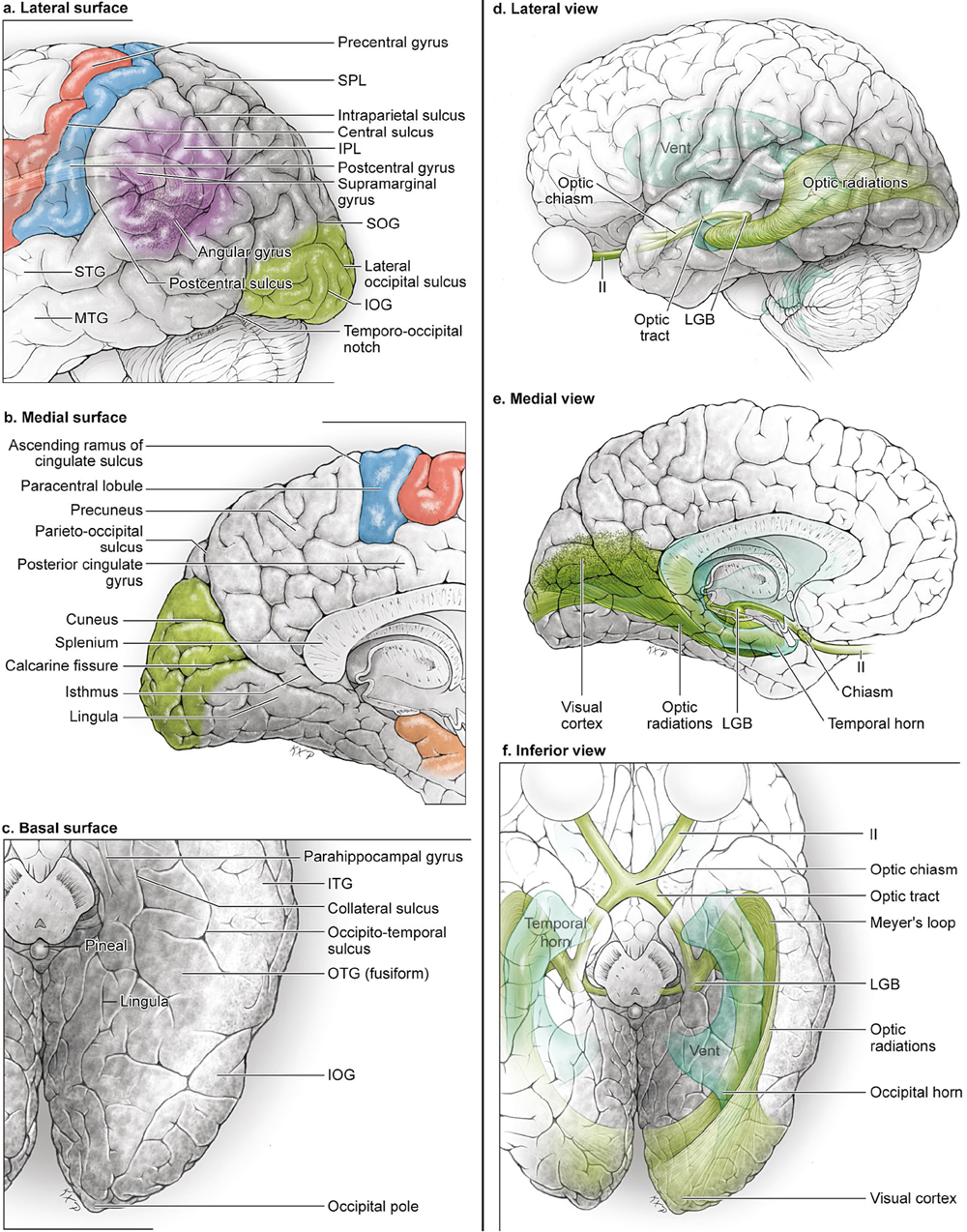
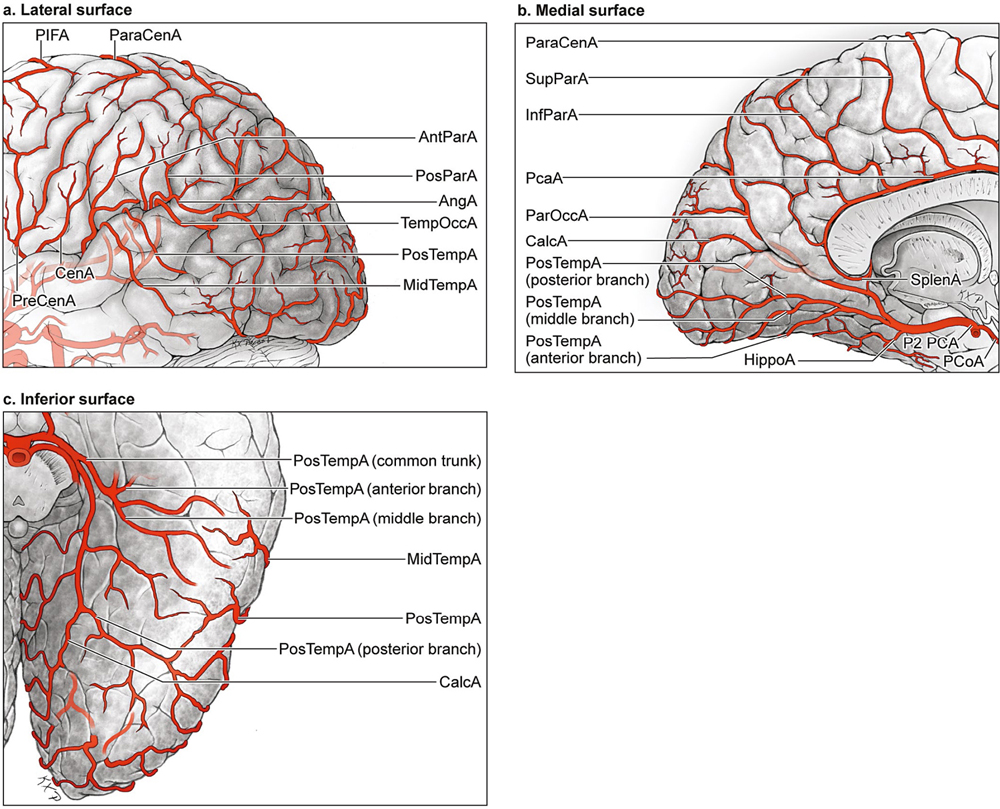
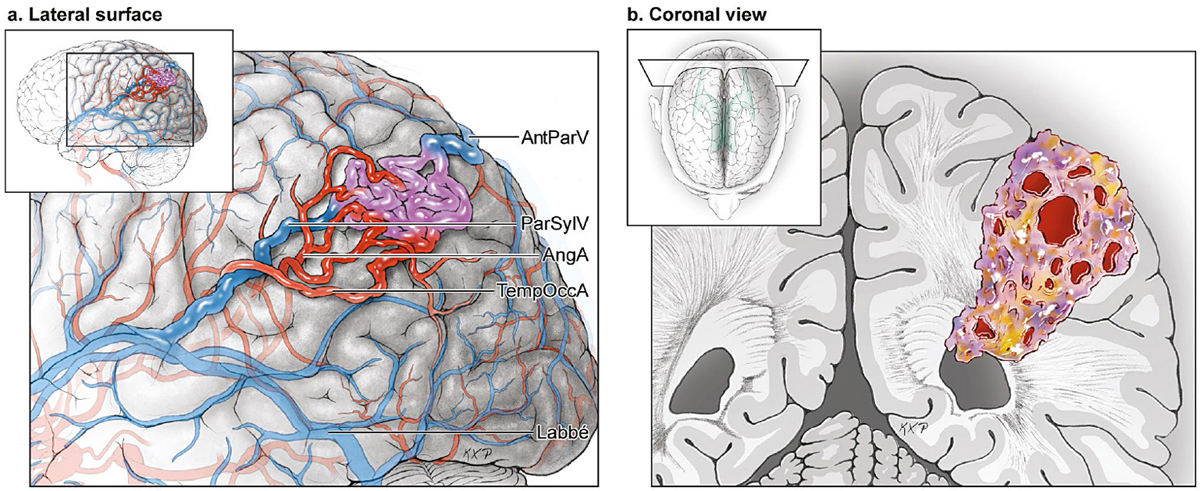
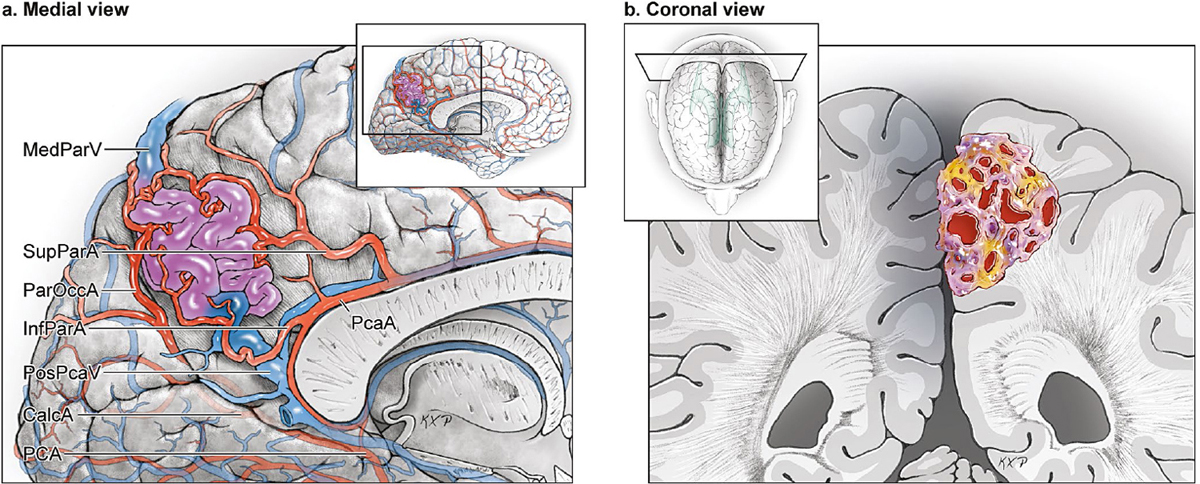
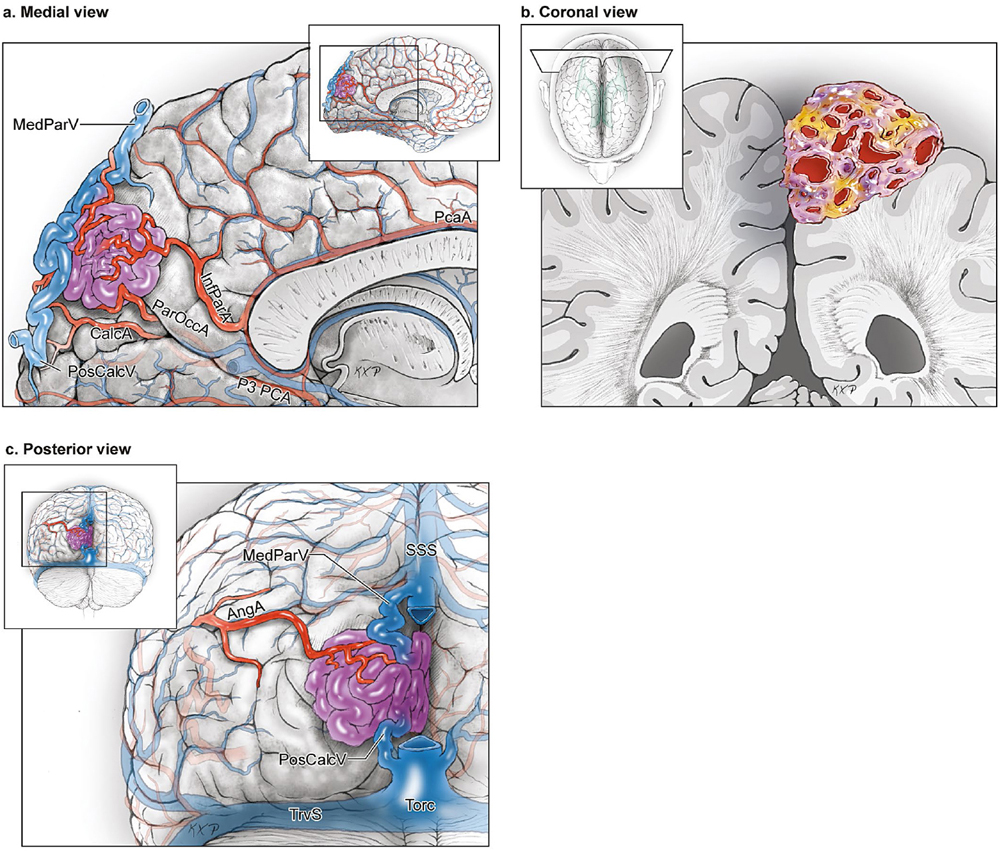
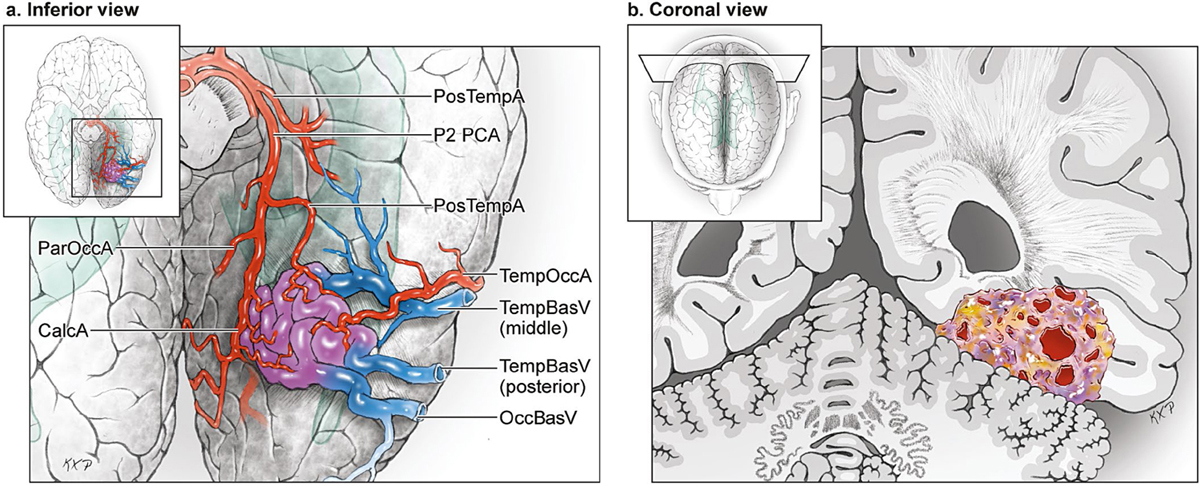
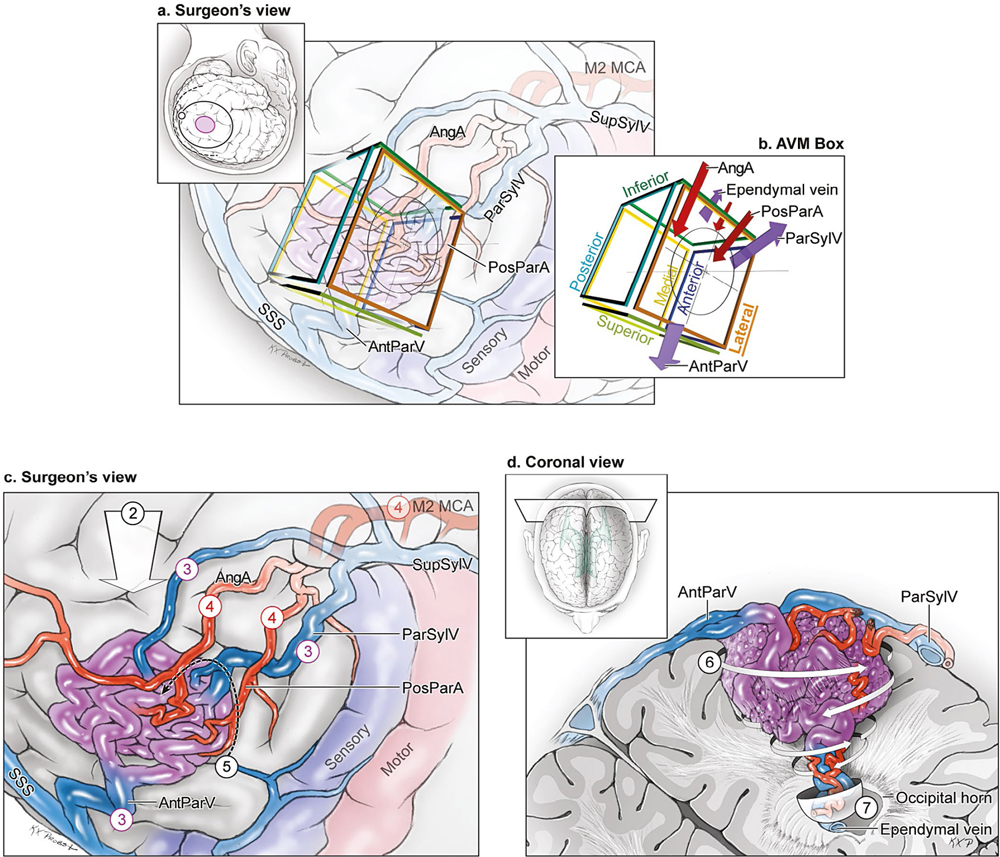
13 Parieto-Occipital Arteriovenous Malformations Divisions between the parietal and occipital lobes are somewhat arbitrary. Although they are divided by the parieto-occipital sulcus on the medial hemisphere, there is no such separating sulcus on the lateral hemisphere. Instead, the extended sylvian line drawn along the long axis of the sylvian fissure divides these two lobes arbitrarily. The parietal and occipital lobes have defined boundaries, but they are anatomically contiguous and continuous. They are considered as a unit in this book because their vascular anatomy is interrelated and arteriovenous malformations (AVMs) in parietal and occipital lobes are managed so similarly. Even combining two lobes, the parieto-occipital unit still has only three anatomic surfaces (lateral, medial, and basal) and lacks the anatomic complexity of a major fissure or convolution (Fig. 13.1). Technically, the parietal lobe has a sylvian surface between the central sulcus and supramarginal gyrus, but it is short and an AVM here would be handled just like a sylvian frontal AVM. The lateral parietal surface is made up of three parts: the postcentral gyrus, which is vertically oriented and parallels the central and postcentral sulci; the superior parietal lobule (SPL), which extends from the superior border of the hemisphere to the horizontally oriented intraparietal sulcus; and the inferior parietal lobule (IPL), the larger of the two lobules that contains the supramarginal and angular gyri. The lateral occipital surface is composed of the superior occipital (SOG) and inferior occipital gyri (IOG), which are divided by the lateral occipital sulcus. The medial parietal surface is made up of the posterior paracentral lobule (medial extension of postcentral gyrus), the posterior cingulate gyrus, and the precuneus (medial extension of SPL). The parieto-occipital sulcus defines the medial boundary between the parietal and occipital lobes. The calcarine fissure extends forward from the occipital pole and joins the parieto-occipital sulcus behind the isthmus of the cingulate gyrus, dividing the medial occipital surface into the cuneus (above) and lingula (below). The basal occipital surface is composed of the lower part of the lingula, the posterior continuation of occipitotemporal gyrus (OTG, or fusiform gyrus), and the medial continuation of the IOG, divided by posterior extensions of the collateral and occipitotemporal sulci. The parieto-occipital lobe is supplied by all three of the major cerebral arteries, unlike the other cerebral lobes that are supplied by only two (Fig. 13.2). Distal middle cerebral artery (MCA) cortical arteries supply the lateral parieto-occipital surfaces and originate from both the superior and inferior MCA trunks of bifurcations, from the middle trunk of MCA trifurcations, or from the dominant trunk in unequal bifurcations. These cortical M4 arteries emerge from the distal sylvian fissure and fan out as central (CenA), anterior parietal (AntParA), posterior parietal (PosParA), angular (AngA), and temporo-occipital arteries (TempOccA). Terminal A5 anterior cerebral artery (ACA) cortical arteries supply the medial parietal lobe as the superior (SupParA) and inferior parietal arteries (InfParA). The lateral parietal arteries from the MCA are named “anterior” and “posterior,” whereas the medial parietal arteries from the ACA are named “superior” and “inferior.” SupParA supplies the precuneus and InfParA supplies the cuneus and precuneus (inferior part). Fig. 13.1 (opposite) Microsurgical anatomy of the parietal and occipital lobes. (a) Lateral parieto-occipital surface (lateral view), with eloquent areas shown in color: motor strip (red), somatosensory strip (blue), visual cortex (green), and language conduction area (angular gyrus, supramarginal gyrus, and underlying arcuate fasciculus, purple). (b) Medial parieto-occipital surface (medial view). (c) Basal parieto-occipital surface (inferior view). (d) Visual system consists of the eyes and retina, optic nerves, optic chiasm, optic tracts, lateral geniculate body or nucleus, optic radiations, and visual cortex, shown in lateral, (e) medial, and (f) inferior views. Note that the optic radiations pass laterally around the temporal horn of lateral ventricle, including Meyer’s loop anteriorly in the temporal lobe, and traverse occipital white matter lateral to the occipital horn. Fig. 13.2 Microsurgical anatomy of parieto-occipital arteries. (a) The lateral parieto-occipital surface is supplied by distal MCA cortical branches from both the superior and inferior trunks of an MCA bifurcation, or the middle trunk of an MCA trifurcation (CenA, AntParA, PosParA, AngA, and TempOccA). Branches from the ACA also extend to the medial part of the lateral parieto-occipital surface, and branches from the PCA extend to the inferior part of the lateral surface. (b) The medial parieto-occipital surface is supplied by terminal ACA branches (ParaCenA, SupParA, and InfParA) and PCA branches (CalcA and ParOccA). (c) The basal occipital surface is supplied by PosTempA, which originates from the P2 PCA as multiple branches (anterior, middle, and posterior) or as a common trunk shown here. The parieto-occipital lobe is drained by cortical veins on the lateral, medial, and basal surfaces (Fig. 13.3). Ascending veins to the superior sagittal sinus (SSS) predominate and include the postcentral (PostCenV), anterior (AntParV) and posterior parietal (PostParV), and occipital veins (OccV), with the largest vein designated as the vein of Trolard. Lateral occipital veins course forward to reach the medial parietal lobe and clear an area of 4 to 5 cm along the distal SSS where no large veins bridge to the sinus; this anatomy is exploited for the posterior interhemispheric approaches. Inferolaterally, there are parietosylvian veins that descend to the sylvian fissure. Occipital veins descend laterally to the transverse sinus (TrvS) and vein of Labbé. The medial parieto-occipital veins drain superficially and deep. Ascending veins to the SSS include the paracentral (ParaCenV), medial parietal (MedParV; anterior and posterior), and posterior calcarine veins (PosCalcV); and descending veins to the vein of Galen (VoG) include the posterior pericallosal vein (PcaV) and anterior CalcV (AntCalcV, a.k.a., internal occipital vein). Occipitobasal veins (OccBasV) drain the basal surface under the occipital pole and course to the tentorial sinus (TentS), posterior TempBasV, or anterolaterally to the TrvS. Fig. 13.3 Microsurgical anatomy of parieto-occipital lobe veins. (a) Veins of the lateral parieto-occipital surface (lateral view). (b) Veins of the medial parieto-occipital surface (medial view). (c) Veins of the basal occipital surface (inferior view). Parieto-occipital AVM subtypes include the lateral parieto-occipital, medial parieto-occipital, paramedian parieto-occipital, and basal occipital. As with frontal AVMs, there is a subtype for each surface and an extra one for paramedian AVMs with sides on both the medial and lateral surfaces that require additional access to two surfaces and three arterial territories. The lateral parieto-occipital AVM is the stereotypical convexity AVM with a cortical base and tapered extension toward the ventricle (Fig. 13.4). It is the second most common subtype overall and accounts for half of all parieto-occipital AVMs and more than twice as many as most other parieto-occipital subtypes. It involves only the lateral surface (involvement of the medial surface would make it a paramedian AVM). Most lateral parieto-occipital AVMs have a free side, although some are deep to the cortical surface without a free side. These AVMs are supplied mainly by MCA cortical arteries: CenA, AntParA, PosParA, AngA, and TempOccA. Input depends on the convexity location, with superior AVMs supplied by AntParA and PosParA and inferior AVMs supplied by AngA and TempOccA. Contributions from ACA and PCA are minimal except with AVMs near the MCA–PCA watershed. Lateral parieto-occipital AVMs drain superficially, ascending to the SSS (PosCenV, AntParV, PostParV, and/or OccV) or descending to the sylvian veins (ParSylV and Sup-SylV). Parietal AVMs are eloquent when located in the post-central gyrus, and occipital AVMs are eloquent when located near the pole in the visual cortex. A perisylvian AVM in the angular and supramarginal gyrus can involve speech conduction tracts in the arcuate fasciculus connecting Wernicke’s and Broca’s areas. Fig. 13.4 The lateral parieto-occipital AVM: (a) lateral and (b) coronal cross-sectional views. This AVM is located on the lateral parieto-occipital surface, supplied by branches from the superior and inferior MCA trunks, and drained by ascending veins to the SSS and/or descending veins to SupSylV. The medial parieto-occipital AVM is based on the medial hemisphere with its base in the posterior interhemispheric fissure without extension to the lateral convexity (Fig. 13.5). It resides anywhere beyond the central sulcus, and may be superficial below the medial corner of the hemisphere or deep near, but not in, the splenium. These AVMs are fed by cortical PCA branches and, to a lesser degree, the ACA, but not the MCA. Parietal AVMs receive contributions from ParaCenA, SupParA, InfParA, and ParOccA (ACA and PCA), whereas occipital AVMs receive contributions from ParOccA and CalcA (just the PCA). Medial parieto-occipital AVMs drain superficially or deep, ascending to the SSS via ParaCenV, MedParV, and posterior CalcV, or descending to the VoG via the posterior pericallosal vein (PcaV) and anterior CalcV. Medial parietal AVMs in the paracentral lobule are eloquent (somatosensory cortex for leg sensation), as are medial occipital AVMs in the cuneus and lingula around the calcarine fissure (visual cortex). A swath of non-eloquent territory lies between these two eloquent areas. Fig. 13.5 The medial parieto-occipital AVM: (a) medial and (b) coronal cross-sectional views. This AVM is located on the medial parieto-occipital surface, supplied by cortical PCA branches (ParOccA and CalcA) and ACA branches (ParaCenA, SupParA, and InfParA), and is drained by superficial veins to the SSS (ParaCenV, MedParV, and PosCalcV) and deep veins to the VoG (PosPcaV and AntCalcV). The paramedian parieto-occipital AVM is a combination of the medial and lateral subtypes residing on both medial and lateral surfaces and centered at their orthogonal intersection at the medial corner of the hemisphere (Fig. 13.6). This AVM has two free surfaces that can expedite resection when exposed properly. Paramedian parieto-occipital AVMs lie at the watershed between the MCA, PCA, and ACA territories, making them the only parieto-occipital subtype and the only cerebral subtype to be fed by all three cerebral arteries. Arterial supply varies with size and location in the parieto-occipital range, with paramedian parietal AVMs having a mix of ACA and PCA supply, and occipital AVMs having mostly PCA supply. Similarly, the more a paramedian AVM extends laterally, the more it will be supplied by the MCA. Venous drainage is predominantly superficial to the SSS. Paramedian AVMs have eloquence when based on the postcentral gyrus/paracentral lobule or the IOG/cuneus. Small AVMs can be resected with good somatosensory and visual outcomes, as can those based in the area between the somatosensory strip and the visual cortex. Fig. 13.6 The paramedian parieto-occipital AVM: (a) medial, (b) coronal cross-sectional, and (c) posterior views (with a section of the superior sagittal sinus [SSS] removed to show the AVM’s medial surface). This AVM is located on both the lateral and medial parieto-occipital surfaces, is supplied by all three cerebral arteries (MCA, PCA, and ACA), and drains superficially to the SSS through lateral and medial parieto-occipital veins. Fig. 13.7 The basal occipital AVM: (a) inferior and (b) coronal cross-sectional views. This AVM is located on the basal occipital surface and is supplied by PosTempA branches from the PCA, with minor contributions from calcarine artery medially (PCA) and temporo-occipital artery laterally (MCA). This AVM drains to basal veins (TempBasV and OccBasV) that collect in the tentorial or transverse sinuses. The basal occipital AVMs are the least common of the parieto-occipital AVMs (around 10%). They are located on the basal undersurface of the occipital lobe along the tentorium anywhere from the falcotentorial junction medially to TrvS laterally (Fig. 13.7). They also vary in their depth from the occipital pole posteriorly to the tentorial incisura anteriorly. The PCA supplies basal AVMs almost exclusively with PosTempA and inferior branches from CalcA. The ACA is uninvolved, but TempOccA from the MCA may supply basal AVMs adjacent to the TrvS. Venous drainage is typically superficial to the posterior TempBasV and OccBasV, which then collect in the TrvS or TentS. The visual pathways, including optic radiations en route to the occipital pole as well as visual cortex, are intimately associated with basal AVMs, and tight dissection planes are needed to spare the visual fields. The lateral parieto-occipital AVM is exposed with a simple convexity craniotomy that does not expose the interhemispheric or infraoccipital planes and therefore does not cross venous sinuses (Fig. 13.8, step 1). The patient is positioned laterally with the degree of head rotation depending on the AVM location: neutral (midline horizontal) for parietal lesions and “nose down” for occipital lesions. A horseshoe skin incision is used. These AVMs are based on the lateral surface, and subarachnoid dissection is limited to opening the overlying arachnoid and surrounding sulci (step 2). This base offers a free side, although some lateral parieto-occipital AVMs are subcortical and are localized by following the arterialized vein. Ascending venous drainage (PosCenV, AntParV, PostParV, and/or OccV) is localized to the AVM’s superior margin (step 3). The arterial supply is superficial and travels from the distal sylvian fissure (CenA, AntParA, PosParA, AngA, and/or TempOccA) (step 4). These arterial feeders are found anteroinferiorly, either on pial surfaces or in sulci along the AVMs margin near the supramarginal and angular gyri (step 5). Parenchymal dissection is parallel, with hot sides located anteriorly and inferiorly and eloquent sides associated with the somatosensory strip, visual cortex, optic radiations, and speech conduction tracts (step 6). Deep dissection may extend conically to an ependymal AVM in the atrium or occipital horn, supplied by choroidal arteries (lPChA) or deep MCA branches and drained by ependymal veins (step 7) (Figs. 13.9, 13.10, 13.11). Fig. 13.8 Resection strategy for lateral parieto-occipital AVMs. (a) Step 1, exposing the AVM with a unilateral parieto-occipital craniotomy (surgeon’s view, with the patient in the lateral position and the head rotated “nose down”; scalp incision (dashed line), craniotomy (solid line), and AVM (purple circle) shown on inset). (b) AVM box showing arterial inputs from MCA branches, venous drainage to both the SSS and the sylvian veins, and proximity to the sensory cortex. Note that the AVM’s cortical surface is depicted with a circle on its base side and that side’s label is underlined. The AVM’s axis is depicted with a line through the box. Arterial and venous anatomy is superimposed on the box with red inflow arrows and blue outflow arrows, respectively. (c) Step 2, dissecting margins in the lateral sulci (broad white arrow); step 3, identifying ascending convexity veins and descending sylvian veins; step 4, locating cortical MCA feeders; and step 5, interrupting the anteroinferior front of arteries near the supramarginal gyrus (dashed black line, surgeon’s view). (d) Step 6, circumdissecting into parieto-occipital parenchyma (encircling arrows); and step 7, mobilizing the AVM (spherical scoop) to expose deep feeding arteries from white matter or ventricle, as well as ependymal draining veins (coronal cross-sectional view).
 Microsurgical Anatomy
Microsurgical Anatomy
Brain
Arteries
Veins
 Four Parieto-Occipital AVM Subtypes
Four Parieto-Occipital AVM Subtypes
The Lateral Parieto-Occipital AVM
The Medial Parieto-Occipital AVM
The Paramedian Parieto-Occipital AVM
The Basal Occipital AVM
 Parieto-Occipital AVM Resection Strategies
Parieto-Occipital AVM Resection Strategies
Lateral Parieto-Occipital AVM Resection
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Neupsy Key
Fastest Neupsy Insight Engine