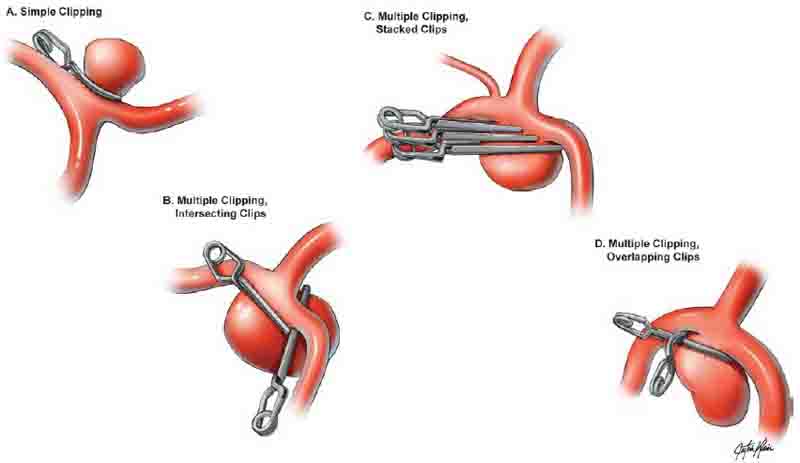
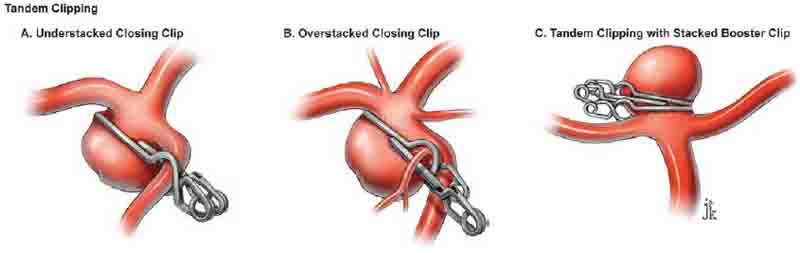
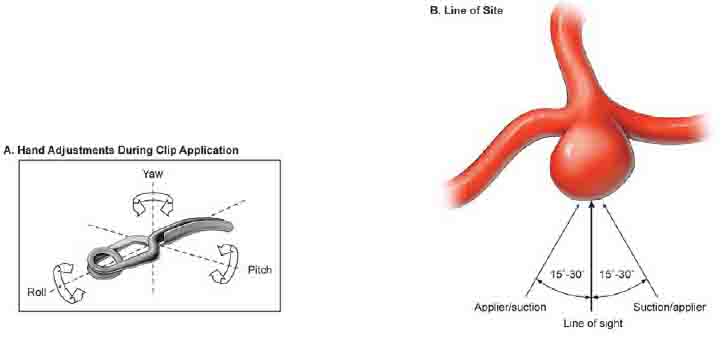
6 Permanent Clipping Applying a permanent clip on an aneurysm neck is like landing an airplane, requiring just the right “yaw, pitch, and roll” (Fig. 6.1A). Pitch refers to the slope of the clip appliers; yaw refers to the side-to-side rotation of the clip appliers about a vertical axis; and roll refers to the side-to-side rotation of the clip appliers about the instrument’s axis. Adjustments are made by the wrist while the hand and fingers stabilize the appliers, squeeze it to open the clip blades, and gently release pressure when the clip is in position. With small, sessile aneurysms, downward pressure may also be required as the clip is released. Permanent clip application demands complete visualization from start to finish, from the introduction of permanent clips into the field to their release from the appliers. Both sides of the aneurysm neck, both clip blades, and the adjacent anatomy are brought into one panoramic view by shifting the microscope, decreasing the zoom, and adjusting retractors. Clip appliers obstruct an established line of sight if they enter the surgical corridor along or near the line of sight; a 15- to 30-degree difference between the appliers’ line and the sight line is needed to visualize the blades on the aneurysm neck (Fig. 6.1B). The appliers’ line is often fixed by the aneurysm anatomy, which requires shifting the microscope to offset the sight line. Clip application should not proceed without complete visualization. Rhoton introduced four rules about aneurysms: aneurysms arise at branching sites on the parent artery, which may be a side branch or a bifurcation (rule 1); aneurysms arise at turns or curves in the outer wall of the artery where hemodynamic stress is greatest (rule 2); aneurysms point in the direction that blood would have gone if the curve at the aneurysm site was not present (rule 3); and each aneurysm is associated with a set of perforating arteries that needs to be preserved (rule 4). According to rule 1, the clip should be applied perpendicular to the afferent artery and parallel to the efferent branches with bifurcation aneurysms (e.g., middle cerebral artery [MCA] and basilar bifurcation aneurysms). According to rules 2 and 3, the clip is applied parallel to the parent artery with aneurysms at curves (e.g., ophthalmic artery [OphA] and superior hypophyseal artery [SHA] aneurysms). According to rule 4, the clip is applied parallel to the line of perforators across an aneurysm base (e.g., anterior communicating artery [ACoA] and basilar bifurcation aneurysms). Not every aneurysm conforms to Rhoton’s rules, but analyzing aneurysm anatomy from this perspective helps envision the repair and select appropriate clips. Fig. 6.1 (A) Clip application requires adjusting the yaw, pitch, and roll of the clip. Pitch refers to the slope of the clip appliers; yaw refers to the side-to-side rotation of the clip appliers about a vertical axis; and roll refers to the side-to-side rotation of the clip appliers about the instrument’s axis. (B) Permanent clip application demands complete visualization of the aneurysm neck, both clip blades, and adjacent anatomy. A line of sight is established that brings these together in one panoramic view. The working line of the clip appliers must be 15 to 30 degrees off of the sight line of the microscope to preserve the view. The appliers’ line is often fixed by aneurysm anatomy, which requires shifting the microscope to offset the sight line. Fig. 6.2 Basic clipping techniques. (A) Simple clipping with a single clip. (B) Multiple clipping with intersecting clips. (C) Multiple clipping with parallel stacked clips. (D) Multiple clipping with an overlapping fenestrated clip closing the posterior lobe of aneurysm. A basic rule of aneurysm clipping is “simple is best.” Simple clipping uses a single clip, usually with aneurysms that are small, have narrow necks, and uncomplicated anatomy (Fig. 6.2A). Reliance on a single clip requires the perfect clip size, contour, and configuration. The part of the blade that matters is the part that crosses the neck. Small, deep aneurysms in tight surgical corridors, such as at the basilar apex, may still require long clip blades that move back the clip’s coiled spring and keep the head of the appliers from obstructing the line of sight. Simple clipping may not be possible with aneurysms that are large, have broad necks, and complex anatomy. These aneurysms require multiple clips, which close an aneurysm neck in sequential steps, progressing from deep neck to near neck and tackling the most difficult, inaccessible part first. Multiple clips can contour the neck reconstruction to match the anatomy of the neck and efferent arteries. Multiple clipping strategies are common and include intersecting clips, stacked clips, and overlapping clips. Multiple clipping with intersecting clips uses a second clip angled into an initial clip, with its tips intersecting the blade or heel of the initial clip at an acute, right, or obtuse angle (Fig. 6.2B). Intersecting clips can be simple, such as two straight clips in a T-configuration, or complex, such as multiple straight clips that converge like leaves of a camera’s aperture. Stacked clips are applied parallel to each other (Fig. 6.2C). The initial clip typically closes most of the aneurysm, and tips of subsequent clips precisely contour the remnant beneath the initial clip (understacking). When the initial clip is applied near the neck but does not adequately reconstruct it, subsequent clips stacked above it will complete the closure (overstacking). Stacked clips are all applied in the same direction, which facilitates clipping in tight surgical corridors where the appliers cannot be maneuvered to intersecting angles. Understacking precisely contours the origins of efferent arteries as they exit the aneurysm’s base, and under-stacking with mini-clips eliminates tiny dog-ear remnants. An overlapping fenestrated clip can be applied over an initial straight clip at various angles to close a distal neck remnant beneath the initial clip (Fig. 6.2D). This overlapping clip reconstruction encircles the initial clip blade, bringing the heel of the fenestrated clip blade against the straight clip blade.
 Clip Application
Clip Application
 Simple Clipping
Simple Clipping
 Multiple Clipping
Multiple Clipping
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree