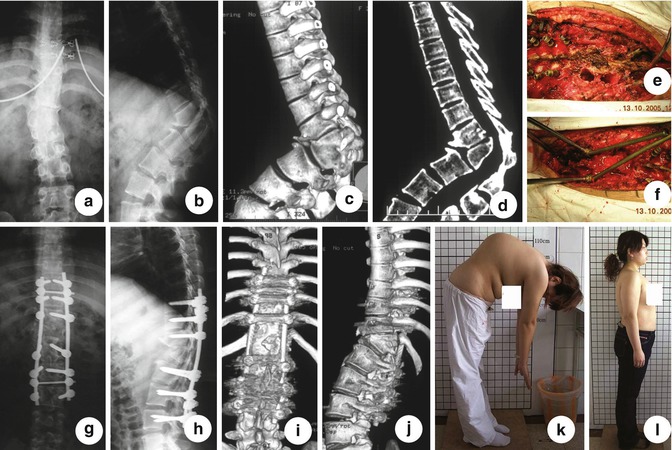
Fig. 10.1
Diagrams of VCR. (a) Pedicle screws were inserted before the osteotomy was performed; (b) A temporary rod was placed to bridge the anterior resection before beginning the posterior osteotomies to provide stability and reduce the chances of sudden spinal translation; (c) The anterior column was reconstructed with metal mesh filled with cracked bone after the osteotomy; (d) Realignment was achieved when the posterior column was closed (Reprint from Yan Wang and Lawrence G. Lenke [13])
Brediwell et al. [1, 2] recommended that the surgeon must answer the following critical questions when evaluating the patient. First, how much surgery is necessary to accomplish sufficient correction to warrant the intervention? Second, can the surgery be accomplished with reasonable risk, especially neurologic? Third, how much surgery can the often debilitated and deconditioned patient tolerate? Finally, will the patient’s quality of life be improved? In short, surgeons must know what we need to do and what we can do.
Theoretically, closing–opening technique, such as VCR, may be the suitable option for management of severe angle spinal deformity, because it can bring an adequate decompression and excellent balance of sagittal and coronal planes while shortening the length of the spinal column. However, the limitation of the VCR is obvious, such as, more unstable, more blood loss, more manipulation performed in cord territory, and greater risk of neurologic deficit [1].
Vertebral column decancellation (VCD) technique is a combination of several spinal surgery techniques, which is a technically demanding method (Fig. 10.2).
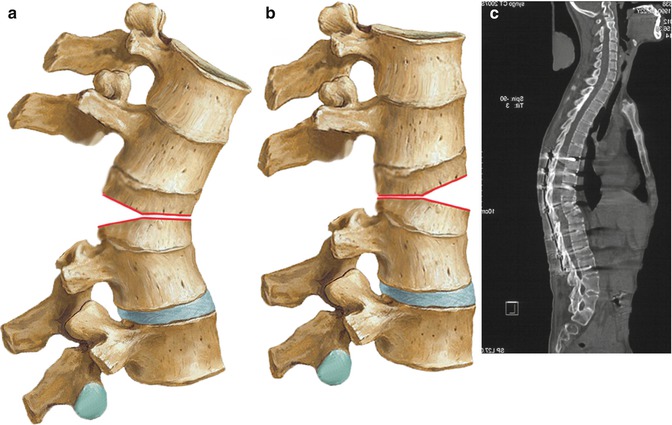
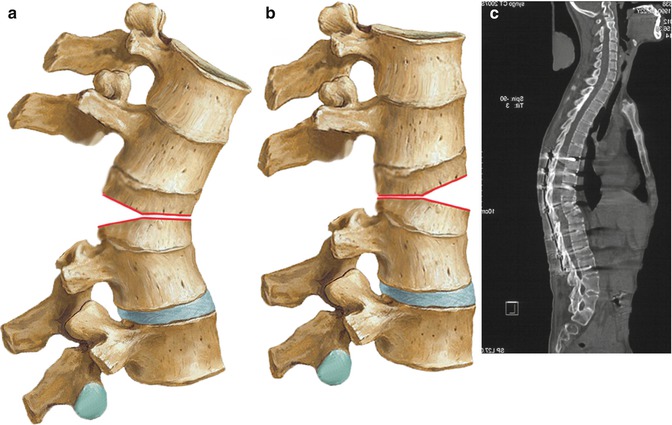
Fig. 10.2
Diagram of VCD. (a) The anterior and middle of vertebra was removed as less as possible to decrease the shortening of spinal cord. The osteotomy gap was removed like shape “Y” rather than “V”; (b) The hinge located at the middle column, the posterior column closes properly and the anterior column opens; (c) Intraoperative picture shows T12 VCD, The proper shortage of the posterior column (Reprint with permission from Wang et al. [14])
10.2 Principle of VCD
The goal of management of angular spinal deformity is to realign the spinal deformity and to decompress the neurological elements. The technique of VCD was based on the recognition of the following (1) the decancellation of deformed vertebrae may facilitate to realignment the angular spine; (2) the spine realignment may result in pain relief or other neurological deficits exception to the cosmetic problem; (3) the rational management of angular spinal deformity can be achieved by lengthening the anterior elements, shortening the posterior elements, or a combination of the two. The osteoclasis of anterior cortex of deformed vertebrae may help to open and elongate the anterior column, which may decrease the needed shorten of posterior column, and then decrease the risk of neurological deficits; (4) the residual bone of deformed vertebrae may take the place of metal mesh described in the VCR technique, served as a “bony cage”, which may bring a better stability instantly and better fusion in foreseeable futures; (5) the manipulation order was from inside to outside (using eggshell technique) rather than from outside to inside, which means it is not necessary to manage the segmental vessel in most cases, and then less vascular complication may be expectable; and (6) VCD is a closing–opening technique and the hinge of correction is adjustable, which is identified to previous closing wedge osteotomy (CWO). The hinge in CWO technique is positioned at the anterior longitudinal ligament at the apex of the deformity. It may become curved or kinked or potentially damaged, if the spinal cord was shortened too long for the correction. Theoretically, the retraler the hinge locate, the shorter the needed shortening of spinal cord is, and the safer the correction.
10.3 Indications for VCD
There are two main curve types in angular spinal deformities: sharp angular and round angular deformity. In patients with Pott’s deformity, the curve type is usually kyphosis deformity. For sharp angular kyphotic deformity, the lever arm of the center of the gravity line with respect to the wedged vertebra may increase [13], this changes lead to the anterior elements of the spine fail under compression and posterior elements fail under tension, then, results in an increase in the eccentric loads and increased wedging and deformity, and pain appears, and neurologic deficit may develop or increase. Therefore, sufficient restoration of alignment may obtain not only better fusion but also decompression. Patients with sharp angular kyphoscoliosis also face the same conditions, and spinal osteotomy also is an option to warrant the intervention.
10.4 Operative Technique
The surgical plan, including the resection site, instrumentation level, and degree of correction, was determined based on clinical radiographs, CT scans, 3-D reconstruction images, and MRI. All surgeries were monitored by intraoperative somatosensory-evoked potential system. In general, the younger the patients infected with TB, the better global sagittal balance the spine can achieve, because the upper and lower spine of the deformity can compensate the curve during the growth of spine. These changes also influence the selection of instrumentation level.
In sharp angular spinal deformity, a standard skin incision was made in the midline, and the subperiosteum dissection was performed to exposure the bony structures of the spine (Figs. 10.3 and 10.4). All pedicle screws were inserted with a free-hand pedicle screw placement technique. The multilevel vertebral column decancellation was begun with the probe of the pedicle of deformed vertebral body to be removed. Using C-arm fluoroscopy confirms the appropriate insertions for osteotomy plane. Then, a high-speed drill was used to enlarge the hole cephalically and caudally by until the corresponding walls were penetrated. An angular forceps or curette was used to remove the residual upper and lower cartilaginous end plates of the resected vertebra and intervertebral discs, then, using a Kerrison rongeur or drill to thin the anterior and lateral walls of the vertebral body, which were collapsed under pressure laterally to expose the posterior walls further. The posterior wall was resected with an angular forceps. In general, it is not necessary to remove the cancellous bone totally, and the residual bone was used to reconstruct a “bony cage” to take the place of metal mesh described in VCR techniques. After the vertebral bodies were decancellated, the posterior elements, including the spinous processes, laminae, facet joints, and transverse processes were removed. Osteoclasis of anterior cortex of vertebrae body was achieved by forceful manual extension of upper body and the lumbar spine to close the posterior wedge osteotomies and to disrupt the anterior longitudinal ligament, creating an anterior monosegmental intervertebral opening wedge with elongation of the anterior column. The hinge of the correction was located at the borderline of anterior and medial column. If the correction was not adequate, retroposition of hinge was performed. Autogenous bone can then be placed at the gap of osteotomy site, if the cavity was too large to contact the two osteotomy plane, with the expectation of better bony fusion and better stability. After the confirmation of correction on fluoroscopy, the final internal fixation was applied.