Chapter 3 Posterior Subscapular Approach to the Brachial Plexus
Patient Positioning
• The patient is initially placed in the lateral decubitus position and is then rolled into a prone position, bringing the operative side close to the edge of the operating table.
• Rolls are placed laterally under the anterolateral chest wall and transversely beneath both shoulders and the manubrium of the chest.
• The shoulder is abducted and the arm is flexed at the elbow. The arm and forearm are then secured to a padded Mayo stand adjacent to the operating table but at a level below it. The stand can be lowered or elevated to change the position of the scapula. The elbow, wrist, and hand are wrapped with protective pads (Figure 3-1).
• The operating table is then tilted up 15 to 20 degrees or into a reverse Trendelenburg position to allow further abduction of the shoulder and the scapula. The operating table can be raised or lowered to change the position of the scapula, as well as that of the head, the neck, and the rest of the shoulder.
• The contralateral arm is padded at the elbow and placed to the side.
• The head is usually turned partially toward the side of the dissection and placed on a well-padded donut or several folded sheets, with care taken to maintain the airway and to keep pressure off the orbits.
• Indications for this approach include tumors or injuries involving the nerve roots or proximal portion of the spinal nerves, especially the lower elements such as C7, C8, and T1.
Skin Incision
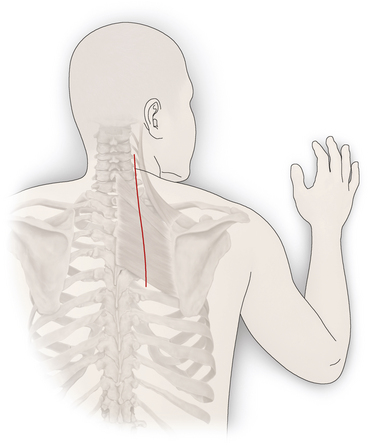
• A slightly curvilinear skin incision is made between the thoracic spinous processes and the medial edge of the scapula.
• The incision is curved around the medial edge of the scapula. It is usually placed halfway between the scapular edge and the thoracic spinous processes so that the midsection of the rhomboid muscles can be exposed.
• The incision extends to the posterolateral aspect of the lower neck. This placement tends to protect the spinal branch of the accessory nerve and the ascending branch of the transverse cervical artery, which course close to the medial border of the scapula.
Division of the Trapezius
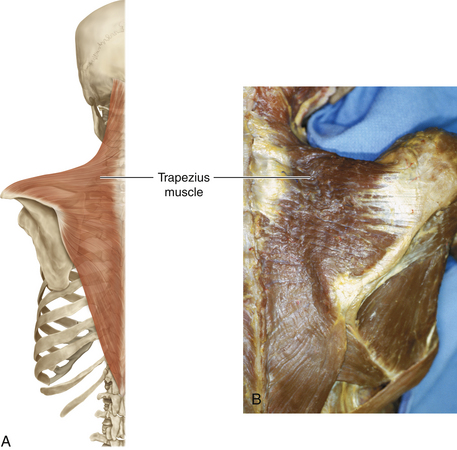
• The inferior spinal portion of the trapezius muscle is divided along the entire length of the skin incision, halfway between the medial edge of the scapula and the spine. The edges are marked at intervals with suture for later approximation (Figure 3-2).
• A large Kelly clamp is used to dissect beneath the trapezius midway between the scapula and the spine. Segments of muscle are clamped and sectioned between two Kelly or Sarot clamps, beginning inferiorly and proceeding superiorly.
Relevant Anatomy
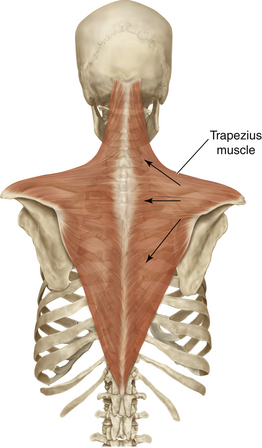
• The trapezius is a diamond-shaped muscle that arises in the midline, from the skull to the lower thorax, and converges on the outer part of the pectoral girdle. It is supplied by the spinal accessory nerve. The upper fibers of the trapezius elevate the scapula, the middle fibers retract, and the lower fibers depress the scapula and lower the shoulder. If the trapezius muscle is reflected laterally, the undersurface, where the spinal accessory nerve innervates, can be exposed (Figure 3-3).
• The superficial muscles of the back can be divided into two groups; the trapezius and latissimus dorsi muscles are the most superficial. Beneath the trapezius, the levator scapulae lies superiorly, the rhomboid minor somewhat medially, and the rhomboid muscle inferiorly. All three of these muscles insert on the medial border of the scapula (Figure 3-4).
• The trapezius muscle distribution is extensive. The diagram has arrows showing the direction of the forces that are brought to bear on the scapula as this large muscle contracts.
• The levator scapulae attaches between the superior angle of the scapula and the lateral extent of the spine. This muscle has to take the strain when the trapezius is paralyzed, and action of this muscle should not be misinterpreted as trapezius function.
• The rhomboids adduct the scapula. A proximal branch of the C5 spinal nerve, the dorsal scapular nerve, supplies both the levators scapulae and the rhomboids. Absence of these functions, in the presence of deltoid paralysis, denotes a very proximal C5 injury. The electromyographer should place the electrode with care, being certain that the recording is being made from the trapezius or rhomboid (deeper); otherwise, confusing information may be obtained.
• The triangular space, which transmits the scapular circumflex artery, is formed by the teres major below, the long head of the triceps laterally, and the subscapularis and teres minor above (Figure 3-5).
• The quadrangular space, which contains the axillary nerve and the posterior circumflex humeral artery, is surrounded by the teres major below, the subscapularis and teres minor above, the long head of the triceps medially, and the surgical neck of the humerus laterally (see Figure 3-5).
• The rhomboids minor and major arise from the ligamentum nuchae, spinous processes, and intervening supraspinous ligaments of C7 to T1 and T2 to T5, respectively. The levator scapulae, which arises from the posterior tubercles of the transverse processes of C1 to C4 vertebrae, appears in the floor of the posterior triangle. The dorsal scapular nerve supplies these muscles.
• When the trapezius and rhomboid major muscles are reflected, the deep muscle layer, which includes the semispinalis capitis, splenius capitis, spinalis thoracis, and longissimus thoracis, is exposed.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree