As with many other areas of surgery, the principles for operative management of peripheral nerve problems have evolved from the published experience of anecdotal data. However, with two of the most common clinical problems in peripheral nerve surgery, CTS and UNE, data exist that provide a basis for evidence-based practice. In this chapter, we examine the evidence available to guide the diagnosis, surgical indications, and choice of surgical technique for these two common peripheral nerve problems. Carpal tunnel syndrome (CTS) is caused by entrapment of the median nerve just distal to the wrist. Thickening of the transverse carpal ligament and hypertrophy of the synovium leads to a decrease in space available to the median nerve in the carpal tunnel. CTS is most often idiopathic but also may be brought on by pregnancy and disease states such as, acromegaly, amyloid, trauma, and hypothyroidism. In the early states, patients typically report nocturnal complaints of numbness and tingling. Later, complaints of ongoing finger numbness and hand weakness evolve. Ulnar nerve entrapment at the elbow (UNE) is the second most common entrapment neuropathy after CTS. The condylar groove posterior to the medial epicondyle creates the cubital tunnel. The floor of the tunnel is the medial ligament of the elbow, and the roof is the aponeurosis of the two heads of the flexor carpi ulnaris. During repetitive motion of the elbow, the cubital tunnel repeatedly expands and contracts in volume. In addition, elbow flexion stretches the ulnar nerve across the elbow. Over time, this strain on the ulnar nerve can lead to signs and symptoms of entrapment including pain, paresthesias, and muscle atrophy in the ulnar distribution. Provocation of symptoms during flexion is a typical feature. We could not identify any studies of inter- and intraobserver reliability of tests for evaluating patients for the presence or severity of either carpal tunnel syndrome or ulnar nerve entrapment at the elbow. We briefly discuss a few selected studies that discuss common methods of patient assessment in these conditions.1–4 Recent investigations have examined the usefulness of sensory, provocative, and electrophysiologic testing as well as their correlation with one another. A survey of industrial workers identified 449 workers out of a population of 824 with at least one positive finding of CTS (sensory, provocative, or electrophysiology).1 Of these, only 23 (5%) had positive findings in all three categories. Two studies reviewed the usefulness of provocative testing in patients who met electrophysiological criteria for CTS. Prignac and Henry2 concluded from their data that the Phalen’s test (wrist flexion to exacerbate pain and paresthesias), but not the Tinel sign correlated with severity of disease. Gellman et al3 concluded that the Phalen’s test was most sensitive while the Tinel sign, although less sensitive, was more specific. Both studies concluded that manual compression of the carpal tunnel and other provocative tests were not useful. The conclusions that reached from these studies are limited in that they depend upon electrodiagnostic testing as the standard for diagnosis and for assessing severity of disease (Table 8-1).  8
8 
Peripheral Nerve Surgery
Jacob P. Schwarz, James N. Campbell
Patient Assessment
Carpal Tunnel Syndrome
| Reference | Purpose | Design | Diagnostic | Subjects | Conclusion |
|---|---|---|---|---|---|
| Homan et al, 19991 | Compare history, physical exam, and NCS in CTS | Prevalence study | History, PE, and NCS | Industrial workers | 449 of 824 with at least one finding. All three criteria met in 23. Poor overlap between screening procedures. |
| Priganc and Henry, 20032 | Examine five diagnostic tests for CTS | Retrospective review of diagnostic findings | Phalen, Tinel, manual CT compression, Katz-Sirrat hand diagram, CT outcomes assessment tool | 66 electrodiagnostically tested patients in occupational therapy practice | Only Phalen correlated with severity of electrodiagnostic tests. |
| Gellman et al, 19863 | Compare provocative testing to electrodiagnostic testing | Provocative testing of patients with CTS and control patients | NCS, wrist flexion (Phalen’s), tourniquet, median nerve percussion (Tinel’s) | 42 patients (67 hands) with findings of CTS on NCS compared with 50 control patients | Using NCS as the gold standard, Phalen’s was found to be most sensitive (71%), Tinel’s most specific (94%). |
| Bindra et al,19974 | Evaluate use of routine wrist radiography in diagnosing and managing CTS | Retrospective review of findings | Wrist radiographs, NCS, PE | 300 consecutive patients (447 wrists) meeting authors’ criteria for CTS from clinical and electrodiagnostic criteria | Only two of 447 radiographs were of therapeutic significance. |
Abbreviations: CTS, carpal tunnel syndrome; NCS, nerve conduction studies; PE, physical examination.
There has been some exploration of the diagnostic utility of imaging studies. A retrospective review of ultrasound and magnetic resonance imaging (MRI) diagnostics revealed that only two of 447 investigations yielded findings that altered management and that $5,869 to $20,115 was spent for each finding of median nerve entrapment considered severe enough to warrant intervention. The authors concluded that imaging of the wrist is not useful in the evaluation of CTS.4
Ulnar Nerve Entrapment at the Elbow
One study with controls was identified by our search. That study evaluated morphological changes in the ulnar nerve in UNE with high-resolution ultrasonography. The results show that among patients with clinical features of UNE, the mean area of the ulnar nerve at the epicondyle was significantly larger than either the unaffected contralateral nerve or the nerve measured from controls (p < 0.001). The authors conclude that these results support the use of ultrasonography in screening and follow-up of patients with UNE.5
Establishing the Diagnosis
Limitations of Testing
Several studies address the issue of how to diagnose CTS and UNE. These studies all share a common limitation; namely, how does one establish the validity of a test when there is no gold standard? In some studies, electrodiagnostic tests are considered the gold standard. In others, electrodiagnostic testing is compared with the gold standard of physical examination and clinical history. There is no established gold standard and thus, it is inevitable that one study will use as its gold standard a modality that is the experimental modality in another study. These circular comparisons confound the power of any conclusions they generate. Careful attention must be paid to the “positive” findings that are being compared. Investigators may conclude, for instance, that physical examination is as sensitive as nerve conduction studies. However, this conclusion is obviously dependent on what is chosen as the criterion for conduction delay and details of the physical exam. Errors in diagnosis are an inevitable part of testing. The test criteria will determine the proportion of time that a particular condition is overdiagnosed or underdiagnosed.
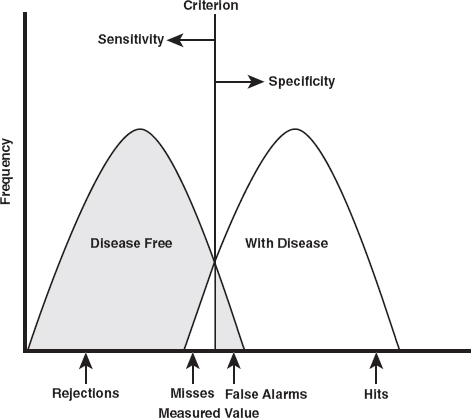
Signal detection theory provides an easy conceptual model with which to evaluate diagnostic criteria. For a given test, the observed measurements of a population will tend to follow a gaussian distribution about a mean value (Fig. 8-1). As an example, let us consider one of the common tests used to diagnose CTS and UNE—latency measurements. In this test, the time it takes for the compound action potential to traverse a putative entrapment point is measured. In our example, participants without a nerve entrapment comprise a distribution of normal values. Patients with nerve entrapment makeup a second distribution, shifted to the right. The degree to which these two distributions overlap determines the power of the test to identify patients who have the disease (“hits”), and those who do not (“correct rejections”). The latency values shared by both distributions and the value chosen to be the test criterion (see the vertical line, Fig. 8-1) define the rate of “false alarms” and “misses.” As is illustrated, shifting the criterion to the left enhances the sensitivity of the test (decreases misses), but at the same time decreases the specificity (increases the false alarm rate). Likewise, as the criterion is shifted to the right specificity (fewer false alarms) increases at the expense of sensitivity (greater misses).
The American Association of Electrodiagnostic Measurement (AAEM) has considered how electrodiagnostic studies should be used to diagnose CTS and UNE. In their review of the existing literature, they found that, although criteria vary, electrodiagnostic testing is useful for comparison if data are (1) obtained prospectively, (2) the electrodiagnostic test method is described in enough detail to be easily reproducible, (3) values obtained from patients are compared with a reference population of controls, and (4) the criterion for abnormal findings is clearly stated and supported by statistically computed terms, range, mean, ± 2 standard deviations from data derived from the reference population.
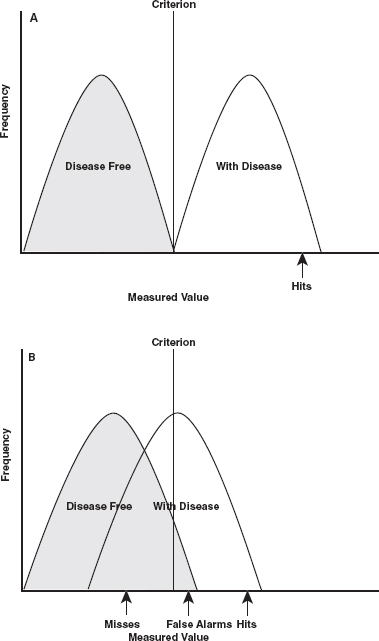
The AAEM recommendations serve the important purpose of providing a standard for comparison within the discipline of electrodiagnostic testing. It is important to consider, however, that the ideal criterion depends on the consequences of the selection, and the risks associated with the error. The incidence of false alarms and misses are related in reciprocal fashion. While using a reference population to establish the test criterion at 2 standard deviations from the mean guarantees a relatively high specificity (around 95%), the same criterion becomes problematic from a sensitivity perspective if there is a great deal of overlap between the distribution of test values for those with and those without the disease (see Fig. 8-2B). If the two distributions do not overlap (Fig. 8-2A) then the better criterion might be 3 or even 4 standard deviations from the mean of the population without disease. To support fully the usefulness of a given test for a given population, studies that examine the test should ideally identify the criterion used, the population that generated it, and the relationship between the test value distributions of those with disease and the disease-free population. This analysis is predicated on the disease being a dichotomous variable (you either have it or you do not). In actuality however, CTS and UNE more likely are “diseases” on a continuum. This obviously further complicates analysis of diagnostic criteria (as well as outcome data).
Carpal Tunnel Syndrome
The diagnosis of CTS may be based on patient history, physical examination, imaging studies, and electrophysiological testing. A literature search with the term carpal tunnel diagnosis yielded 336 responses. As noted above, diagnostic tests must be evaluated as compared with a gold standard for the diagnosis. This does not exist for CTS. Patients often fulfill electrodiagnostic criteria for CTS, for example, and have no symptoms, whereas other patients have symptoms that respond well to carpal tunnel surgery but fail to have positive electrodiagnostic tests.
A systematic review of the literature by Jordan et al 6 uncovered only six retrospective case studies concerning the utility of electrodiagnostics in CTS (all class III evidence). These studies compared outcomes of surgery in patients with clinical signs of CTS and electrodiagnostic results. The authors found no correlation between the outcome of electrodiagnostic studies and patient satisfaction or functional recovery after surgery. An earlier meta-analysis with wider inclusion criteria concluded that, when clinical criteria and physical exam findings are used as the gold standard for diagnosis, median sensory and motor nerve conduction studies detect CTS reliably, reproducibly, and with high sensitivity (70–85%) and specificity (98–100%).7 Although an earlier study found positive tests to be associated with a greater likelihood of subsequent surgery,8 others claim that there is no correlation with electrodiagnostic testing and improved final symptomatic outcome.9
Electrodiagnostic and provocative testing are routinely used in the diagnosis of CTS, but there is no compelling evidence to support one gold standard diagnostic test for CTS.
Ulnar Nerve Entrapment at the Elbow
A search of the National Library of Medicine’s online database, PubMed, regarding the diagnosis of UNE yielded 162 references. These citations report the experience with electrophysiologic testing, provocative maneuvers from physical examination, and MRI and ultrasound investigations of the cubital tunnel. In the absence of an agreed gold standard for the diagnosis, none met the criteria for level I evidence. We have selected studies evaluating patients prospectively (Table 8-2).
As with CTS, there are patients who meet electrophysiological criteria for UNE, yet have no symptoms. Conversely, some patients who have symptoms that respond to ulnar nerve surgery have negative electrophysiological studies. As would be expected, slowing of conduction across the likely entrapment site is the earliest electrophysiological change that can be identified. One of the prospective evaluations including normal controls evaluated the difference in compound nerve action potential latencies recorded from median and ulnar nerves.10 The magnitude of slowing of the ulnar nerve compound action potentials (CNAPs) compared with those from the median nerve was termed the Dlat index. These action potentials were elicited by stimulation at the wrist and recorded 10 cm above the elbow. The authors found a mean Dlat index of 0.72 ms (SD = 0.3 ms) among 60 healthy control patients and Dlat indices of at least 1.47 ms in nine of 10 patients with clinical features of ulnar neuropathy (median 2.07 ms). To verify specificity of the test, 24 patients with other disorders unrelated to the ulnar nerve were also examined. This group was indistinguishable from the control group. The authors conclude that comparing median and ulnar CNAPs in this fashion is feasible and provides sensitive and specific results for ulnar neuropathy.
| Reference | Purpose | Design | Diagnostic | Subjects | Conclusion |
|---|---|---|---|---|---|
| Odusote et al, 197911 | Electrophysiological quantification of UNE | Prospective evaluation of 492 ulnar nerves in 237 patients with UNE and 283 patients without clinical UNE | Electrophysiologic measurements, physical exam | 492 ulnar nerves studied in 237 patients with UNE and 233 controls | 71.5% demonstrated relation of physical exam and electrodiagnostics. The 28.5% that did not correlate all had no objective abnormal physical signs or only mild sensory deficit. |
| Novak et al, 199412 | To evaluate the utility of provocative testing in the diagnosis of UNE | Prospective | Tinel’s sign, elbow flexion (30 second), and pressure provocation (30 second) | 44 with clinical findings of UNE; 33 controls | Most sensitive test was the combination of pressure and elbow flexion (0.91) followed by Tinel’s (0.70), pressure alone (0.55), and elbow flexion (0.32). |
| Merlevede et al, 200010 | To identify a new diagnostic approach to UNE | Evaluation of electrodiag-nostic studies in 60 normal controls, 24 non-UNE neurological patients, and 10 UNE patients | Differences in CNAPs of ulnar and median nerves were used to identify UNE. | 60 normal controls were were compared with 10 patients with UNE identified by PE and NCS. | Electrodiagnostic measures were reliable when identifying UNE. |
| Britz et al, 199613 | To evaluate the correlation of MRI with PE, NCS, and OR findings | Prospective study | Physical examination, PNCS, OR observations, and MRI | 27 symptomatic patients and 10 asymptomatic control patients | Of the four evaluations, only MRI findings were both sensitive and specific in diagnosing UNE as defined by the other criteria. |
Abbreviations: CNAP, compound nerve action potential; MRI, magnetic resonance imaging; NCS, nerve conduction studies; OR, operating room; PE, physical examination; UNE, ulnar nerve entrapment.
The second prospective evaluation measured terminal motor and sensory latencies as well as motor and sensory conduction velocities, and sensory action potential amplitudes.11 Comparing 237 patients with varying degrees of UNE as stratified by electrodiagnostic test results to 233 controls, the authors of this study concluded that these diagnostic studies could be relied upon to follow objectively the improvement or deterioration of the clinical condition with the passage of time.
The literature regarding provocative testing for UNE includes prospective evaluation including normal controls.12 This study evaluated the usefulness of Tinel’s sign, elbow flexion, pressure provocation, and combined elbow flexion–pressure provocation in 44 patients with electrodiagnostically proven UNE and 33 control subjects. The authors found that the maneuvers did not provoke paresthesias, pain, or weakness among control subjects but had the following sensitivities among those patients with electrodiagnostic findings of UNE: Tinel sign 70%, elbow flexion 32%, pressure provocation 55%, and combined flexion pressure 91%. The authors conclude that the combined elbow flexion and pressure provocation test are the most useful in the diagnosis of UNE.
The use of ultrasonography and MRI to evaluate UNE has been reported. For instance, citing the absence of a clear gold standard for the diagnosis of UNE, one investigation evaluated MRI, clinical, electrodiagnostic, and intraoperative findings. Each modality was evaluated for its ability to predict the presence or absence of disease as measured by the other three modalities. The MRI scan was interpreted in blinded fashion. Magnetic resonance imaging was both sensitive (97%) and specific (normal study in 10 control subjects), in diagnosing ulnar nerve entrapment at the elbow as defined by the other criteria.13
As is the case with carpal tunnel syndrome, the lack of an agreed gold standard for diagnosis eliminates the possibility of identifying class I evidence regarding the diagnosis of the condition.
Determination of Prognosis
Natural History Studies
CARPAL TUNNEL SYNDROME
A PubMed search of natural history, carpal tunnel syndrome yielded 16 entries. Only one report commented specifically on untreated patients without other comorbidities. In that study, 12 patients (with 20 affected hands) who had clinical and electrodiagnostic findings consistent with CTS and who refused surgery, medication, and bracing were followed for 4 to 9 years. In all cases, electrodiagnostic testing was performed at the beginning and end of the evaluation period. Clinical symptoms and electrodiagnostic findings, such as nerve conduction velocities, improved in seven patients (eight hands). Two hands deteriorated, and 10 were unchanged.14 It is possible that patients who refuse surgery may have more tolerable and less-pervasive symptoms. It is also possible that deterioration of function is not an inevitable outcome of CTS and that some patients may even demonstrate spontaneous improvement. The small sample size that also limits the ability to evaluate extraneous prognostic variables led to a classification of this study as level III.
ULNAR NERVE ENTRAPMENT AT THE ELBOW
Only one study was identified that specifically investigated the outcomes for patients who receive no therapy. In this study, patients diagnosed with UNE using clinical and electrodiagnostic criteria refused therapy. The study enrolled 37 patients prospectively but added measurements that were collected at follow-up and were therefore retrospective. Of the 37 enrollees, 24 who did not receive surgery participated to the 1-year follow up end point. At one-year follow-up, 10 of the patients reported no significant pain or difficulty with motor function in the distribution of the ulnar nerve. The remaining 14 patients all complained of at least one symptom. Eleven of the patients received complete neurophysiologic assessment at the 1-year time point. Of these, seven demonstrated improvements and six demonstrated absence of any neurophysiologic abnormality. Four patients were unchanged. Two of the four patients without electrodiagnostic improvement nonetheless demonstrated clinical resolution of their symptoms.15 Because of small sample size and incomplete, retrospective follow-up this would also be classified as level III data.
Evaluation of Intervention
Prevention
CARPAL TUNNEL SYNDROME
Repetitive stress is thought by many to play an important role in the genesis of CTS. Extensive computer keyboard use is one factor that is cited. However, one study indicated that the frequency of CTS is similar among computer users and the general population.16 Review of the PubMed citations regarding prevention of CTS reveals more than 200 citations. Of these, very few concentrate on studies of preventive measures (Table 8-3).
Two studies have evaluated the effectiveness of splints or gel-padded gloves to change the pressures measured in the carpal tunnel or the results of nerve conduction latency studies when used by healthy volunteers.17,18 Measurements of carpal tunnel pressure and median nerve conduction velocities from healthy volunteers were compared with and without the splints or gel-padded gloves. Neither intervention was found to modify the pressure in the carpal tunnel or the results from nerve conduction studies during repetitive motion.
| Reference | Purpose | Design | Diagnostic | Subjects | Conclusion |
|---|---|---|---|---|---|
| Deltombe et al, 200119 | To evaluate the protective potential of gel-padded gloves | Randomized crossover trial. Induce NCS changes using external pressure. Evaluated effect of gel-padded gloves | NCS | 6 healthy adults | Gel-padded gloves do not have a protective effect on electrodiagnostic features of CTS induced by compression. |
| Rempel et al, 199418 | To evaluate effect of splints on carpal tunnel pressures | Measurement of mechanical pressures with and without splints | Catheter inserted in carpal tunnel measures pressure. | 19 healthy volunteers | Wrist splint limits range of motion but has no significant effect on carpal tunnel pressure. |
| McKenzie et al, 198519 | To measure effect of OSHA-approved safety measures on incidence of CTS | Incidence study | Cases identified by reports to OSHA | Manufacturing facility with 6600 employees | Before interventions, there were 2.2 cases per 200,000 work hours and 1001 lost work days. After intervention, there were 0.53 cases per 200,000 work hours and 129 lost work days. |
| Lincoln et al, 200021 | To analyze of studies reporting an effect of workplace interventions. | Meta-analysis | Identified 24 studies with at least one tested intervention | No study conclusively demonstrated prevention of CTS. Further randomized, controlled trials with long-term outcome measures are needed. |
Abbreviations: CTS, carpal tunnel syndrome; NCS, nerve conduction studies; OSHA, Occupational Safety and Health Administration.
Many recommendations are made to improve the ergonomics of the workplace but these recommendations are not tested against control groups. Rather, the incidence of CTS before and after the implementation of these changes is compared. One report determined that reducing exposure to repetitive trauma, as well as other improvements, led to a reduction in the incidence of CTS (defined as symptomatic hands requiring treatment) from 2.2 to 0.53 per 200,000 work hours.19 A similar, but more recent, study with similar criteria reported similar improvement after Occupational Safety and Health Administration (OSHA) visits targeted at facilities with high rates of CTS and tendonitis among their workers.20 In the state of New Hampshire such OSHA visits and implementation of ergonomic targets led to a 10-fold reduction in CTS at inspected sites (from 38/10,000 to 3.8/10,000). Sites that had not been targeted by OSHA saw a drop from 6.6/10,000 to 3.4/10,000. The effects of these visits and targeting appear to have an effect on higher risk environments that have drawn the attention of OSHA. Low-risk environments have also shown a reduction of CTS incidence without specific oversight from OSHA. A meta-analysis of recent publications regarding interventions for the primary prevention of work-related CTS evaluated 24 studies of workplace ergonomic improvements and worker education.21 The analysis revealed that several engineering improvements modified the risk factors associated with CTS, but disease incidence was either not measured or not affected. The study concluded that these measures currently command sufficient resources to warrant a large, controlled trial to justify their expense.
ULNAR NERVE ENTRAPMENT AT THE ELBOW
A search for prevention of perioperative neuropathy did not uncover any randomized, controlled trials or prospective studies. The perioperative literature includes one large retrospective study of 1,129,692 consecutive surgery patients at the Mayo Clinic.22 This review reports that 414 patients experienced persistent ulnar neuropathy with onset of symptoms in the immediate postoperative period. It identifies the risk factors of male gender and either very thin or obese body habitus. The authors conclude that most perioperative ulnar neuropathies are not related to anesthesia or operative positioning. Instead, poor ulnar hygiene may predate the operation, or, more likely, it may arise in the period between the time patients are removed from the operating room table and the time when they become alert enough to protect themselves from excessive or prolonged exposure to pressure on the ulnar nerve.
Treatment Effectiveness
CARPAL TUNNEL SYNDROME
The management of carpal tunnel syndrome presents an excellent opportunity to utilize techniques of evidence-based medicine. Multiple randomized clinical trials have investigated the effectiveness of splinting, steroid injections, open release, and endoscopic release (Table 8-4).
A meta-analysis of trials of conservative therapy found varying quality of data to support nonoperative therapy. Based on limited evidence, steroid injections appear to be effective. Diuretics, pyridoxine, nonsteroidal antiinflammatory drugs (NSAIDS), yoga, and laser acupuncture seem to be ineffective. Splinting provides some relief but is not as effective as surgery.23 The Maine Carpal Tunnel Study, a prospective, community-based, observational study of 429 patients, showed that nonoperatively managed patients experienced no significant improvement in clinical status at 6, 18, and 30 months follow-up.24 These findings are from a much larger group of patients and draw into question the results from the small natural history study described earlier. A review of the literature related to CTS from 1987–1995 evaluating multiple randomized trials determined that there was limited evidence that steroid injection, vitamin B6, splinting, cognitive therapy, and rehabilitation reduced pain and shortened time away from work.25 The small number of well-controlled trials available for the analysis qualifies these conclusions.
Several trials have focused on surgical therapy for CTS. A Cochrane Database (http://www.cochrane.org) systemic review of surgery versus conservative therapy found that surgery relieves symptoms considerably better than splinting.26 The use of endoscopy to minimize surgical incisions and postoperative discomfort is gaining popularity. Randomized trials have demonstrated that it may be applied safely to large numbers of patients.27,28 A systematic review from the Cochrane Database, however, does not support replacement of the open surgical approach with any alternative.29 Inadequate concealment or insufficient statistical detail is cited as a limitation to several studies. The authors conclude that there is insufficient evidence to support any difference between endoscopic and open techniques. Given that open techniques are more familiar to more practitioners and less technically demanding, the authors conclude that the open method incurs less risk of complication and less cost.
ULNAR NERVE ENTRAPMENT AT THE ELBOW
A search of the existing English language literature regarding the treatment of UNE yielded 169 references. Almost all of these references consist of retrospective reviews of one therapeutic intervention. Only one controlled prospective study and two comprehensive meta-analyses review the management of UNE in patients without other comorbidities. (Table 8-5)
A prospective study of epicondylectomy compares it to anterior subcutaneous ulnar-nerve transposition.30 Fifty-two patients were randomized to either medial epicondylectomy or anterior transposition of the ulnar nerve. Forty-three patients with 47 affected ulnar nerves completed the study and were available for follow-up. At a mean follow-up interval of 4.5 years, the study found no significant difference between the two in terms of muscle atrophy, paresthesias, two-point discrimination, or muscle power. Patients in the anterior transposition group reported more hand pain, had a lower opinion of recovery, and were less inclined to have surgery again than those in the medial epicondylectomy group. The authors conclude that medial epicondylectomy is preferable to anterior transposition in achieving patient satisfaction.
One meta-analysis reviews the available literature for surgical and nonoperative management of ulnar neuropathy.31 This meta-analysis is greatly limited by virtue of the fact that the studies were nonrandomized, included different outcome measures, and reported severity of disease in different ways. The analysis includes 903 patients studied in 30 reports between 1945 and 1995. The severity of the disease was stratified as minimum, moderate, or severe using the Dellon criteria.32 In all, 54 patients were treated nonoperatively, 294 with simple decompression, 166 with medial epicondylectomy, 175 with anterior subcutaneous transposition, and 214 with submuscular transposition. Among the patients with minimal symptoms, there was no statistical difference for satisfaction rates observed among any of the therapeutic modalities. Normal strength was more likely after medial epicondylectomy and least likely with nonoperative management. Among those with moderate disease, total relief, patient satisfaction, and the lowest recurrence rate occurred with submuscular transposition. Nonoperative therapy was associated with the highest incidence of recurrence and the least patient satisfaction. Finally, among those with severe disease, all modalities yielded poor results. No treatment was statistically more likely to lead to total relief and all modalities yielded similarly poor results. Medial epicondylectomy led to the lowest patient satisfaction and was equally likely to lead to recurrence as nonoperative therapy. The authors conclude that minimal disease is best treated initially with nonoperative therapy followed by medial epicondylectomy. Moderate disease responds best to submuscular transposition. The lack of evidence to support any one therapy for severe disease emphasizes the importance of early treatment for ulnar neuropathy.
| Reference | Purpose | Design | Diagnostic | Subjects | Conclusion |
|---|---|---|---|---|---|
| Gerritsen et al, 200223 | To study the effectiveness of conservative therapies | Meta-analysis of 14 randomized, controlled trials of conservative treatment | Inclusion criteria: Patients with CTS, efficacy of one or more conservative treatment options, randomized controlled trial design | Limited and conflicting evidence; no conclusions could be drawn. | |
| Katz et al, 199824 | Outcomes comparison of operative versus nonoperative and open versus endoscopic release for CTS | Prospective, community-based observational study | History and physical examinations | 429 patients; 270 had surgery, 125 no surgery, and 34 crossed over from nonoperative to surgery cohort. | Operative cohort showed 25-45% improvement in symptomatic and functional scores. Nonoperative showed no changes at 6, 18, 30 months. No difference between endoscopic and open release. |
| Feuerstein et al, 199925 | To evaluate effectiveness of different therapies | Meta-analysis of outcome studies | 34 English language articles including prospective and retrospective studies | Limited evidence, multiple study designs limited conclusions. Possible benefit from steroid injections, splinting, behavioral therapy, and occupational therapy. | |
| Verdugo et al, 200326 | To evaluate surgical versus nonsurgical treatment of CTS | Cochrane database review of randomized controlled trials | Identified to randomized controlled trials that met inclusion criteria | 198 patients in total | Surgical treatment relieves symptoms better than splinting. |
| Brown et al, 199327 | To compare open versus endoscopic release of CTS | Prospective, randomized trial | Physical exam and NCS | 85 hands randomized to open, 84 to endoscopic | Endoscopic technique resulted in quicker restoration of function and return to work but more complications. |
| Trumble et al, 200228 | To compare endoscopic and open carpal tunnel release | Prospective, randomized trial | Physical exam, NCS | 95 hands open, 97 hands endoscopic (147 total patients) | Endoscopic release results in greater relief of symptoms, improvement in function, and patient satisfaction during first 3 months only. |
Abbreviations: CTS, carpal tunnel syndrome; NCS, nerve conduction studies.
| Reference | Purpose | Design | Diagnostic | Subjects | Conclusion |
|---|---|---|---|---|---|
| Geutjens et al, 199630 | To compare ME with AT for the treatment of UNE | Randomized clinical trial | Physical exam and NCS | 43 patients, four with bilateral operations | Patient satisfaction (p = 0.04) and pain (p = 0.03) both significantly better with ME than AT. No statistical difference between the two for other motor or sensory outcomes. |
| Mowlavi et al, 200031 | To review the literature regarding the treatment of UNE | Meta-analysis | Thirty studies with data of pre- and posttreatment staging and outcome from 1945–1995 were reviewed. | 903 patients treated with nonoperative management (n = 54), surgical decompression (n = 294), ME (n = 166), AT (n = 175), and SMT (n = 214) | In minimum-stage disease, all modalities were equivalent. Moderate disease responded best to SMT. Poor outcomes for all modalities in severe-stage disease. |
| Bartels et al, 199833 | To review the literature regarding surgical management of UNE | Meta-analysis | Review of the literature from 1970–1997. Of 192 retrieved, 60 met inclusion criteria. | 3024 patients. ME (n = 457), decompression (n = 1262), AT (n = 505), IMT (n = 302), SMT (n = 498) | There was no significant difference between surgeries among patients with mild and moderate disease. Among patients with severe disease, IMT yielded the best results. |
Abbreviations: AT, anterior subcutaneous transposition; IMT, intramuscular transposition; ME, medial epicondylectomy; NCS, nerve conduction studies; SMT, submuscular transposition; UNE, ulnar nerve entrapment.
A second meta-analysis reviews only the surgical management of UNE.33 This study includes the period from 1970 to 1997. The authors included 60 reports on the topic. These reports review the experience of 3024 patients treated with simple decompression, anterior subcutaneous transposition, anterior intramuscular transposition, and anterior submuscular transposition. In this analysis, preoperative condition was assessed using McGowan’s grading scale.34 According to that scale, grade 1 is assigned to purely subjective symptoms and mild hypesthesia, grade 2 to sensibility loss and weakness of intrinsic hand muscles with or without atrophy, and grade 3 to severe sensory motor deficit. When patient outcomes for the 2040 limbs available at follow-up were analyzed without considering preoperative condition, simple decompression had the most favorable result. When preoperative condition was considered, there was no statistical difference between any of the operations among patients with mild (McGowan grade 1 and grade 2) disease. Anterior intramuscular transposition offered the best result in the more severe cases. Many of the studies included in the analysis do not include data regarding operative complications. As a result, any comparison between the operative modalities is accordingly limited. The authors conclude that, for mild (McGowan grade 1 and grade 2) disease, simple decompression offers adequate decompression while remaining minimally invasive and maintaining adequate vascular supply to the nerve. For more severe cases, anterior intramuscular transposition offers the best outcomes with submuscular transposition and simple decompression as acceptable alternatives.
Conclusion
References
- Homan, MM, Franzblau, A, Werner, RA, Albers, JW, Armstrong, TJ, Bromberg, MB. Agreement between symptom surveys, physical examination procedures and electrodiagnostic findings for the carpal tunnel syndrome. Scand J Work Environ Health 1999;25(2):115–124
- Priganc, VW, Henry, SM. The relationship among five common carpal tunnel syndrome tests and the severity of carpal tunnel syndrome. J Hand Ther 2003;16(3):225–236
- Gellman, H, Gelberman, RH, Tan, AM, Botte, MJ. Carpal tunnel syndrome: an evaluation of the provocative diagnostic tests. J Bone Joint Surg Am 1986;68(5):735–737
- Bindra, RR, Evanoff, BA, Chough, LY, Cole, RJ, Chow, JC, Gelberman, RH. The use of routine wrist radiography in the evaluation of patients with carpal tunnel syndrome. J Hand Surg [Am] 1997;22(1):115–119
- Chiou, HJ, Chou, YH, Cheng, SP,, et al. Cubital tunnel syndrome: diagnosis by high-resolution ultrasonography. J Ultrasound Med 1998;17(10):643–648
- Jordan, R, Carter, T, Cummins, C. A systematic review of the utility of electrodiagnostic testing in carpal tunnel syndrome. Br J Gen Pract 2002;52(481):670–673
- Massy-Westropp, N, Grimmer, K, Bain, G. A systematic review of the clinical diagnostic tests for carpal tunnel syndrome. J Hand Surg [Am] 2000;25(1):120–127
- Boniface, SJ, Morris, I, Macleod, A. How does neurophysiological assessment influence the management and outcome of patients with carpal tunnel syndrome? Br J Rheumatol 1994;33(12):1169–1170
- Glowacki, KA, Breen, CJ, Sachar, K, Weiss, AP. Electrodiagnostic testing and carpal tunnel release outcome. J Hand Surg [Am] 1996;21(1):117–121
- Merlevede, K, Theys, P, van Hees, J. Diagnosis of ulnar neuropathy: a new approach. Muscle Nerve 2000;23(4):478–481
- Odusote, K, Eisen, A. An electrophysiological quantitation of the cubital tunnel syndrome. Can J Neurol Sci 1979;6(4):403–410
- Novak, CB, Lee, GW, Mackinnon, SE, Lay, L. Provocative testing for cubital tunnel syndrome. J Hand Surg [Am] 1994;19(5):817–820
- Britz, GW, Haynor, DR, Kuntz, C,, et al. Ulnar nerve entrapment at the elbow: correlation of magnetic resonance imaging, clinical, electrodiagnostic, and intraoperative findings. Neurosurgery 1996;38(3):458–465
- Resende LA, Tahara, A, Fonseca, RG, Sardenberg, T. The natural history of carpal tunnel syndrome: a study of 20 hands evaluated 4 to 9 years after initial diagnosis. Electromyogr Clin Neurophysiol 2003;43(5):301–304
- Padua, L, Aprile, I, Caliandro, P, Foschini, M, Mazza, S, Tonali, P. Natural history of ulnar entrapment at elbow. Clin Neurophysiol 2002;113(12):1980–1984
- Stevens, JC, Witt, JC, Smith, BE, Weaver, AL. The frequency of carpal tunnel syndrome in computer users at a medical facility. Neurology 2001;56(11):1568–1570
- Deltombe, T, Theys, S, Jamart, J, Valet, F, Kolanowski, E, Hanson, P. Protective effect of glove on median nerve compression in the carpal tunnel. Spinal Cord 2001;39(4):215–222
- Rempel, D, Manojlovic, R, Levinsohn, DG, Bloom, T, Gordon, L. The effect of wearing a flexible wrist splint on carpal tunnel pressure during repetitive hand activity. J Hand Surg [Am] 1994;19(1):106–110
- McKenzie, F, Storment, J, Van Hook, P, Armstrong, TJ. Aprogram for control of repetitive trauma disorders associated with hand tool operations in a telecommunications manufacturing facility. Am Ind Hyg Assoc J 1985;46(11):674–678
- May, DC. Results of an OSHA ergonomic intervention program in New Hampshire. Appl Occup Environ Hyg 2002;17(11):768–773
- Lincoln, AE, Vernick, JS, Ogaitis, S, Smith, GS, Mitchell, CS, Agnew, J. Interventions for the primary prevention of work-related carpal tunnel syndrome. Am J Prev Med 2000;18(4 Suppl):37–50
- Warner, MA, Warner, ME, Martin, JT. Ulnar neuropathy: incidence, outcome, and risk factors in sedated or anesthetized patients. Anesthesiology 1994;81(6):1332–1340
- Gerritsen, AA, de Krom, MC, Struijs, MA, Scholten, RJ, de Vet, HC, Bouter, LM. Conservative treatment options for carpal tunnel syndrome: a systematic review of randomised controlled trials. J Neurol 2002;249(3):272–280
- Katz, JN, Keller, RB, Simmons, BP,, et al. Maine Carpal Tunnel Study: outcomes of operative and nonoperative therapy for carpal tunnel syndrome in a community-based cohort. J Hand Surg [Am] 1998;23(4):697–710
- Feuerstein, M, Burrell, LM, Miller, VI, Lincoln, A, Huang, GD, Berger, R. Clinical management of carpal tunnel syndrome: a 12-year review of outcomes. Am J Ind Med 1999;35(3):232–245
- Verdugo, RJ, Salinas, RS, Castillo, J, Cea, JG. Surgical versus non-surgical treatment for carpal tunnel syndrome. Cochrane Database Syst Rev 2003;3:CD001552
- Brown, RA, Gelberman, RH, Seiler, JG III,, et al. Carpal tunnel release: a prospective, randomized assessment of open and endoscopic methods. J Bone Joint Surg Am 1993;75(9):1265–1275
- Trumble, TE, Diao, E, Abrams, RA, Gilbert-Anderson, MM. Single-portal endoscopic carpal tunnel release compared with open release: a prospective, randomized trial. J Bone Joint Surg Am 2002;84–A(7):1107–1115
- Scholten, RJ, Gerritsen, AA, Uitdehaag, BM, van Geldere, D, de Vet, HC, Bouter, LM. Surgical treatment options for carpal tunnel syndrome. Cochrane Database Syst Rev 2002;4:CD003905
- Geutjens, GG, Langstaff, RJ, Smith, NJ, Jefferson, D, Howell, CJ, Barton, NJ. Medial epicondylectomy or ulnar-nerve transposition for ulnar neuropathy at the elbow? J Bone Joint Surg Br 1996;78(5):777–779
- Mowlavi, A, Andrews, K, Lille, S, Verhulst, S, Zook, EG, Milner, S. The management of cubital tunnel syndrome: a meta-analysis of clinical studies. Plast Reconstr Surg 2000;106(2):327–334
- Dellon, AL. Review of treatment results for ulnar nerve entrapment at the elbow. J Hand Surg [Am] 1989;14(4):688–700
- Bartels, RH, Menovsky, T, Van Overbeeke, JJ, Verhagen, WI. Surgical management of ulnar nerve compression at the elbow: an analysis of the literature. J Neurosurg 1998;89(5):722–727
- McGowan, AJ. The results of transposition of the ulnar nerve for traumatic ulnar neuritis. J Bone Joint Surg Br 1950;32–B(3):293–301
- Priganc, VW, Henry, SM. The relationship among five common carpal tunnel syndrome tests and the severity of carpal tunnel syndrome. J Hand Ther 2003;16(3):225–236
< div class='tao-gold-member'>







