7 Peripheral Nerves
General
 History and Physical
History and Physical
1. What types of sensation are affected in amyotrophic lateral sclerosis (ALS)?
None, sensation is intact.
2. What muscle group should be examined in the lower extremities to differentiate a foot drop from radiculopathy versus a foot drop from peroneal nerve palsy?
Test foot inversion, which is controlled by the tibialis posterior and anterior. In a pure peroneal neuropathy, foot inversion is intact. Also note that gluteus medius (internal rotation of a flexed hip) is spared in peroneal nerve palsy.1
3. What is the usual presentation of anterior interosseous nerve entrapment?
Pain located in the proximal forearm that increases with exercise and decreases with rest; up to 85% of patients will present in this way.2
4. What muscles are involved in anterior interosseous nerve entrapment?
Flexor digitorum profundus 1 and 2, flexor pollicis longus, and the pronator quadratus3
5. What symptoms may be present with the rare T1 radiculopathy caused by a Pancoast tumor in the apical pleura of the lung?
Irritation in the medial upper arm and a Horner syndrome4
6. What are the standard laboratory tests in a peripheral neuropathy workup?
Thyroid panel, rheumatology profiles, vitamin B12, folic acid, hemoglobin A1C, erythrocyte sedimentation rate, rapid protein reagent, heavy metals, and immunoelectrophoresis of serum protein1
7. What is a Froment sign?
Paralysis of the adductor pollicis produces a Froment sign; when grasping a piece of paper between the thumb and index finger, the flexor pollicis longus is used (resulting in interphalangeal [IP] joint flexion) because the adductor pollicis does not work.5
8. What is the pinch or “O” sign?
To test for anterior interosseous nerve palsy, the thumb and index finger are unable to make a circle (“O”); instead, the pulps of the thumb and index finger touch each other. This is the result of weakness of flexion of the distal phalanges (Fig. 7.1).3,5
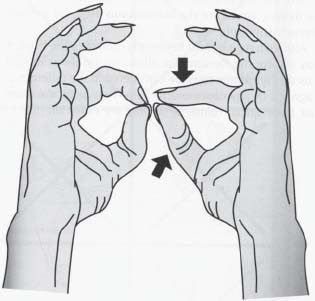
Fig. 7.1 Pinch or “O” sign. (Reprinted with permission from Alberstone et al6)
9. How can one differentiate an ulnar nerve injury below the midforearm and an ulnar nerve injury above the midforearm if there are no external signs of injury to the arm?
If the ulnar nerve is divided below the midforearm, an ulnar claw hand is produced. The fourth and fifth digits are hyperextended at the metacarpopharyngeal (MP) joints by the long extensors, but are flexed at the IP joints. This posture is sometimes called the “hand of benediction.” If an ulnar nerve lesion is above the midforearm, the clawing of the ulnar side two fingers may not occur if the extrinsic muscles producing IP joint flexion are also denervated.5
10. How does a lower plexus lesion result in a claw hand?
Lower brachial plexus lesions are usually injuries caused by excessive abduction of the arm as a result of someone clutching for an object when falling from a height. The first thoracic nerve (T1) is usually torn. The fibers from this segment of the spinal cord help form the ulnar and median nerves; the small muscles of the hand (interossei and lumbricals) are affected and the hand has a clawed appearance due to hyperextension of the MP joints and flexion of the IP joints. The extensor digitorum is unopposed by the lumbricals and extends the MP joints. Because the flexor digitorum superficialis and profundus are unopposed by the lumbricals and interossei, the claw hand results. There is also sensory loss along the medial side of the forearm, hand, and medial two fingers. Lower brachial plexus lesions may also be the result of malignant metastases from the lungs in the lower deep cervical lymph nodes and an aberrant cervical rib.7
11. A golfer complains of palmar pain on the ulnar side of the hand that is aggravated by grasping his club; what is the primary diagnosis?
Hook of hamate fracture. The hook of the hamate forms the lateral (radial) border of tunnel of Guyon, which transports the ulnar nerve and artery to the hand.8
12. What branch of the ulnar nerve takes an abrupt turn around the hook of the hamate?
The deep branch8
13. In neuropathies which muscles most commonly first show wasting in the upper extremities? In the lower extremities?
The first dorsal interosseus muscle in the upper limbs and extensor digitorum brevis in the lower limbs
14. What is the rate of axonal regeneration in a peripheral nerve lesion?
In a peripheral nerve injury, the axon progresses down the distal stump at a rate of 1 mm per day. The rate is greater if the lesion is close to the central nervous system and lesser if the injury is more distal. Thus proximal lesions may grow as rapidly as 2 to 3 mm per day, whereas distal lesions may progress as slowly as 0.5 mm per day.1,5
15. What is the significance of a positive Tinel sign in the setting of peripheral nerve regeneration?
A Tinel sign signifies that fine fibers have reached the area of stimulation. If the nerve is indeed regenerating, then the patient will report paresthesias in the distribution of the nerve that is stimulated. The absence of a Tinel sign many months after injury may be an indication for operative exploration.5
16. How can one radiologically differentiate ganglia from other masses such as schwannomas?
Ganglia exhibit lack of contrast enhancement and display a connection with the joint space. For example, in peroneal nerve compression, a paraarticular ganglia is connected to the superior tibiofibular joint capsule.
17. What type of neuropathy can a patient with acquired immunodeficiency syndrome (AIDS) have?
AIDS patients can present with a distal sensory neuropathy or an antiretroviral toxic neuropathy caused by exposure to specific nucleoside reverse transcriptase inhibitors. The conditions can coexist as well resulting in burning dysesthesias and debilitating paresthesias. Symptoms are typically limited to the feet, but often extend to the lower extremities.1,9
18. Describe the Sunderland classification of a seventh cranial nerve injury.
• First degree
• Neurapraxia
• Nerve fiber and covering are intact.
• No Wallerian degeneration
• Full recovery
• Nerve stimulation across the nerve is not present initially.
• Second degree
• Axonotmesis
• Endoneurium is intact.
• Wallerian degeneration in 24 hours
• Axon regeneration
• Potential full recovery
• Third degree
• Neurotmesis
• Endoneurium is damaged.
• Wallerian degeneration
• Synkinesis
• Incomplete recovery
• Fourth degree
• Neurotmesis
• Perineurium is damaged.
• Wallerian degeneration
• Worse synkinesis
• Less recovery
• Fifth degree
• Epineurium also is damaged.
• No recovery unless repaired
 Emergencies
Emergencies
19. What is the most common neuropathy in a patient on anticoagulation medication?
Femoral neuropathy from a hematoma near the psoas muscle1
20. What is the diagnosis of progressive paralysis, an expanding mass in a limb, and/or a bruit detected in that limb?
An aneurysm or fistula may be present and urgent decompression may be required.
 Technique
Technique
21. Where is the approximate location of the sural nerve?
Halfway between the lateral malleolus and Achilles’ tendon3
22. What are the steps in performing a sural nerve biopsy?
The patient is supine with the leg elevated. A 3-cm incision is made proximal to the lateral malleolus at the groove formed by the lateral malleolus and the Achilles’ tendon. A 2- to 3-cm piece of whole nerve is sectioned and given to the pathologist. Make sure that on closing the proximal stump of nerve does not retract beyond the incision line and become entrapped within the healing skin.3
23. How is a sural nerve block performed?
The needle is introduced just lateral to the Achilles’ tendon ~1 to 2 cm proximal to the level of the distal tip of lateral malleolus. The needle is directed to the posteromedial aspect of the fibula and 5 mL of anesthetic is injected after aspiration of the syringe to ensure that a vessel was not breached.10
24. How does one administer a Tensilon test?
One milliliter of 1% edrophonium chloride (10 mg/mL, Tensilon) is prepared. The patient is given an initial dose of 0.1mL and observed for a response. If the patient’s symptoms do not change, the remaining 0.9 mL is administered and the response observed again. Administration of an acetylcholinesterase (AChE) inhibitor, such as edrophonium, causes transient improvement in symptoms of myasthenia gravis.9
25. Where is the location of an incision in tarsal tunnel surgery?
Start 2 cm proximal to the medial malleolus, about halfway between the medial malleolus and the Achilles tendon. The incision is extended distally, directly superficial to the course of the posterior tibial nerve.3
26. Where is the greater saphenous vein located?
Immediately posterior to the medial malleolus and superficial to the medial malleolar ligament. It is important to identify the distal portion of the vein during dissection so that the proper orientation of the valves is made when grafting the vein to another location.11
27. How is a tibial nerve block performed?
The posterior tibial artery is palpated as a landmark. The needle is passed adjacent to the Achilles tendon toward the posterior tibial artery behind the medial malleolus. To block the posterior tibial nerve, direct the needle just medial to the Achilles tendon. Proceed with the needle through the deep fascia until it impinges on the bone behind the medial malleolus. After aspiration, 5 mL of anesthetic is injected.12
28. Where is the location for harvesting the medial antebrachial cutaneous nerve for a graft?
The medial antebrachial cutaneous nerve can be used for nerve cable grafts. The anterior branch of this nerve is harvested two fingerbreadths anterior and distal to the medial epicondyle.13
29. How does one perform a suprascapular nerve block?
A suprascapular nerve block is performed by needle insertion behind the lateral end of the clavicle at its junction with the insertion of the trapezius muscle; the needle is directed downward and backward.14
30. Where is the palmar cutaneous branch of the median nerve and in what common surgery is it at risk?
The palmar cutaneous branch of the median nerve arises from the radial border of the median nerve ~5 to 6 cm proximal to distal transverse flexion crease of the wrist. It runs along the median nerve for 2 to 3 cm, and then runs along the ulnar border of the flexor carpi radialis tendon. An anatomic cadaver study showed that in no case did the palmar cutaneous branch extend ulnar to the axial line of the ring finger. It is at risk in carpal tunnel surgery. That is why it is important to err on the ulnar side when performing carpal tunnel surgery.3,8
31. What are the complications of carpal tunnel operations?
1. Inadequate release of the ligament resulting in persistence of symptoms
2. Postoperative fibrosis
3. Tender neuroma of the palmar cutaneous branch of the median nerve
4. Hypertrophic scars
5. Section of the motor branch, resulting in complete denervation and atrophy of the thenar muscle mass
6. Reflex sympathetic dystrophy
7. Bowstringing of the flexor tendons
8. Wound infection and hematoma8
32. What is pillar pain?
Pillar pain is a deep wrist pain after carpal tunnel release thought to result from a redistribution of forces between the carpal bones after the surgery. It usually subsides spontaneously after carpal tunnel surgery in ~6 months.15
33. What is the significance of nerve action potential recordings across a lesion in determining what type of surgery is to be done?
If no potential is recorded distal to the lesion, it is resected and a repair is done. When a nerve action potential is recorded, then only a neurolysis is performed. Neurolysis is usually the initial technical step in the surgical management of any lesion in continuity.3
34. What are the most common causes of failure of nerve repair?
The leading causes of failure of nerve repair back to healthy tissue are inadequate resection and distraction of the repair site. Use of grafts can help with this problem as the surgeon is encouraged to resect back to healthy nerves and using grafts permits repair with minimal tension. The use of grafts is not advisable for making up small gaps that can be readily closed with proper mobilization and end-to-end repair.3
35. When harvesting iliac crest bone for a fusion procedure, what nerve is at risk if the bone is harvested too far laterally?
The surgeon may use the medial 6 to 8 cm of the iliac crest to avoid injuring the superior cluneal nerves (Fig. 7.2).16
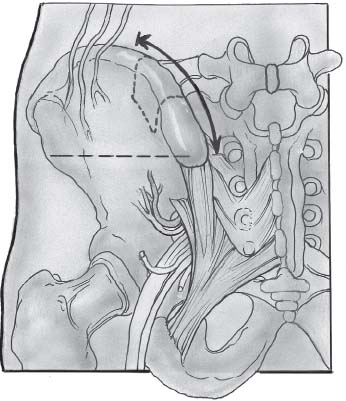
Fig. 7.2 Illustration of posterior iliac crest bone graft harvesting. Note the location of the superior cluneal nerves lateral to the incision site. (Reprinted with permission from Fessler & Sekhar, p. 77917)
 Electrophysiology
Electrophysiology
36. What are three crucial phases one needs to record when performing electromyography (EMG)?
1. Recording of insertional activity
2. Determination of the presence or absence of spontaneous discharges at rest
3. Assessment of the presence and type of muscle action potential5
37. What are some findings on EMG that one sees with nerve compression?
1. Sharp positive waves
2. Insertional activity
3. Fibrillations
4. Spontaneous rest activity
5. Decreased recruitment18
38. What is the electrophysiologic equivalent of the tendon jerk?
An H reflex18
39. What electrophysiologic reflex occurs with supra-maximal stimulus to the nerve?
An F reflex18
40. What is the only muscle from which an H reflex can be readily elicited?
Soleus (in response to stimulation of the posterior tibial nerve)18
41. Compare and contrast a neurogenic motor unit potential from a myogenic motor unit potential.
Both are polyphasic; however, neurogenic motor unit potentials have increased amplitude and long duration compared with myogenic (reduced amplitude and short duration).18
42. What else must be present in an EMG examination for an observed fasciculation to be considered abnormal?
Fibrillations and/or positive sharp waves18
43. What is the most common disorder of neuromuscular transmission?
Myasthenia gravis
44. Is electrodiagnostic testing useful in the acute setting?
A frequent misconception is that electrodiagnostic testing is not useful in an acute injury. EMG changes take 1 to 3 weeks to become recordable in the muscles. Nerve conduction abnormalities, however, are present immediately and can be helpful in the immediate determination of the extent of injury.1
45. What study, if positive, increases the diagnostic yield of a sural nerve biopsy?
Nerve conduction velocities. Decreased nerve conduction velocities in the lower extremities increases the diagnostic yield of a sural nerve biopsy.
46. What is the Erb point?
The point on the side of the neck 2 to 3 cm above the clavicle and in front of the transverse process of the sixth cervical vertebra. Pressure over this point elicits Duchenne-Erb paralysis, and electrical stimulation over this area causes various arm muscles to contract.1
47. Fibrillations, fasciculations, and atrophy are all manifestations of what type of nerve injury?
Lower motor neuron paralysis18
 Pain
Pain
48. What are common causes of neuropathic pain?
1. Diabetic neuropathy
2. Alcoholic neuropathy
3. Acute inflammatory demyelinating polyradiculopathy
4. HIV-related neuropathy
5. Postherpetic neuralgia
6. Trigeminal neuralgia
7. Posttraumatic neuralgia
8. Postradiation plexopathy
9. Thalamic stroke
10. Radiculopathy caused by spinal osteoarthritis or discopathy, compressive myelopathy1



