Pedicle Navigation in Spondylothesis
C. Bolger
M. Bourlion
Pedicle screw fixation has been widely used for stabilization of the spine for conditions such as trauma, deformity, tumors, and the degenerative spine since its introduction in the late 1950s (1,2,3,4,5,6). One of the main problems facing the surgeon during pedicle screw placement is the inability to visualize the actual pedicle during both preparation of the pedicle and the actual screw placement, a situation that makes perforation of the vertebral wall a surgical risk. Numerous published studies have looked at the rate of both cortical breaches and screw misplacement, concluding that between 15% and 55% of screws breach some aspect of the pedicle. Complications of such breaches include but are not limited to dysesthesia, paraparesis, or paraplegia (7,8,9,10,11,12,13).
To achieve optimal placement of pedicle screws and to avoid the complications described above, surgeons have increasingly used computer-assisted and spinal-monitoring devices. Such techniques include, but are not limited to, mechanical probing, electromyography (EMG), somatosensory evoked potentials (SEEP), and spinal cord monitoring, along with image guidance. However, these methods all have their drawbacks. Probing is an inconsistent method, the results of which depend on the operator. The use of intraoperative EMG and monitoring is complex and requires the participation of trained personnel for the duration of the surgery (14,15,16).
Postoperative solutions for detection of accurate pedicle screw placement include computed tomography (CT), fluoroscopy, and roentgenography, as well as feedback from the patient. However, these are carried out after the screw placement and are therefore too late to avoid neurologic deficit.
SURGICAL NAVIGATION
Surgical navigation techniques offer many benefits to the surgeon for the accurate placement of pedicle screws. Preoperative CT scanning loaded into the system allows the surgeon to plan preoperatively for the best trajectory for optimal placement of the screws. The option to measure all dimensions of the pedicle, which is normally not visible to the surgeon, avoids the risk of breaches as a direct result of the actual screw. For more complex and deformed spines, the three-dimensional (3D) image generated by the computer is beneficial in defining complex and disrupted anatomy, allowing the surgeon to operate in confidence and increasing the accuracy of the placement of the pedicle screws (11,17,18,19,20,21).
However, surgical navigation also has its drawbacks insofar as it is an expensive system and requires preoperative CT scanning and time for the surgeon to load the scanning and plan the exams preoperatively. To gain the best advantage from the system there is a rather long learning curve for the user, which can lead to the risk of overreliance on technology for completion of the surgery. Moreover, when using image guidance for
multiple-level spinal fusions, the actual registration tends to lose its accuracy over the multilevel procedure and may require the surgeon to reregister the system to another anatomical landmark in the spine, thus lengthening the actual surgical procedure.
multiple-level spinal fusions, the actual registration tends to lose its accuracy over the multilevel procedure and may require the surgeon to reregister the system to another anatomical landmark in the spine, thus lengthening the actual surgical procedure.
IMAGE GUIDANCE IN SPONDYLOLISTHESIS
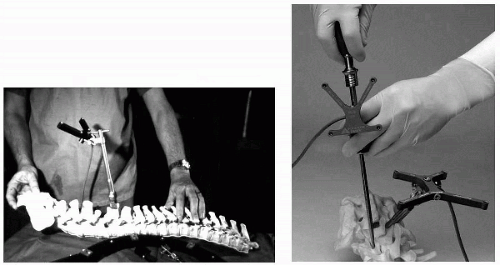
In order to use image guidance, the spine needs to be both orientated and registered to the computer-generated 3D model that has been obtained from preoperative CT. A reference arc is clasped onto one of the exposed spinous process, and this is registered onto the 3D model (Fig 28.1). The remainder of the registration is generated around this point.
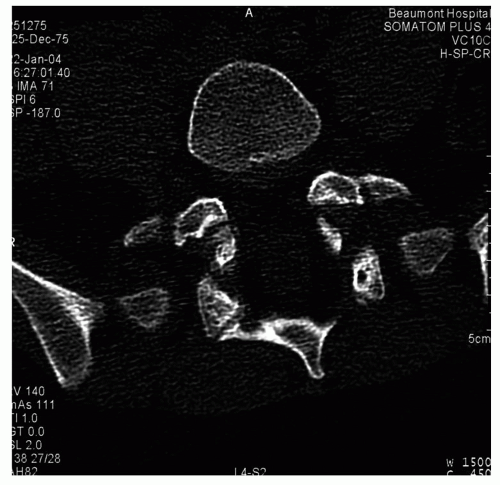
However, in spondylolisthesis, a stress fracture of the pars interarticularis (Fig. 28.2) causes detachment of the stabilizing elements posterior to the motion segments. This
detachment causes a biomechanical imbalance resulting in a shearing and eventual failure of the disc annulus, which results in displacement of the vertebral body. Therefore, because there is no stable anatomy for placement of the reference frame for image guidance, this method of navigational surgery is not suitable for accurate navigation in patients with spondylolisthesis. Hence, there is a need for an efficient and cost-effective device that will assist the surgeon to navigate the pedicle in relative safety that is adaptable to be used in most spinal conditions, including spondylolisthesis.
detachment causes a biomechanical imbalance resulting in a shearing and eventual failure of the disc annulus, which results in displacement of the vertebral body. Therefore, because there is no stable anatomy for placement of the reference frame for image guidance, this method of navigational surgery is not suitable for accurate navigation in patients with spondylolisthesis. Hence, there is a need for an efficient and cost-effective device that will assist the surgeon to navigate the pedicle in relative safety that is adaptable to be used in most spinal conditions, including spondylolisthesis.
ELECTRICAL IMPEDANCE IN SPINE SURGERY
In biologic tissues, electrical conductivity depends on tissue structure and blood content. The basic idea is that by assessing electrical conductivity, one can distinguish cortical bone from cancellous bone and both from soft tissue. Electrical impedance measurements have been used previously in spinal surgery. Although some authors have suggested that impedance is not effective for detecting screw fractures (22,23), this conclusion was biased by several technical artifacts, as described below.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree