Fig. 18.1
Case 1 (a–f): Preoperative axial (a), coronal (b) and sagittal (c) T1 weighted contrast MRI showing a giant adenoma with moderate suprasellar extension and almost complete filling of the sphenoid sinus. Postoperative day #1 axial (d), coronal (e) and sagittal (f) T1 weighted post-contrast MRI shows gross total tumor removal and pituitary gland re-expansion
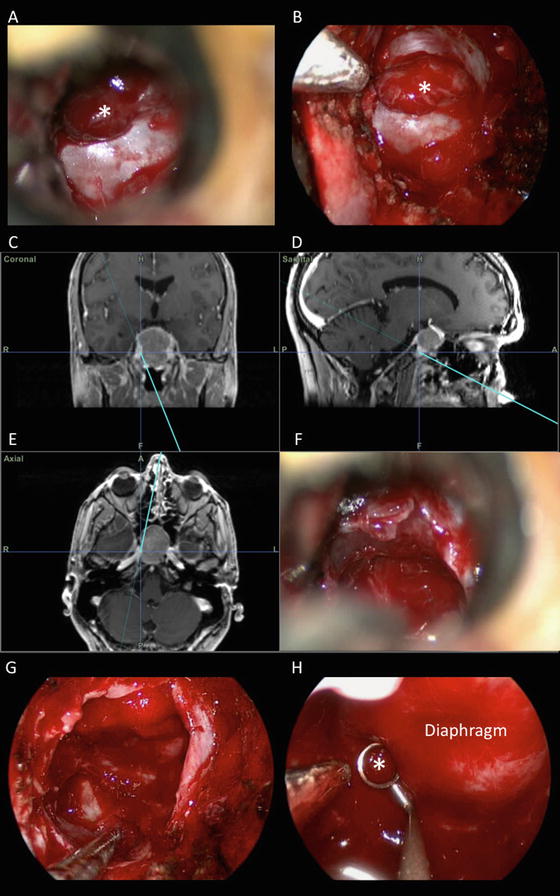
Fig. 18.2
(a–h): Intraoperative images of the endonasal tumor removal described in case 1. Microscopic (a) and endoscopic (b) views of the sellar dura, with superior tumor eroding through dura (*). Navigational images (c, d and e) with pointer along right cavernous sinus wall as seen with microscopic view (f). A 0° endoscopic view after further tumor removal (g) and a 45° endoscopic view of postero-superior sellar cavity (h), where tumor remnants were removed from below compressed gland (*)
Case 2
A 19 year-old woman with infrequent menses since adolescence was found to have an elevated prolactin of 171 ng/ml (normal range 5–23 ng/ml). Pituitary MRI revealed a 15 mm predominantly cystic sellar mass with severe gland compression and evidence of subacute and chronic hemorrhagic changes (Fig. 18.3a, b). Given the hemorrhagic nature of this presumed macroprolactinoma, she underwent endonasal tumor removal (Fig. 18.4). After maximal tumor removal with the microscope, the endoscope revealed no obvious residual adenoma. Her prolactin level decreased to 21 ng/ml on post-operative day #1 and no residual tumor was seen on postoperative MRI. At 13 months after surgery, her menstrual periods were normal, she had no galactorrhea and her MRI showed no obvious adenoma (Fig. 18.3c, d). However, her prolactin level had gradually increased to 43 ng/ml. She was consequently started on a low dose of cabergoline (0.25 mg twice weekly) and continues to do well.
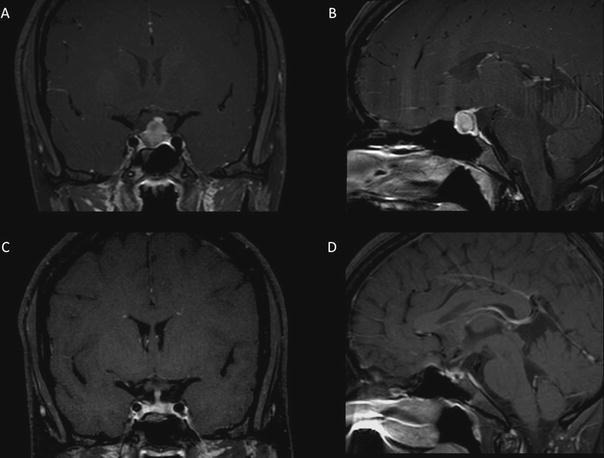
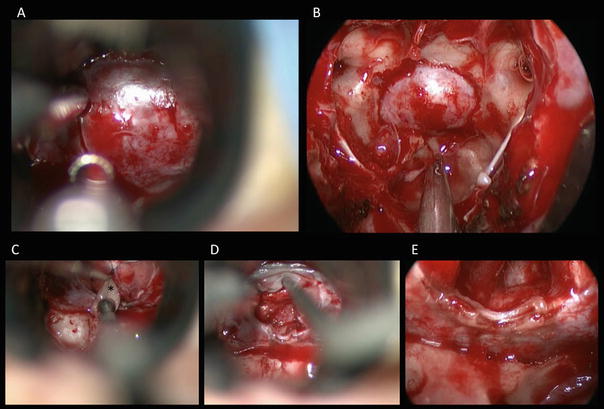
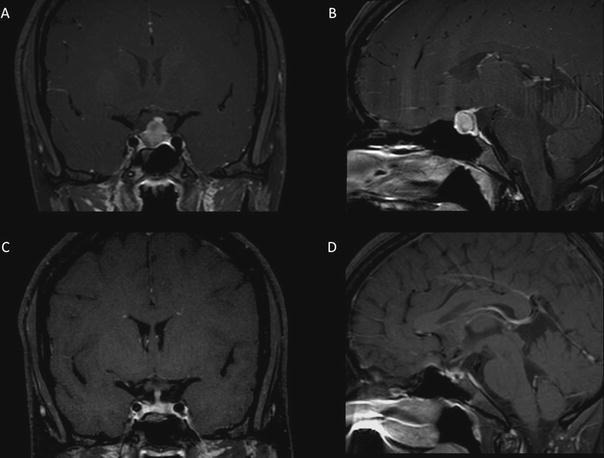
Fig. 18.3
Case 2 (a–d): Preoperative coronal (a) and sagittal (b) T1 weighted post-contrast MRI showing a hemorrhagic pituitary adenoma with leftward pituitary stalk deviation and the normal pituitary gland pushed superiorly and posteriorly. Postoperative coronal (c) and sagittal (d) T1 weighted contrast MRI showing gross total tumor removal with midline pituitary stalk
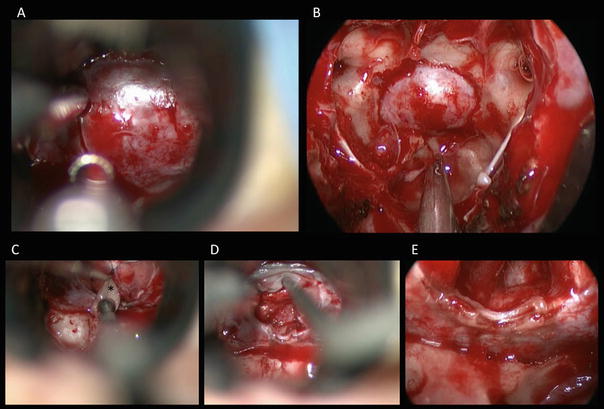
Fig. 18.4
(a–e): Intraoperative images of the endonasal removal or hemorrhagic prolactinoma described in case 2. Microscopic (a) and endoscopic (b) views of the bone window and sellar dura on the posterior surface of the sphenoid sinus. Observe the panoramic view afforded by the 0° endoscope (b). Once the dura is incised under microscopic visualization (c), tumor tissue (*) is removed. The dural opening is then widened to facilitate complete tumor removal (d). The 30° endoscope is brought in at the end of the procedure (e) to inspect the sellar cavity and the areas posterior to the ICAs and lateral sellar compartments, towards the cavernous sinuses. No residual tumor was seen with endoscopic inspection
References
Cushing H (1912) The Pituitary body and its disorders: clinical states produced by disorders of the hypophysis cerebri. J.B. Lippincott, Philadelphia, pp 296–305
Dusick JR, Esposito F, Malkasian D, Kelly DF (2007) Avoidance of carotid artery injuries in transsphenoidal surgery with the Doppler probe and micro-hook blades. Neurosurgery 60(4 Suppl 2):322–328, discussion 328–329PubMed
Esposito F, Dusick JR, Fatemi N, Kelly DF (2007) Graded repair of cranial base defects and cerebrospinal fluid leaks in transsphenoidal surgery. Neurosurgery 60(4 Suppl 2):295–303, discussion 303–294PubMed
Fatemi N, Dusick JR, Malkasian D, McArthur DL, Emerson J, Schad W, Kelly DF (2008b) A short trapezoidal speculum for suprasellar and infrasellar exposure in endonasal transsphenoidal surgery. Neurosurgery 62(5 Suppl 2):ONS325–ONS329, discussion ONS329-330PubMed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








