Posterior Nonfusion Stabilization of the Degenerated Lumbar Spine with Cosmic
Archibald von Strempel
Dieter Moosmann
Christoph Stoos
Arno Martin
Introduction
The degeneration of the lumbar motion segment starts with a height loss of the disc caused by a water loss of the nucleus pulposus. The facet joints lose their congruence, which may cause a consecutive spondylarthritis (1). The fibers of the annulus fibrosus and the vertebral column ligaments lose tension so that a structural loosening occurs, complete with increased rotation instability (2,3,4). To compensate for the instability, a hypertrophy of the yellow ligament as well as the facet joints occurs very frequently, which may lead to a reduction of the surface of the cross-section of the central as well as lateral spinal canal. At the same time the motion segment may lose its original position, and scolioses, flat backs, rotations, and rotation slidings may develop. During the further course of the degeneration, lateral and front spondylophytes up to and including syndesmophytes may form, which in turn may lead to a spontaneous stiffening of the segment.
The complaints depend on the respective stage of the vertebral column degeneration.
In the first phase with a reduction of the height of the vertebral disc and loss of the congruence of the facet joints, chronically recurrent lumbalgies may occur that increase under load stress. When the stenosis of the spinal channel increases, additional symptoms may occur in one or both legs with the indications of a claudicatio spinalis. If a spontaneous ankylosis of the segment occurs before a symptomatic spinal channel stenosis occurs, the frequency and intensity of lumbalgies decrease.
Why Are Spondylodeses Carried Out in the Treatment of Degenerative Lumbar Vertebral Column Diseases?
Until recently, there were few alternatives to a standard spondylodesis. One important reason is that the surgery of the degenerative lumbar vertebral column is a relatively young chapter in spine surgery. The techniques of correction and fusion, so successful in scoliosis surgery, were transferred to this new area of spine surgery, ever increasing since the early 1980s. An essential task of the spondylodesis consists of protecting the implants used against failure (dislocation, breakage).
When Is a Correction Necessary?
In contrast to the treatment of an adolescent scoliosis, in which the correction of the deformity is also the objective of the treatment, there are not very many indications for the correction of the degenerative lumbar vertebral column that actually serve the direct objective of the operation with pain release and restoration of neurologic functions.
Positional deformities in the sagittal and frontal planes that in total do not lead to a loss of the body vertical plump line need not be corrected. This concerns most lateral deviations. Therefore, the correction of a degenerative lumbar scoliosis is only necessary in exceptional cases.
The reduction of the vertebral disc always leads also to a flattening of the lumbar vertebral column, which also does not need to be corrected as long as the patient assumes an upright well-balanced posture. True and degenerative olistheses at an adult age are mostly not progressive. Stabilization and decompression without correction lead to the objective of the treatment. Therefore, it is not meaningful to transfer the principles of scoliosis surgery noncritically to the surgery of the degenerative lumbar vertebral column.
When Is a Fusion Necessary?
Fusion is necessary when corrections (mostly in the sagittal plane) are necessary to treat pain.
When Will It Be Possible to Do Without a Fusion?
The precondition is a dynamic implant, which does not require the protection of a spondylodesis. It must be possible to achieve the treatment objective (pain release, restoration of the neurologic function) without correction. The stabilization does not need to include more than three segments.
The Cosmic Implant System
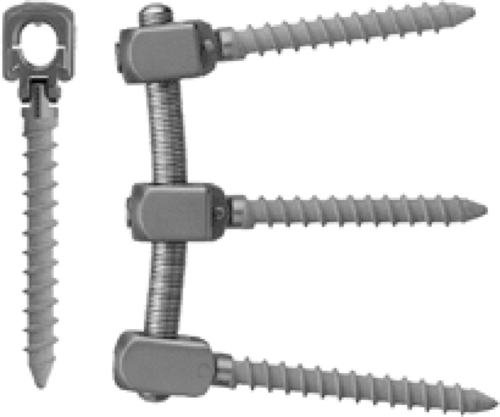
A posterior nonfusion implant system, which can do without protection by a spondylodesis, should not have any rigid characteristics. However, to be able to control instabilities effectively, the system must also feature stable characteristics. The cosmic system is a stable nonrigid implant. Stability is assured by the 6.25-mm rod, and nonrigidity is ensured by the hinged screw head. The screw features a hinged joint between head and threaded part, which causes the load to be shared between the implant system and the anterior vertebral column (Fig. 27.1). It was possible to show by means of laboratory tests that cosmic allows the same rotation stability as a healthy motion segment (5). In a cyclic loading test with 0.3 to 3.0 KN/1 Hz, we did not find an implant breakage or any debris after 10 million cycles (6). Because cosmic is used like a stability endoprosthesis, the bone healing of the pedicle screws is of major importance here. For this reason, the threaded part of the screw is coated with bonit. Bonit is the second generation of
bioactive calcium phosphate coatings on implants. In 1995, it was originally used for the first time in oral surgery for dental implants (7). In the area of vertebral column surgery, there exists a study on the use of a first-generation of bioactive calcium phosphate coating on Schanz screws. It was found that there was a significantly improved fixation of the coated screws in comparison to the uncoated screws (8). Thus, the screw is introduced transpedicularly into the vertebral body, similar to an orthopædic endoprosthesis. To achieve a sufficient press-fit behavior, the pedicle is widened by drilling to 3.2 mm maximum but only along approximately 50% of the screw. The screw has a self-tapping thread so that the tapping instrument only needs to be used in cases of extremely hard spongiosa. To prevent any early loosening of the screw, the screw must not be manipulated in any major way. Before the rods are implanted, these must be prebent such that they can be connected without any problems to the screw heads.
bioactive calcium phosphate coatings on implants. In 1995, it was originally used for the first time in oral surgery for dental implants (7). In the area of vertebral column surgery, there exists a study on the use of a first-generation of bioactive calcium phosphate coating on Schanz screws. It was found that there was a significantly improved fixation of the coated screws in comparison to the uncoated screws (8). Thus, the screw is introduced transpedicularly into the vertebral body, similar to an orthopædic endoprosthesis. To achieve a sufficient press-fit behavior, the pedicle is widened by drilling to 3.2 mm maximum but only along approximately 50% of the screw. The screw has a self-tapping thread so that the tapping instrument only needs to be used in cases of extremely hard spongiosa. To prevent any early loosening of the screw, the screw must not be manipulated in any major way. Before the rods are implanted, these must be prebent such that they can be connected without any problems to the screw heads.
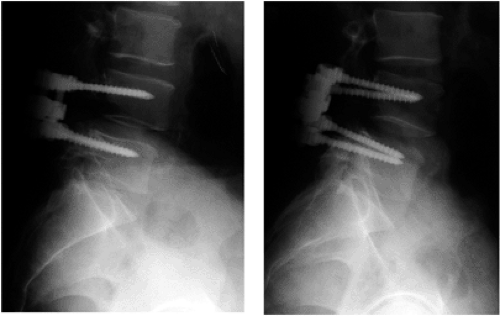
After the screw heads have been connected to the longitudinal rods, there remains only a micromobility in the hinges, which are placed close to the facet joints (Fig. 27.2). This micromotion and the shock absorber function of the preserved disc protect the adjacent levels.
Due to the good rotation stability, cosmic is not only used for purely discogenic pain conditions but also used together with a conventional laminectomy or even a facetectomy. A transverse stabilizer is only used for a monosegmental application in combination with a laminectomy. For two- or three-segmental applications, no transverse stabilizer is used.
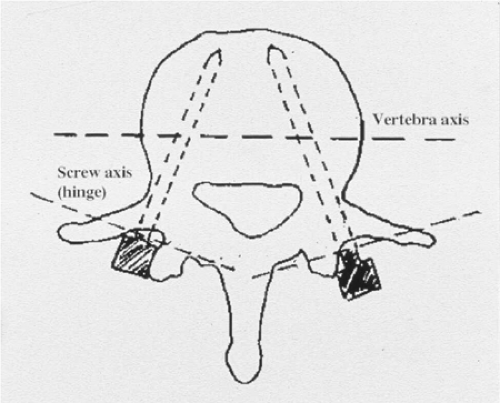
The implantation of the screws is affected either by means of a conventional midline approach with a point of entry lateral to the facet joint and an angle of approximately 15 degrees horizontal to the sagittal plane or by means of the more laterally situated Wiltse access with a somewhat ventrally located point of entry close to the base of the transverse continuations and an angle of 20 to 25 degrees horizontal to the sagittal plane (Fig. 27.3). A purely sagittal implantation direction is not recommended, as this will lead to a parallel positioning of the hinges and thus to an increased mobility in the sagittal plane.
Before the rod is implanted, the correct positioning of the patient will be checked again by means of lordosis that is as physiologic as possible. To avoid any early loosening, correction forces must not be applied to the screw.
Indications for Dynamic Stabilization with Cosmic
Symptomatic lumbar stenosis (claudicatio spinalis).
A stand-alone decompression of the spinal channel carries the risk of a reoccurrence of spinal narrowness, as the instability that led to the hypertrophy of the yellow ligament and the facet joints is not taken into consideration. In addition, lumbalgies and deformities may increase as an expression of the increased clinical instability. For this reason, we always carry out an additional stabilization with cosmic (Fig. 27.4A–C).
Chronically recurring lumbalgy in the case of discogenic pain and facet syndrome.
A degenerated disc disease is present if, in the magnetic resonance tomography (MRT), a vertebral disc dehydration with height loss and positive Modic signs is detected. If there are further changed vertebral discs (black disc), we carry out an additional discography. A positive memory pain confirms the suspicion of a symptomatic vertebral disc degeneration (9). In the case of a facet syndrome, we carry out a diagnostic local anesthesia under x-ray control, using 2-mL local anesthetic, respectively. If the pain subsides for some hours, the suspected diagnosis is confirmed. In such cases we carry out the cosmic stabilization using a paraspinous transmuscular approach according to Wiltse et al (10). (Figs. 27.5A–C and 27.6A–C).
Recurrent disc herniation.
In the case of a second recurrence of a disc herniation we carry out a stabilization with cosmic in addition to the nerve root decompression.
In combination with a spondylodesis.
Cosmic can also be used if, in addition to the nonfusion stabilization, there is an indication of a spondylodesis in one or two segments. For example, if there is a spondylolisthesis with a clear shift in the function x-rays and, in addition, in a further segment a symptomatic vertebral disc degeneration. In addition to the cosmic stabilization in situ, a posterolateral fusion is set up within the area of the spondylolisthesis. A laminectomy or facetectomy is carried out if there is an indication for this purpose.
Extension of an existing spondylodesis in the case of a painful adjacent level degeneration.
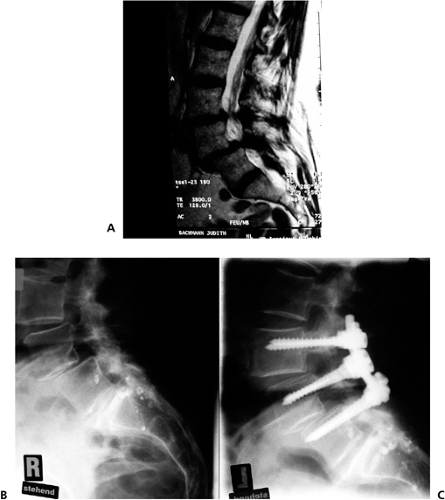
FIGURE 27.4 A–C: Spinal stenosis, pseudospondylolisthesis, decompression, and stabilization with cosmic.
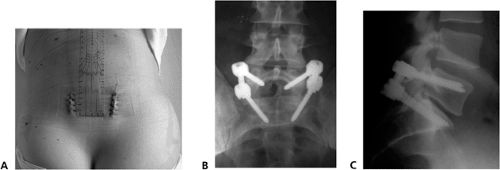
FIGURE 27.6 A–C: Paraspinal approach L5-S1, single-level stabilization anteroposterior and lateral view 2-years follow-up.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access