Chapter 155 Paracoccygeal Transsacral Approach to the Lumbosacral Junction for Interbody Fusion and Stabilization
The interbody space can be approached from the ventral, dorsal, and direct lateral approaches. Each of these approaches has its limitations. Anterior interbody fusions allow for the instrumentation to be placed along the long axis of the spine, which has been shown to demonstrate favorable biomechanics, because the instrumentation is placed close to the instantaneous axis of rotation of the spine and perpendicular to the compressive moments of the vertebral bodies. The ventral exposure techniques to the lumbosacral segment have evolved from transperitoneal to retroperitoneal and even laparoscopic approaches. However, these exposures require mobilization of the abdominal contents and vascular structures, and this carries an element of risk and also frequently involves specialized expertise to perform the exposure safely. The use of interbody implants with these exposures necessitates partial resection of the anulus to place the implant. This, in turn, may contribute to a destabilizing effect on the spine despite the use of a specific implant. In response to the limitations of these contemporary exposures and techniques for lumbosacral fusions, Cragg et al.1 recently described a novel percutaneous, fluoroscopically guided, access method to the lumbosacral junction. The access is gained through a paracoccygeal incision with blunt dissection through the presacral space, all while the patient is positioned prone. This approach allows for axial transsacral access to the lumbosacral junction. Along with this exposure, specially designed tools to evacuate the disc space, prepare the end plates, and introduce graft material, as well as a specialized axial stabilization rod, have all been developed to facilitate a minimally invasive fusion of the lumbosacral junction.
Presacral Anatomy
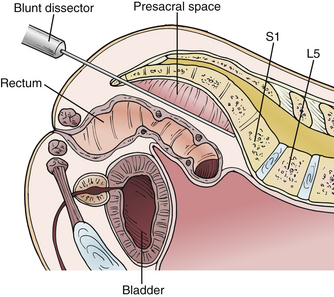
The paracoccygeal presacral access to the lumbosacral junction takes advantage of a well-defined anatomic potential space between the anterior surface of the sacrum and posterior surfaces of the sigmoid colon and rectum (Fig. 155-1). This presacral space is bounded by visceral fascia on the sigmoid colon and rectum and by parietal fascia on the anterior surface of the sacrum. The presacral space is filled with areolar tissue and fat. The rectum and sigmoid colon are not attached to any structures in the course of the presacral space; therefore, they can be easily mobilized with a blunt dissector. It is important to keep the dissection limited to the midline presacral space. The sacral nerve roots exit the foramina and course laterally and inferiorly, away from the midline presacral space. Because this space is devoid of any significant vascular or neurologic elements, there are no obstacles to establishing a corridor for access.
Yuan et al. studied the anatomic relationships of the presacral space.2 These investigators reported that at the lumbosacral junction the iliac vessels and their accompanying sympathetic hypogastric nerves coursed laterally over the sacral ala. In the midline just beyond the lumbosacral junction, the midline sacral artery and vein follow a variable course and typically terminate in a fine reticular mesh. They defined the coronal safe zone at the S1-2 interspace as more than 6 cm wide in both males and females on the basis of CT and MRI measurements. Therefore, at the typical docking and entry point into the sacral promontory, which is usually at the S1-2 junction, there are no significant obstructions.
Parke et al. described the variability of the middle sacral artery in 20 cadavers, reporting that in humans, it is only a minor contributor to any major segmental arteries, through bilateral segmental branches.3 Furthermore, it was found to be absent in many specimens. Using 10 cadavers and MRI studies, Güvençer et al. measured the distances between the sacrum and the presacral structures (i.e., middle and lateral sacral arteries, sympathetic trunks, internal iliac arteries and veins, and colon/rectum).4 This cadaver study showed that the middle sacral artery was located on the right side in 55.0% of cases, on the left side in 31.7%, and on the midline in the 13.3%. The distance between the sacral midline and middle sacral artery was 8.0 ± 5.4, 9.0 ± 4.9, 8.7 ± 6.0, 8.6 ± 6.4, and 4.7 ± 5.0 mm at the S1-2, S2-3, S3-4, S4-5, and S5-coccyx levels, respectively. The distance between the sacral midline and the sympathetic trunk ranged between 22.4 ± 5.8 and 9.5 ± 3.2 mm in different levels between the S1 and coccygeal levels. The study also showed that the distance between the posterior wall of the intestine (colon/rectum) and the ventral surface of the sacrum can be as close as 11.44 ± 7.69 mm on MRI. Because of the close relationships, as well as the potential for anatomic variations, the authors recommended the use of sacral and presacral imaging before a presacral approach. Oto et al.5 described the sagittal width of the presacral space at the S1, S2, and S3 vertebral levels retrospectively on MRI in 193 patients. The researchers found that (1) the presacral width in males was significantly wider than in females and (2) in general, the presacral space was at least 1 cm wide in more than 60% of males and 40% of females.
Evolution of Technique
The paracoccygeal presacral access to the lumbosacral junction was validated in a series of cadaver, animal, and human trials. Cragg et al., in a series of 15 cadavers, refined the access technique and the necessary instruments.1 The instruments evolved to include dissectors, cannulae, drills, discectomy tools, bone graft application tools, and axial rod implantation tools. The investigators validated the procedure with a fully percutaneous fluoroscopic approach through a single 2-cm paracoccygeal incision. Cragg et al. then assessed the safety of the access procedure in a series of six consecutive animals.1 The access was performed without adverse events. Lumbosacral access in the animals was confirmed fluoroscopically by axial discography. Following the success of the preclinical studies, the researchers undertook a series of consecutive biopsies of the lumbosacral disc and vertebral body region for suspected pathologic lesions in three patients.1 Again, the technique posed no significant issues.
Surgical Procedure
Preoperative Planning
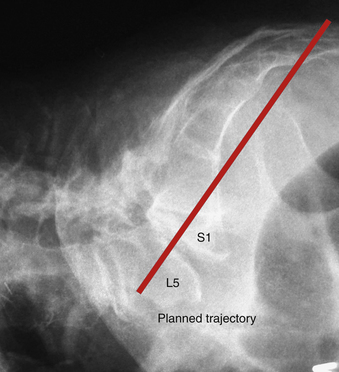
In preparation for the surgical approach, the radiographic images, including a full sacral view, are analyzed to determine if the anatomy is suitable for the paracoccygeal transsacral approach to the lumbosacral junction. The standard field of view for a lumbar MRI scan should be expanded to include the entire sacrum and coccyx on the sagittal views. With the radiographs and MRI scans, one can plan and map the trajectory of the access and subsequent implantation of the axial rod (Fig. 155-2).
Patient Preparation
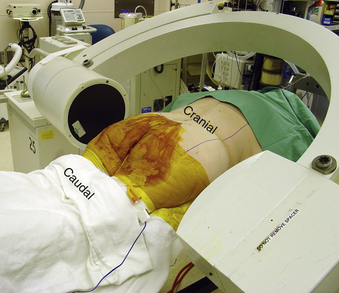
Typically, a standard bowel preparation the evening before surgery is advisable. In the operating room, the patient is positioned prone onto a radiolucent table with the lumbar spine in extension to facilitate lumbar lordosis. The lumbar and the sacrococcygeal regions are prepped and draped. The operative area should be isolated from the anus with an occlusive dressing (Fig. 155-3).
Operating Room Setup
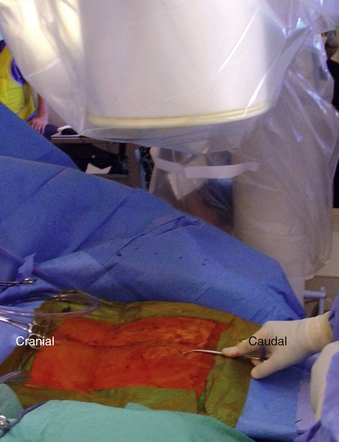
Once the patient is positioned, two image intensifiers are positioned for simultaneous biplanar fluoroscopy. The posteroanterior C-arm should be adjusted to project a lordotic view of the lumbosacral junction. The lateral C-arm should be adjusted to achieve a true lateral view of the lumbosacral junction. The lateral and anteroposterior C-arms should be draped such that they can move in a parallel fashion from the tip of the coccyx to the lumbosacral junction freely as needed throughout the procedure (Fig. 155-4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree