1 Parasomnias can be misdiagnosed and inappropriately treated as a psychiatric disorder.
2 Parasomnias can be a direct manifestation of a psychiatric disorder, e.g. dissociative disorder, nocturnal bulimia nervosa.
3 The emergence and/or recurrence of a parasomnia can be triggered by stress.
4 Psychotropic medications can induce the initial emergence of a parasomnia, or aggravate a preexisting parasomnia.
5 Parasomnias can cause psychological distress or can induce or reactivate a psychiatric disorder in the patient or bed partner on account of repeated loss of self-control during sleep and sleep-related injuries.
6 Familiarity with the parasomnias will allow psychiatrists to be more fully aware of the various medical and neurological disorders, and their therapies, that can be associated with disturbed (sleep-related) behaviour and disturbed dreaming.
7 Parasomnias present a special opportunity for interlinking animal basic science research (including parasomnia animal models) with human (sleep) behavioural disorders.
8 Parasomnias carry forensic implications, as exemplified by the newly-recognized entity of ‘Parasomnia Pseudo-suicide.’ Also, psychiatrists are often asked to render an expert opinion in medicolegal cases pertaining to sleep-related violence.
1 Clinical sleep-wake interview, with review of medical records, and review of a patient questionnaire that covers sleep-wake, medical, psychiatric and alcohol/chemical use and abuse history, review of systems, family history, and past or current physical, sexual, and emotional abuse.
2 Psychiatric and neurologic interviews and examinations, including psychometric testing.
Table 4.14.4.1 Classification of parasomnias: primary and secondary sleep phenomena
Primary sleep phenomena
Non-REM sleep
Disorders of arousal: sleepwalking/sleep terrors/confusional arousal
REM sleep
REM sleep behaviour disorder (RBD)
Dream anxiety attacks (nightmares)
Miscellaneous (including mixed non-REM/REM sleep)
Parasomnia overlap disorder (sleepwalking/sleep terrors/RBD)
Sleep related eating disorder
Restless legs syndrome/periodic limb movements in sleep
Obstructive sleep apnoea-related parasomnias
Rhythmic movement disorders
Status dissociatus
Bruxism
Secondary sleep phenomena
Central nervous system
Seizures (conventional, unconventional)
Headaches
Psychiatric
Nocturnal dissociative disorders
Nocturnal panic attacks
Nocturnal bulimia nervosa
Post-traumatic stress disorder
Cardiopulmonary (arrhythmias, asthma, etc.)
Gastrointestinal (gastro-oesophageal reflux etc)
Malingering
Modified from Mahowald and Ettinger.(7)
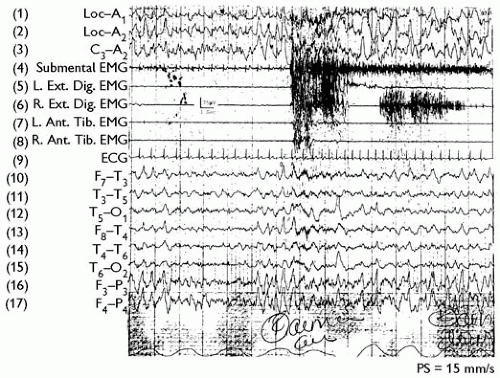
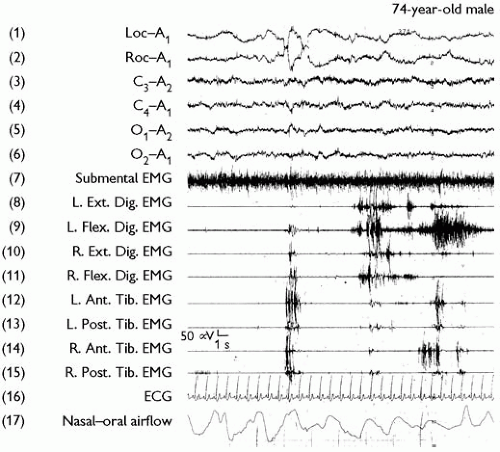
3 Extensive overnight polysomnographic monitoring at a hospital sleep laboratory, with continuous audio-visual recording. Figures 4.14.4.1, 4.14.4.2 depict the polysomnographic montage that includes the electro-oculogram, EEG, chin and four-limb electromyograms, ECG, and nasal-oral airflow (with full respiratory monitoring whenever indicated). Polysomnographic recording speeds of 15 to 30 mm/s are employed in order to detect epileptiform activity. Urine toxicology screening is performed whenever indicated.
4 Daytime multiple sleep latency testing, if there is a complaint or suspicion of excessive daytime sleepiness or fatigue (methods discussed in Narcolepsy chapter).
1 Sleepwalking/sleep terrors (M:F 3:2; mean age of onset, 5 years);
2 REM sleep behaviour disorder (predominantly male; mean age of onset, 57 years)
3 Dissociative disorders (Mostly female mean age of onset, 21 years)
4 Nocturnal seizures (uncommon)
5 Obstructive sleep apnoea/periodic limb movements (uncommon).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree