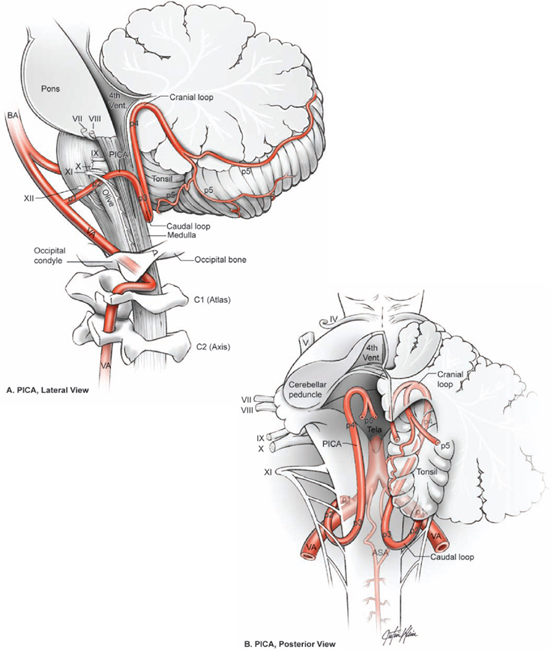
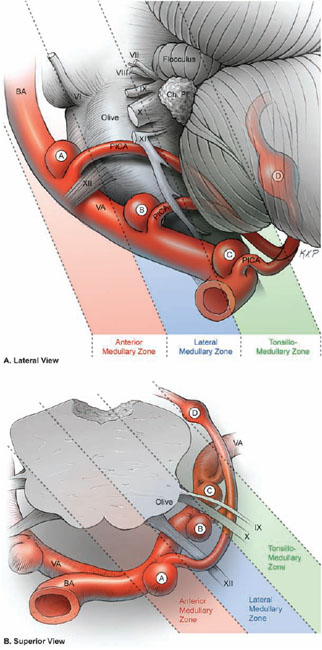
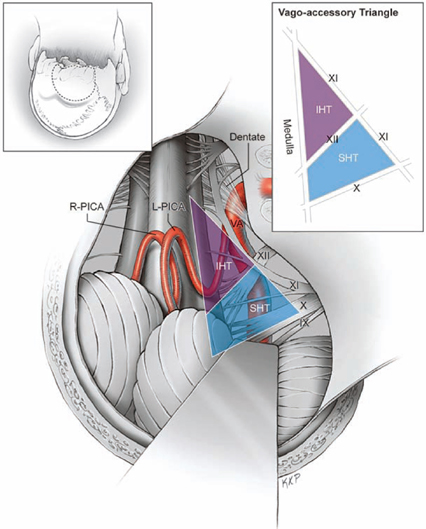
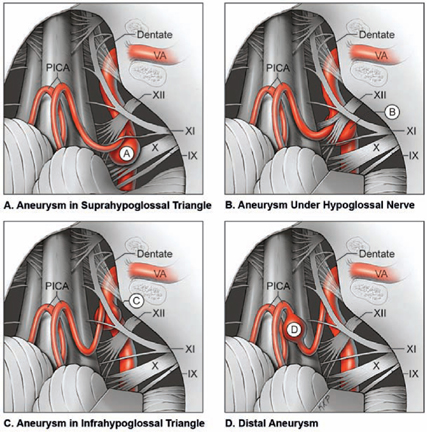
20 Posterior Inferior Cerebellar Artery Aneurysms Vertebral artery originates from the subclavian artery, ascends through the transverse processes of the upper six cervical vertebrae, swings behind the lateral mass of the atlas, passes anterior to the lateral border of the atlanto-occipital membrane, and pierces the dura behind the occipital condyle. The initial intradural vertebral artery (VA) segment passes over the dorsal and ventral roots of the first cervical nerve, and crosses anterior to the dentate ligament and the spinal portion of the accessory nerve. The VA courses from the lower lateral to upper the anterior surface of the medulla, giving off perforators along the way. It passes across the pyramid, joins the contralateral VA at or near the pontomedullary sulcus, and forms the vertebrobasilar junction and basilar trunk (Fig. 20.1). The posterior spinal artery is the first intracranial branch from the VA, although it sometimes arises extradurally and travels with the VA through the dural ring into the subarachnoid space. The posterior spinal artery courses medially behind the dentate ligament, where it divides into ascending and descending branches that supply the dorsal columns and portions of the dorsal cervical spinal cord. The posterior inferior cerebellar artery (PICA) is the next branch and is the VA’s largest, most clinically significant branch. The PICA has five segments defined by its relationship to the lower cranial nerves as it winds around the medulla and the posterior surface of the cerebellum: anterior medullary, lateral medullary, tonsillomedullary, telovelotonsillar, and cortical segments. The anterior medullary segment (p1 segment) begins at the PICA’s origin, lies anterior to the medulla, and extends past the hypoglossal rootlets at the medial edge of the inferior olive. The lateral medullary segment (p2 segment) extends from olive to the rootlets of CN9, CN10, and CN11 at the lateral edge of the olive. The tonsillomedullary segment (p3 segment) begins where the PICA passes under or between the rootlets of the CN9 to CN11 triad, descends to the inferior pole of the cerebellar tonsil, reverses course in the caudal or infratonsillar loop, and ascends along the medial tonsil to its midpoint. The telovelotonsillar segment (p4 segment) begins at the midpoint of the PICA’s ascent along the medial tonsil, continues toward the roof of the fourth ventricle, turns around again to form a cranial or supratonsillar loop, and courses downward and posteriorly to the tonsillobiventral fissure. The telovelotonsillar segment derives its name from its branches to the choroid plexus of the fourth ventricle (tela choroidea) and its association with the roof of the fourth ventricle (inferior medullary velum). The cortical segment (p5 segment) begins as the PICA emerges from the tonsillobiventral fissure, where the tonsil, the vermis, and the biventral lobule of the cerebellar hemisphere meet. This segment consists of numerous trunks and branches, with a medial trunk supplying the vermian surface and a lateral trunk supplying the tonsillar and hemispheric surfaces. The anterior spinal artery is the last branch of the VA proximal to the vertebrobasilar junction (VBJ). It joins the contralateral artery to form a single midline anterior spinal artery that descends through the foramen magnum on the ventral surface of the medulla and spinal cord in or near the anterior median fissure. It supplies the pyramids and their decussation, the medial lemniscus, and the hypoglossal nuclei and nerves. The spinal accessory nerve is an orienting landmark around the foramen magnum because it traverses the entire field in a far-lateral exposure, from its origin from the cervical spinal rootlets, through the foramen magnum, across the VA, to the jugular foramen. CN11 leads to its partners in the jugular foramen, CN9 and CN10. Rootlets of CN9, CN10, and CN11 originate in the groove between the lateral surface of the olive and the posterolateral medulla (retro-olivary sulcus). Rootlets of the hypoglossal nerve originate more anteromedially in the groove between the medial edge of the olive and the medullary pyramids (preolivary sulcus). CN12 rootlets course laterally to the hypoglossal canal, which runs above the anterior third of the occipital condyle. The VA always passes anterior to rootlets of CN9, CN10, and CN11, but can split rootlets of CN12. Ideally, the arachnoid of the cisterna magna is preserved until the microscope is in the field to keep blood out of the subarachnoid space. Once the microscope is in, this arachnoid is incised in the midline from the vermis down to the cervical spinal cord, and incised laterally under the tonsil, which allows the arachnoid to flap laterally against the dura. Fig. 20.1 Microsurgical anatomy of the vertebral artery (VA) and posterior inferior cerebellar artery (PICA). Lateral (A) and posterior (B) views of the PICA and its relationship to the medulla and cerebellum. The PICA segments are seen: p1, anterior medullary segment; p2, lateral medullary segment; p3, tonsillomedullary segment; p4, telovelotonsillar segment; and p5, cortical segments. ASA, anterior spinal artery; BA, basilar artery. The dissection to PICA aneurysms is relatively simple because both the VA and the PICA are identifiable landmarks that lead directly to the aneurysm. The VA is identified under the dentate ligament as described above, and the PICA is identified under the tonsil in the cerebellomedullary fissure, if the caudal loop of the PICA is not already visible in the cisterna magna. One or both arteries are traced proximally to their convergence, and the aneurysm lies just beyond this convergence. Arteries do not traverse a difficult fissure or require extensive dissection. The caudal loop of the PICA at the inferior tonsil is apparent early or with tonsillar retraction. The medulla and the anterior tonsil are easily separated because their surfaces are smooth, distinct, and never interdigitated like some other fissures. As the tonsil retracts superiorly, the cerebellomedullary fissure widens to expose the proximal tonsillomedullary segment of the PICA. Fig. 20.2 Three anatomical triangles defined by the lower cranial nerves as exposed by the far-lateral approach (inset): the vagoaccessory triangle; the suprahypoglossal triangle (SHT); and the infrahypoglossal triangle (IHT). These triangles clarify the dissection routes through the lower cranial nerves to PICA aneurysms. The PICA-VA convergence is obstructed by the lower cranial nerves, and the dissection pathway to the aneurysm traverses this neural lattice. Three anatomic triangles clarify the dissection routes: the vagoaccessory triangle, the suprahypoglossal triangle, and the infrahypoglossal triangle (Fig. 20.2). The vagoaccessory triangle is defined by the vagus nerve superiorly, the accessory nerve laterally, and the medulla medially. This triangle is the natural working window of the far-lateral approach. The accessory nerve lies along the skull base and prevents dissection anterolateral to the nerve; vagus and glossopharyngeal nerve rootlets fan out from the retro-olivary sulcus to prevent dissection superiorly, and most PICA aneurysms do not extend above this nerve complex. CN9, CN10, and CN11 originate from the retro-olivary sulcus and course to the jugular foramen, whereas CN12 originates from the preolivary sulcus and courses to the hypoglossal foramen. Consequently, the course and depth of the hypoglossal nerve differs from that of the vagus and accessory nerves. The vagoaccessory triangle is divided into two smaller triangles by the hypoglossal nerve as it traverses laterally. The suprahypoglossal triangle is the area in the vagoaccessory triangle above the hypoglossal nerve, between CN10, CN11, and CN12. The infrahypoglossal triangle is the area in the vagoaccessory triangle below the hypoglossal nerve, between CN11, CN12, and the medulla. Fig. 20.3 PICA aneurysms reside in different anatomic triangles depending on variations in PICA anatomy, VA tortuosity, and aneurysm pathology. (A) PICA aneurysms can lie in the suprahypoglossal triangle (aneurysm A), with hypoglossal nerve rootlets in the axilla of the PICA. (B) PICA aneurysms can lie directly under the hypoglossal nerve at the border between the supra- and infrahypoglossal triangles (aneurysm B), with hypoglossal nerve rootlets both in the axilla and over the shoulder of the PICA. (C) PICA aneurysms can lie in the infrahypoglossal triangle (aneurysm C), with hypoglossal nerve rootlets between the distal aneurysm neck and the VA. (D) PICA aneurysms can lie outside the vagoaccessory triangle (aneurysm D), separate from the lower cranial nerves. These triangles through two layers of nerve roots are opened to reach the PICA-VA confluence. Variability in arterial anatomy, tortuosity, and aneurysm pathology makes the route different with each case (Fig. 20.3). For example, a proximal PICA origin positions the aneurysm inferolaterally in the vagoaccessory triangle, and the route to the aneurysm is through the infrahypoglossal triangle. A distal PICA origin positions the aneurysm superomedially, and the route to the aneurysm is through the suprahypoglossal triangle. The dissection beyond the retro-olivary sulcus follows the PICA’s lateral medullary segment around the olive to the preolivary sulcus and hypoglossal nerve rootlets. These rootlets drape the VA perpendicular to the artery’s axis like the rungs of a ladder. They are easy to work through, but can settle in the aneurysm’s cleavage planes: in the axilla of the PICA as it originates from the VA, over the shoulder of the PICA against the proximal neck, or in the crotch between the distal neck and the distal VA. Dissection beyond the preolivary sulcus through the hypoglossal nerves follows the anterior medullary segment and arrives at the PICA-VA confluence with aneurysms deep in the suprahypoglossal triangle. Posterior inferior cerebellar artery anatomy is highly variable, and can originate anywhere along the VA trunk and in some cases even extradurally. The PICA originating inferiorly may be lateral to the medulla and not have an anterior medullary segment. An elongated or tortuous VA can move a PICA aneurysm away from the lower cranial nerves. Some aneurysms displace and drape lower cranial nerves. Therefore, it is often more useful to apply the anatomic zones that define PICA segments to the aneurysm location instead (Fig. 20.4). Aneurysms that lie in the anterior medullary zone, where the anterior medullary segment would normally reside, require working through CN10, CN11, and CN12 to reach the PICA-VA convergence. Aneurysms that lie in the lateral medullary zone, where the lateral medullary segment would normally reside, require working through CN10 and CN11. Aneurysms that lie in the tonsillomedullary zone, in the cerebellomedullary fissure where the tonsillomedullary segment would normally reside, do not require traversing any nerves. Aneurysms in the tonsillomedullary zone have an early PICA origin or a distal PICA aneurysm. This survey clarifies aneurysm location relative to the medulla and helps in planning the dissection route.
 Microsurgical Anatomy
Microsurgical Anatomy
 Aneurysm Dissection Strategy
Aneurysm Dissection Strategy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree