Pituitary Imaging
Introduction
Magnetic resonance imaging is an excellent imaging modality for pituitary and optic chiasmal disease. However, MDCT is a proven accurate alternative if and when MR is not possible, or cannot be accessed urgently in a patient with acute visual failure. MDCT has been shown superior to MR in assessing the lateral extent of an adenoma and the sellar floor.
The purpose of imaging is to identify the presence or absence of a functioning/nonfunctioning adenoma or any parasellar pathology causing a hormonal abnormality. The effect of any lesion on the adjacent chiasm and the anatomy of the parasellar vessels will all determine future management. An axial helical scan provides isotropic images in all planes and so is superior to angled direct coronal incremental scanning. Careful review of all adjacent structures and the pituitary infundibulum (stalk) is an integral part of pituitary imaging, as disease of the stalk or hypothalamus can produce hormone abnormalities that mimic primary pituitary disease. Presurgical assessment requires comments about the gland, the cavernous sinus, the carotid arteries, and the sphenoid sinus so good vascular contrast is necessary.
Dual bolus contrast acquisition allows time for the normal pituitary tissue to enhance and the second contrast bolus optimizes the vascular data. Single phase scanning is also acceptable but vessels are less well defined.
Indications for pituitary imaging
Hormonal
Hyperprolactinaemia
Acromegaly
Cushings syndrome
Thyroid stimulating hormone excess
Suspected pituitary stalk compression (moderately elevated prolactin)
Hypopituitarism
Apoplexy
Hypogonadism
Structural
Bitemporal hemianopia (nonfunctioning adenoma/suprasellar mass)
Incidentally found enlarged sella on skull radiograph
Technique
Protocol parameters for pituitary imaging are shown in Table 5.1 and surview is shown in figure 5.1A.
Multiplanar reformations in the axial, sagittal, and coronal planes can then be done from the data set. Twelve or 14 images in each plane at slice thickness 2 mm/interspace 2 mm covers the parasellar region. The images below show an example of each and also the reconstructive zoom used for this study.
Reconstruction and reformation
Pathology and illustrations
These will include examples from the list of indications above, including hormonal and structural pathology.
Table 5.1 Protocol parameters for pituitary imaging | ||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
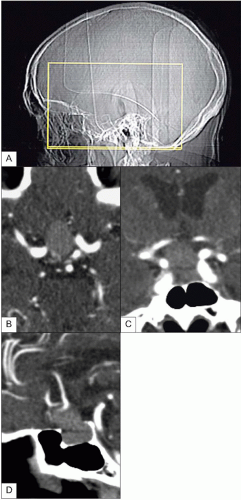 5.1 (A) Surview for pituitary study. Axial (B) coronal (C), and sagittal (D) reormations. In each of these (B-D) the intra- and suprasellar lesion appears well enhanced from the first contrast bolus. Similarly. from the second bolus, the adjacent vessels are very well defined.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





