♦ Preoperative
Operative Planning
- Biopsy proven pathology
- Staging of disease
- Life expectancy dictates extent of the procedure, unless to prevent paraplegia
- Cardiac and medical clearance
- Pulmonary status
- What type of exposure will patient tolerate
- What level disease defines surgical options
- What type of exposure will patient tolerate
- Embolization
- Localization
- Preoperative placement of radiopaque localizing implant (such as Guglielmi detachable coils placed into costotransverse junction, metallic pin placed on transverse process [so it does not migrate])
- Make identification of level easier if there is no clear intraoperative localizer with intraoperative fluoro (such as isolated epidural disease in the mid-thoracic spine with no obvious local landmarks like a compression fracture, large unique osteophyte, etc.)
- Preoperative placement of radiopaque localizing implant (such as Guglielmi detachable coils placed into costotransverse junction, metallic pin placed on transverse process [so it does not migrate])
- Consideration of less invasive palliative treatments
- Vertebroplasty/kyphoplasty
- Radiation therapy alone or as stereotactic radiosurgery
- Pain stimulator
- Pain pump
- Vertebroplasty/kyphoplasty
- Computed tomography scan (bone windows)
- Magnetic resonance imaging
- Spine x-rays
Equipment
- Fluoro compatible table
- Fluoro unit
- Multiaxial reconstruction unit
- Exposure determines retractors
Operating Room Set-up
- Equipment
- Fluoro (Best: isocentric or O-arm [Medtronic] type unit that allows axial, sagittal, and coronal reconstructions)
- Spinal table (Best: Jackson or Allen [Allen Medical Systems, Acton, MA] type table that allows for fluoro through table rather than standard operating room table with central pedestal and bolsters)
- Minimally invasive set-up (if used) locked to opposite side as surgical side
- Anesthesia at head, nursing table at feet
- Fluoro (Best: isocentric or O-arm [Medtronic] type unit that allows axial, sagittal, and coronal reconstructions)
- Anesthetic issues
- Single lumen tube
- If monitoring motor evoked potentials, then recommend total intravenous anesthesia or minimal inhalational
- Small (1 mg/hr vecuronium if strong potentials)
- Large bore catheters
- Central line
- Introducer, if possible
- Not groin line unless for a-line
- Central line
- Multiple units packed red blood cells in operating room before start
- Be prepared for massive transfusion, including factor and even factor 7 transfusion
- No postoperative or intraoperative use of nonsteroidal anti-inflammatory drugs
- No blood recycling use (some use leukocyte filter, we do not trust it to remove all tumor prior to blood return)
- Antibiotics on board prior to incision
- Be prepared for massive transfusion, including factor and even factor 7 transfusion
- Single lumen tube
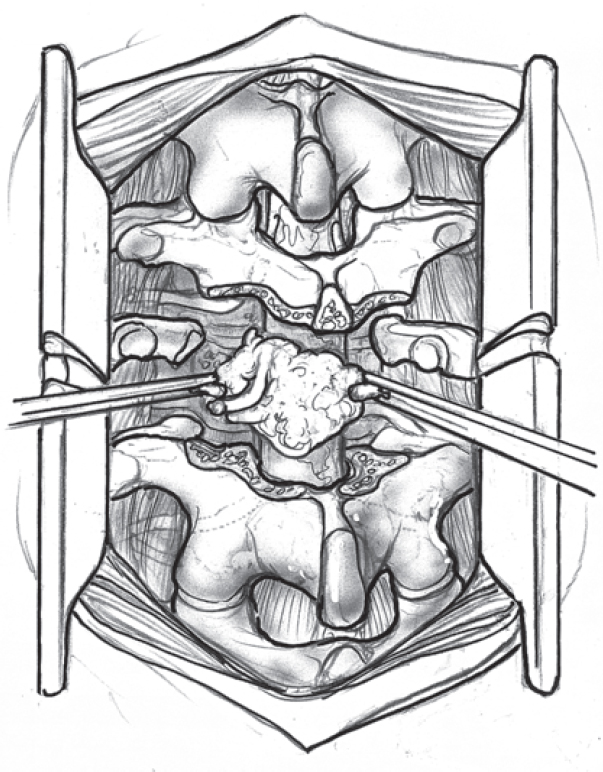
♦ Intraoperative (Fig. 128.1)
Positioning
- Prone
- All metallic artifact-generating wires out of fluoro field circumferentially
- Arms down at side (below the plane of the spine) if need to be operating above T6 (T5 and up) because of the need to get fluoro around shoulders and arms
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree