Differential CSF Analysis
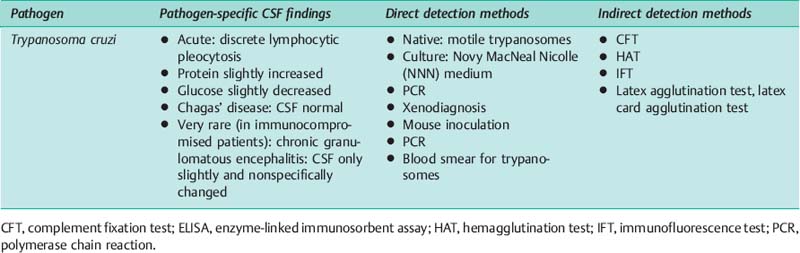
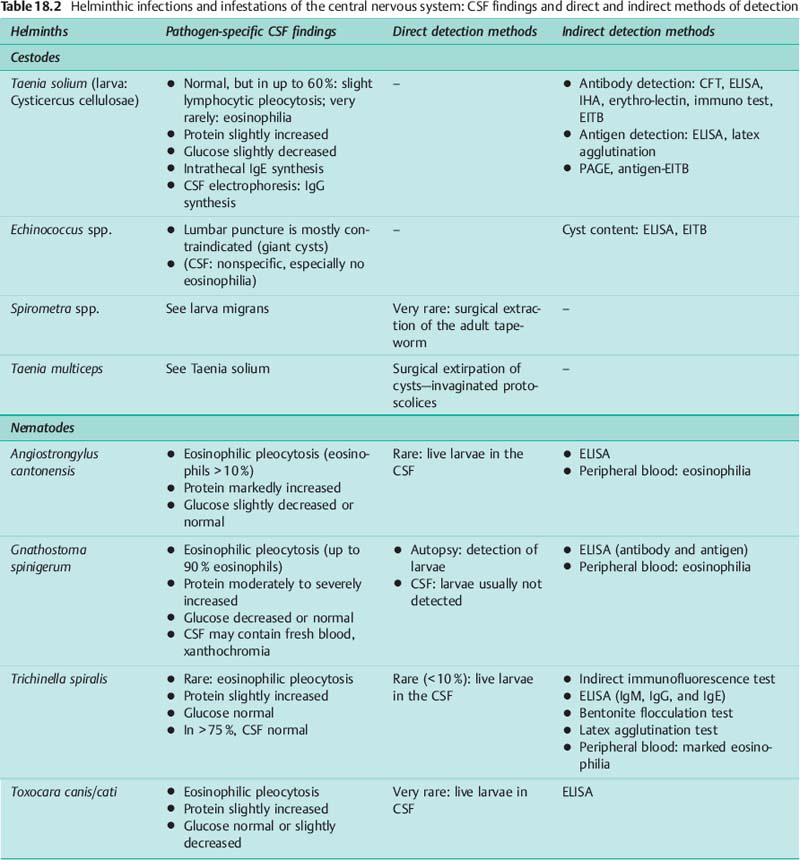
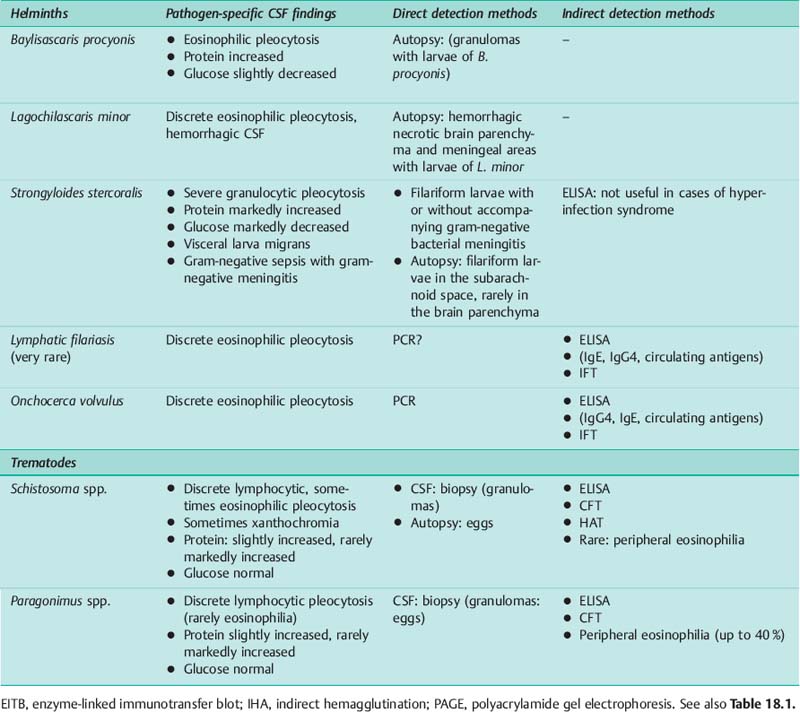
Eosinophilia. Many parasites invade the cerebrospinal fluid and/or the CNS parenchyma, usually at specific stages of their development. This facilitates direct detection of the pathogen by stereotactic brain puncture, aspiration of abscesses or cysts, or by lumbar puncture. The main indirect method of detection is characterization of the immune responses in the CSF. Eosinophilia in CSF and blood has an important part in directing suspicion toward parasitosis (Table 18.3).
Stage-dependent patterns of pathological response. CSF protein data can change dramatically between an early diagnostic puncture and the one performed 7 days after the onset of clinical symptoms, as illustrated in Fig. 18.1 for meningoencephalitis in children caused by Angiostrongylus cantonensis, a nematode endemic to Cuba. Apart from the eosinophilia which dominates the cytological picture, initially only a blood–CSF barrier dysfunction without a humoral immune response is observed. Just 7 days after the onset of clinical symptoms, however, the albumin quotient has normalized, and a humoral two- or three-class immune response has occurred.
This example is representative for early dynamics of CSF data patterns.
• Diseases with a dramatic fast appearance of symptoms (see also bacterial meningitis) are analyzed in the early stage of pleocytosis and severe barrier dysfunction.
• The humoral immune response appears no earlier than 7 to 14 days after onset of disease with normalizing barrier dysfunction.
• Chronic diseases with late recognition of symptoms are analyzed in the later stage with a humoral immune response but almost normalized barrier dysfunction (neurotrypanosomiasis, Fig. 18.2).
Trypanosomiasis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree