Fig. 1
The image on the left depicts the Penumbra Coil 400 System and its 0.020″ diameter loops. The image on the right is of a conventional coil with 0.010″ coil loops (Image reprinted with permission from Penumbra Inc.)
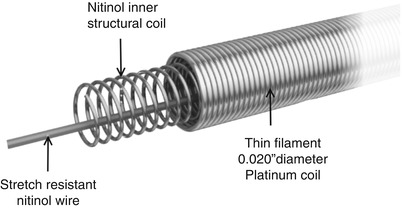
Fig. 2
The design of the Penumbra Coil 400 System is composed of three metal layers (Image reprinted with permission from Penumbra Inc.)
Methods
Approval was obtained from the Institutional Review Board of our university for this study. We retrospectively collected data from consecutive patients with unruptured intracranial aneurysms with a wide-neck (≥4-mm neck or dome:neck ratio <2:1) treated by the senior author (EMD) between October 2008 and December 2012. Patients were divided into two groups based on the choice of endovascular coils: (1) PC-400 and (2) conventional coils (Cashmere, Micrusphere, DeltaWind, and Ultipaq: Codman & Shurtleff, Inc., Raynham MA, USA; Hydrogel, Cosmos, Complex, and HyperSoft: MicroVention, Inc., Tustin CA, USA). All patients had planned adjunctive stenting with either an Enterprise (Codman & Shurtleff, Inc., Raynham MA, USA) or Neuroform (Stryker Corporation, Kalamazoo MI, USA) intracranial stent. Only unruptured aneurysms were considered in the present analysis because adjunctive stent placement is a rarity after aneurysm subarachnoid hemorrhage where antiplatelet therapy is a relative contraindication.
In our series, the first framing coil was placed into the aneurysm sac and its ability to respect the ostium of the neck was tested to confirm that it would not herniate into the parent vessel before detachment. In the PC-400 group, the stiffer standard coils were typically inserted first to frame the aneurysm so that they would maintain their position within the sac better and minimize the chance of coil loop herniation into the parent vessel. Subsequently, the coils were rapidly downsized and soft or extra-soft PC-400 coils were used to finish the packing to avoid pushing the previous coils out of the aneurysm sac. The initial PC-400 framing coil typically was chosen based on the maximum aneurysm sac diameter, downsizing to the closest loop size that matched the dome because of their more robust nature. Similar techniques were used with the conventional coils, except that the first framing coil was upsized to the closest loop length to secure them against the sac wall; our initial experience demonstrated that when the PC-400 system was chosen in the same manner, the coils were too large and would push out of the aneurysm. In both cases, if the first framing coil herniated into the parent vessel, it was removed and the process was repeated with a larger-sized framing coil and when stent assistance was required, a Neuroform or Enterprise stent was placed across the neck to act as a scaffold for the coil mass according to our standard treatment preferences.
The goal of every coiling was total occlusion of the aneurysm, aneurysm embolization grade (AEG) = A, with stent assistance only when framing coils would not respect the aneurysm neck. The AEG system was used because of its unique angiographic filling characteristics, which have been demonstrated to have predictive value for determining aneurysm sac thrombosis [2, 11]. The filling characteristics include persistent contrast in the aneurysm neck (AEG = B) or dome (AEG = C) in the capillary or venous phase of the angiogram, and emptying of contrast from the aneurysm neck (AEG = D) or dome (AEG = E) during the arterial phase in sync with the parent artery.
Coil insertion was stopped when total occlusion of the aneurysm was achieved or the microcatheter dislodged from the aneurysm neck and could not be accessed again, thus preventing additional coils from being inserted into the sac. An AEG was assigned by the interventionalist based on the flow of contrast material into the aneurysm neck and dome immediately after embolization. The packing density was calculated using AngioCalc (www.angiocalc.com) for all treated aneurysms. The length of coils and aneurysm volume were also used to calculate the total coil length per unit aneurysm volume (cm/mm3). Short-term radiographic occlusion was noted at follow-up imaging typically scheduled 6 months postprocedure. The long-term occlusion durability of the PC-400 is being examined on a larger scale in the Aneurysm Coiling Efficiency Clinical Trial (NCT01465841).
Data were analyzed using SPSS Version 17 (IBM Corporation, Armonk NY, USA). Nominal variables were compared between the PC-400 and conventional coil groups using Fisher’s Exact test. Continuous variables were compared between groups using independent samples t-tests. Two-sided probability values less than .05 were considered statistically significant for all analyses.
Results
Thirty-eight patients (59 ± 14 years) were identified who underwent coil embolization for wide-necked intracranial aneurysms. Fifteen patients were treated with the PC-400 system and the remaining 23 with conventional coils (Table 1). There were no significant differences in neck size or the maximum aneurysm dimension between groups (P = .760 and P = .425, respectively).
Table 1
Elective wide-necked intracranial aneurysm patient population characteristics and treatment details
Penumbra Coil 400 System (N = 15) | Conventional coils (N = 23) | P value | |
|---|---|---|---|
Age, years; mean (SD) | 58 (14) | 59 (14) | .799 |
Aneurysm Embolization Grade (AEG) | |||
A; n (%) | 6 (40 %) | 9 (39 %) | .269 |
B; n (%) | 3 (20 %) | 9 (39 %) | |
C; n (%) | 4 (27 %) | 5 (22 %) | |
D; n (%) | 2 (13 %) | 0 (0 %) | |
E; n (%) | 0 (0 %) | 0 (0 %) | |
Stent assistance; n (%) | 6 (40 %) | 17 (74 %) | .049 |
Neck size, mm; mean (SD) | 5.2 (1.8) | 5.7 (1.5) | .425 |
Maximum aneurysm dimension, mm; mean (SD) | 10.5 (4.2) | 10.1 (3.5) | .760 |
Coil length, cm; mean (SD) | 47 (31) | 137 (117) | .002 |
Coil length per aneurysm volume (cm/mm3); mean (SD)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| |||


