30
Oxygen Administration in the Sleep Center
STEVEN H. LENIK
NOTE: This chapter corresponds to Chapter 36 in Fundamentals of Sleep Technology, 2nd edition.
OXYGEN STORAGE AND DISTRIBUTION
1. What is the primary source of oxygen available to you in a freestanding sleep center?
A. Compressed oxygen
B. Liquid oxygen
C. Piped gas
D. Oxygen concentrators
2. The sleep center is located on a floor in the hospital. What is the most likely source of oxygen delivery?
A. Compressed oxygen
B. Liquid oxygen
C. Piped gas
D. Oxygen concentrators
OXYGEN DELIVERY DEVICES
3. What are the types of devices used to administer oxygen to your patient? Name two.
INTERVENTION
4. Describe when to begin administering the oxygen to your patient.
TITRATION
5. Explain how to titrate oxygen during a sleep study.
PRECAUTIONS
6. How can oxygen be dangerous to a patient?
RECORDING AND DOCUMENTATION
7. What needs to be documented?
A. Current medications
B. Current use of oxygen
C. Oxygen liter flow
D. All of the above
8. How do I record oxygen use on the PSG?
A. PSI
B. cm/H2O
C. lpm
D. mm Hg
CASE STUDY NO. 1
A patient arrives at your sleep center for a polysomnogram, and the orders state, “Titrate O2 if sats remain below 90%.” You begin to prepare for the procedure by carefully reviewing the patient’s medical history. You note that the patient complains of shortness of breath with activity (exertional dyspnea) and at night, with occasional waking with gasping. He also complains of constant fatigue. The patient is slightly obese (BMI = 30), and is taking medication for hypertension (lisinopril and hydrochlorothiazide) and type II diabetes (metformin and glyburide). The patient had an overnight oximetry study (which is not in the chart), and the lowest oxygen saturation of the night was 76%. There is no mention of pulmonary disease or that the patient is currently using supplemental oxygen.
9. What should you do to treat this patient?
CASE STUDY NO. 2
An elderly patient is sent for a polysomnogram with a long history of smoking and smoke inhalation (>50 years). She is thin for her height (BMI = 18.1) and rather frail looking. Her complaints include frequent waking with inability to breathe at night, depression, panic attacks, coughing, wheezing, and daytime sleepiness. There are no orders regarding oxygen use on this patient.
After beginning diagnostic study, you observe a few central breathing events and even fewer obstructive breathing events in the first hour, along with many periodic limb movements. In the second hour of the study, the patient enters REM sleep and immediately begins to desaturate below 85%. Long periods of decreased airflow are noted, but they do not meet the criteria for hypopneas (Fig. 30-1).
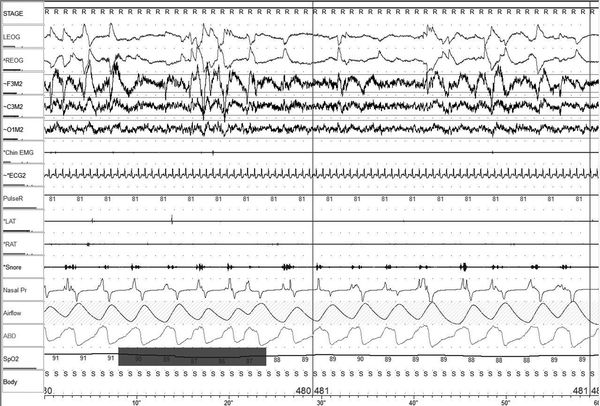
Figure 30-1 Example PSG for Case Study no. 2.
10. What do you do now?
CASE STUDY NO. 3
A pediatric patient undergoing polysomnography has a history of premature birth with low birth weight and has developed bronchopulmonary dysplasia as a result of respiratory distress syndrome and subsequent mechanical ventilation. The polysomnogram has been ordered to rule out pediatric sleep apnea. The patient is currently on continuous supplemental oxygen at 2.5 lpm.
The test is started (per doctor’s orders) with the patient on usual oxygen flow via nasal cannula. As the test progresses, the child demonstrates a large number of respiratory events, both obstructive and central. There are also what appear to be hypopneas, albeit without sufficient desaturation to score them.
11. What treatment is appropriate?
ANSWERS
1. D, Oxygen concentrators.
2. C, Piped gas.
Compressed oxygen comes in canisters (or tanks) of varying sizes. They are most useful for portable or emergency oxygen delivery. If the patient arrives with one, it will be a smaller size (for instance, “E” cylinder) that probably does not hold enough gas to last the length of the study. You will need to supply your own supplemental oxygen. If your lab uses compressed gas, it is probably a larger tank (for instance, “H” cylinder): These will last quite a while but are bulky, unwieldy, and not very practical. They need to be secured to a wall or flooring, inspected, and replaced regularly. These tanks will have a pressure and flow regulator, which must be set and adjusted appropriately, and you will need to run a tube from the regulator to the patient’s oxygen interface, which may be a significant distance from the tank.
Liquid oxygen comes in tanks that are much smaller than compressed gas tanks. These are ideal for portable use, but rather expensive for use in a sleep lab. If the patient brings one, it will have a built-in flow regulator. Otherwise, you will have to provide a flow regulator. The advantage of liquid oxygen is that a tank can hold much more liquid than it would gas.
Many hospitals and clinics provide piped oxygen, usually available in the patient’s room via a wall plate. This gas is most likely coming from a very large reservoir of liquid gas located elsewhere on the facility campus. The liquid is checked and refilled regularly by maintenance personnel. This is one of the most convenient ways to supply supplemental oxygen to your patients, if available. A specific wall adapter regulator must be used to ensure only oxygen is delivered, since many of these wall plates are right next to compressed air and vacuum outlets that look similar.
Most freestanding sleep laboratories resort to oxygen concentrators for regular use. These are hardy and economical machines that extract oxygen from the air (by filtering out the nitrogen) and deliver 95% or greater concentrations of oxygen. The machines are slightly bulky, run on electricity (so you need to be near an AC outlet), and tend to be fairly noisy. It is not uncommon to position the machine outside the patient’s room and run a fairly long oxygen hose into the room to keep the noise from disturbing the patient during the test. The concentrator should come fitted with an adjustable flow regulator (Fig. 30-2).

Figure 30-2 Oxygen concentrator.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




