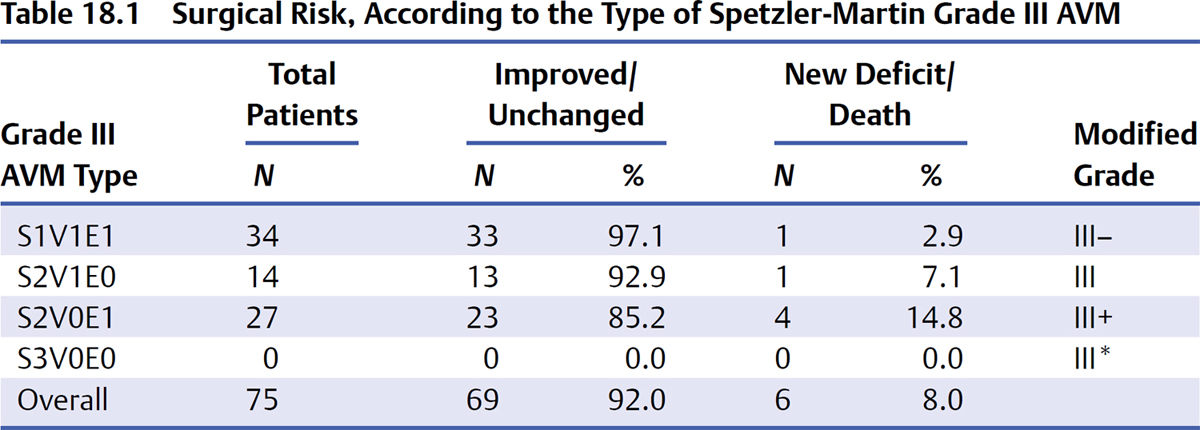
18 Patient Selection Judicious patient selection is essential to avoid surgical complications and poor neurologic outcomes with microsurgical resection of brain arteriovenous malformations (AVMs); it is the secret to success. The wide variety of AVM anatomy, size, location, and clinical presentation makes patient selection for surgery a difficult process. Neurosurgeons have analyzed their surgical experiences to identify factors that determine the risks of surgery in order to assist them in this selection process. Numerous classification schemes have been developed, each with its own emphasis, accuracy, advantages, and disadvantages. Some are complex and others simple, each striving to predict surgical risk and achieve bedside applicability. These classification schemes have value because they transform complex decisions into algorithms. This chapter describes my approach to patient selection. The first major AVM grading scheme, developed by Luessenhop and Gennarelli, in 1977 formulated a grade from I to IV based on the number of feeding arteries, counting the number of tertiary arteries feeding the AVM from a single vascular territory [middle cerebral artery (MCA), anterior cerebral artery (ACA), or posterior cerebral artery (PCA)]. When the AVM was supplied by multiple territories, the grade was determined by the vascular territory with the largest number of feeders. No additional grade was assigned for large AVMs with more than four arteries, as these lesions were deemed inoperable. Surgical results in 49 patients demonstrated that grade I AVMs were associated with low risk, higher grade AVMs were associated with increasing risks, and grade IV AVMs were managed nonoperatively. Luessenhop and Rosa simplified this grading scheme in 1984 by considering only the angiographic size of the AVM, which was easier than counting arterial feeders. The new grades were assigned based on nidus diameter: grade I, < 2 cm; grade II, 2 to 4 cm; grade III, > 4 to 6 cm; and grade IV, > 6 cm. Surgical results in 90 patients demonstrated low morbidity and mortality with grades I and II AVMs, and surgical resection was recommended for these lesions, with minimal consideration of nidus location, patient age, or comorbidities. Conservative management was recommended for patients with highgrade lesions (grades III and IV). Shi and Chen presented an alternative classification scheme in 1986 that considered AVM size, location and depth, arterial supply, and venous drainage. Each of these four aspects was divided into four grades. Specifically, size was graded as < 2.5 cm (grade I), 2.5 to 5 cm (grade II), > 5 to 7.5 cm (grade III), or > 7.5 cm (grade IV). Location and depth were graded as superficial/nonfunctional (grade I), super ficial/functional (grade II), deep (grade III), and deep/vital (grade IV). Arterial supply was graded as single superficial branch of MCA or ACA (grade I), multiple superficial branches of MCA and/or ACA (grade II), PCA branches or deep MCA and/or ACA branches (grade III), and branches of all three cerebral arteries or vertebrobasilar artery (grade IV). Finally, venous drainage was graded as single superficial (grade I), multiple superficial (grade II), deep (grade III), and deep with variceal dilatation (grade IV). The final AVM grade was determined based on the highest of the grades. Excellent results were achieved in patients with low-grade AVMs, and morbidity/mortality increased with high-grade AVMs. This classification scheme demonstrated that complexity will ruin a grading scheme and prevent it from gaining acceptance. In 1986, Spetzler and Martin published what has become the predominant classification scheme for brain AVMs. After considering a range of factors including size, number of feeding arteries, location, operative accessibility, shunt flow, vascular steal, location, and venous drainage, the authors settled on a simplified scheme utilizing only size, eloquence of surrounding brain parenchyma, and venous drainage pattern. Simplicity, applicability at the bedside, and accurate outcome prediction were the authors’ principal objectives. Each factor in the grading scale was scored independently. Size was divided into three categories, with small AVMs, < 3 cm, assigned 1 point; medium AVMs, 3 to 6 cm, assigned 2 points; and large AVMs, > 6 cm, assigned 3 points. Venous drainage was considered superficial if it drained into cortical veins and convexity sinuses and assigned 0 points, or deep if it drained into veins that coursed to the vein of Galen [i.e., internal cerebral vein (ICV), basal vein of Rosenthal (BVR), and precentral cerebellar vein (PreCenCblV)] and assigned 1 point. In the posterior fossa, only veins draining to the straight or transverse sinuses were considered superficial. Arteriovenous malformation eloquence was assessed anatomically based on the presumed function of surrounding brain tissue, with 1 point assigned to lesions located in sensorimotor cortex, language areas, visual cortex, hypothalamus, internal capsule, brainstem, cerebellar peduncles, or deep cerebellar nuclei. Arteriovenous malformations not in these regions were assigned 0 points for eloquence. The final AVM grade was the sum of points across the three domains, with a grade range from I to V. Arteriovenous malformations that are too complex for resection, such as intrinsic brainstem and holohemispheric AVMs, were deemed grade VI. The Spetzler-Martin grading system was initially evaluated in 100 consecutive surgically resected AVMs. Outcomes were categorized as “no deficit,” “minor deficit” (temporary worsening of neurologic function, mild ataxia, or mild increase in brainstem deficit), or “major deficit” (aphasia, hemianopsia, or hemiparesis). There were no major deficits and only one minor deficit in patients with low-grade AVMs (grades I and II). Patients with high-grade AVMs experienced much higher rates of both major (grade IV, 7%; grade V, 12%) and minor deficits (grade IV, 20%; grade V, 19%). Prospective analysis as well as independent analyses by other groups confirmed the accuracy of the grading system to predict operative morbidity and mortality. This grading system has been widely accepted by neurosurgeons and other clinicians for its simplicity and practicality, quickly providing estimates of surgical risk. Furthermore, its easy applicability has made the grading system an integral part of the description and language of brain AVMs. Experience with this grading has demonstrated three distinct groups of patients. Low-grade AVMs (grades I and II) have low morbidity rates associated with their resection and are frequently treated surgically. High-grade AVMs (grades IV and V) have high morbidity rates associated with their resection and are frequently managed conservatively. Grade III AVMs have intermediate morbidity rates associated with their surgical resection, and treatment recommendations require an individualized approach with multimodality treatment. One deficiency of the Spetzler-Martin grading system is its handling of grade III AVMs. A 2-cm thalamic AVM with deep drainage has the same score as a 7-cm right frontal pole AVM with superficial drainage, yet these two very different lesions have the same grade. Grade III AVMs are the most heterogeneous of the five grades, with four different combinations of size, venous drainage, and eloquence, and one third of all combinations of these elements of the grading scale. In addition, these AVMs are technically challenging, at the limit of what many neurosurgeons are willing to accept in terms of technical difficulty and potential morbidity. The Spetzler-Martin grading system lumps these diverse lesions together and fails to provide the clarity in management that it does for lowand high-grade AVMs. In an analysis of a consecutive series of 76 of my grade III AVMs, neurologic outcomes varied according to the subtype of grade III AVM (Table 18.1). Small grade III AVMs, with 1 point assigned for size, deep venous drainage, and eloquence (S1V1E1), were the most common and had the lowest surgical risk (3% morbidity). In contrast, medium-sized/eloquent grade III AVMs (S2V0E1) had the highest surgical risk (15% morbidity). Medium-sized/deep grade III AVMs (S2V1E0) had an intermediate surgical risk (7%). Large grades III AVMs (S3V0E0) are exceedingly rare, with none in this surgical experience. Based on these data, grade III AVMs should not be considered a homogeneous group with equivalent risks for all subtypes, as the Spetzler-Martin scheme suggests. Instead, grade III AVMs should be analyzed according to the four subtypes defined by the Spetzler-Martin scheme. A modification to the Spetzler-Martin scheme emphasizes these differences. Small grade III AVMs are designated grade III– because their surgical risk was less than the average grade III lesion, more like a grade II lesion. Medium/eloquent grade III AVMs are designated grade III+ because their surgical risk was more than the average grade III lesion, more like a grade IV lesion. Medium/deep grade III AVMs are designated plain grade III because their surgical risk was the same as the average grade III lesion. Large grade III AVMs are designated grade III* because they are lesions fabricated by the grading system with an incidence so low that their surgical risk is unclear. Large, superficial AVMs in non-eloquent brain can only occur in the frontal or temporal poles; large AVMs in other locations are likely to have a deep draining vein or abut eloquent brain tissue.
 Pre-Spetzler-Martin Grading Systems
Pre-Spetzler-Martin Grading Systems
 Spetzler-Martin Grading System
Spetzler-Martin Grading System
 A Modification to the Spetzler-Martin Grading System
A Modification to the Spetzler-Martin Grading System
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree