported their results of PVCR in 70 patients with congenital kyphoscoliosis, postinfectious kyphosis, and adult scoliosis [10]. The deformity correction was 61.9 % in the coronal plane and 45.2 % in the sagittal plane. In patients with adult scoliosis, preoperative scoliosis of 111° ± 25° was corrected to 50° ± 20° postoperatively, showing an immediate correction of 56.4 %, comparable to those of Bradford’s anterior–posterior VCR (Fig. 16.2 ). On the other hand, as we will discuss later, these results were achieved with a shorter operation time, less blood loss, and lower rate of complications. In 2004, Suk et al. published another paper to evaluate the utility of PVCR, focusing on severe rigid scoliosis [11]. In a total of 16 patients (averaging age 29 years), the mean preoperative scoliosis of 109.0° was corrected to 45.6° (59 % correction) at the minimum 2-year follow-up. The mean preoperative coronal imbalance of 4.0 cm was improved to 1.0 cm at follow-up; and the sagittal imbalance of 4.2 cm was improved to 1.6 cm.
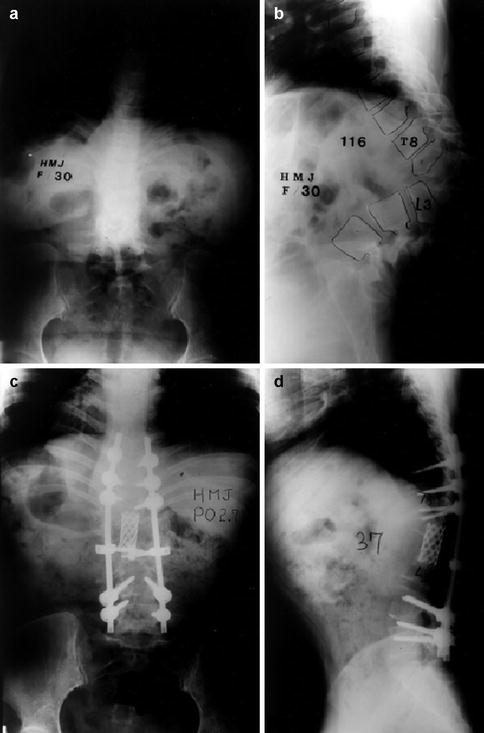
Fig. 16.2
A 30-year-old female with 116° kyphosis treated with six-level PVCR from T9 to L3. The curve was corrected to 37° postoperatively (Suk et al. [10], published with permission)
Lenke et al. applied PVCR in the treatment for severe pediatric deformity including scoliosis, kyphosis, and kyphoscoliosis [12]. Between 2000 and 2005, 35 consecutive adolescents averaging 11 years of age received surgery and all of them completed the minimal 2-year follow-up. The major curve correction averaged 24°–98° (51–60 %), according to deformity type. The authors concluded that “dramatic radiographic and clinical correction of these deformities can be obtained via a posterior-only approach.”
In recognizing that spinal osteotomy by a single posterior approach can be potentially dangerous, especially in patients with progressive neurologic dysfunction, Song et al. combined an anterior VCR and fusion with an in situ posterior fusion to treat severe angular kyphosis (>70°) with myelopathy in 16 patients [13]. It was natural that the deformity correction was not ideal, as the mean local kyphosis angle at final follow-up was 74° (range, 35°–102°). However, solid bony fusion was achieved in all patients and significant kyphosis progression did not occur during the mean follow-up period of 72 months (32–168 months).
At the aggressive extreme is a PVCR procedure reported by Chen et al. (Beijing) in 2011 as “apical segmental resection osteotomy with dual axial rotation corrective technique” [14], which emphasized the osteotomy covering the “entire apical area of kyphosis,” severing the anterior longitudinal ligament, and coordinated rotation of both cephalic and caudal osteotomies during correction, in an attempt to avoid inadequately shortening or distracting the spinal cord. Twenty-three patients who had severe focal kyphosis underwent this procedure. The average kyphotic angle improved from 86.9° preoperatively to 25.6° immediately postoperatively and 27.4° at 2-year follow-up, making the final correction rate 69.87 %.
16.2.2 Clinical Outcomes
In Bradford et al’s report of anterior–posterior VCR, all 24 patients rated their results as either good or excellent [9]. However, the operation time exceeded 10 h in 75 % of the patients, and the blood loss exceeded 5,000 ml in 33 % of the patients. Also, 58 % of the patients had complications with a reoperation rate of 25 %. The most common complication was dural tear, two of which occurred during the anterior approach and thus could not be repaired. Nevertheless, despite the pitfalls, these data clearly demonstrate that staged anterior–posterior VCR can be an effective albeit formidable procedure for severe spinal deformity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








