Fig. 9.1
(a–d) Patient is a 54 + 8-year-old female, previously treated with radiotherapy for spinal cord neuroblastoma as a child, with severe collapsing lumbar kyphoscoliosis. (a) Upright and (b) supine anteroposterior and lateral (c, d) radiographs demonstrated a 67° lumbar curve with 94° of kyphosis
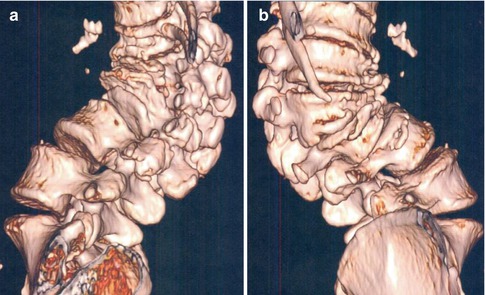
Fig. 9.2
(a, b) 3D CT reconstructions illustrate the severity of the deformity
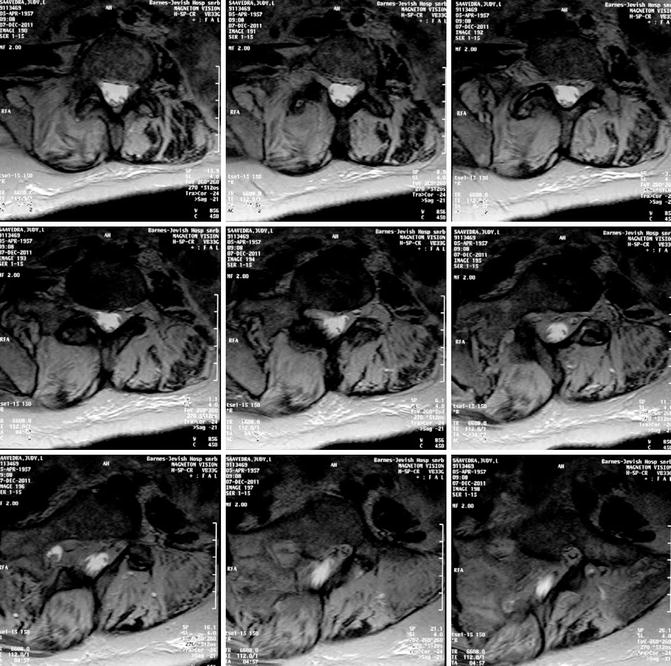
Fig. 9.3
Preoperative MRI axial images demonstrating significance of the bony deformity as well as compression of the lumbar neural elements

Fig. 9.4
(a–d) Preoperative (a, c) and postoperative (b, d) clinical photographs demonstrating significant correction in both coronal and sagittal planes

Fig. 9.5
(a–d) Preoperative (a, c) and postoperative (b, d) clinical photographs demonstrating implant fixation through zone of VCR, as well as significant correction in both coronal and sagittal planes
Because many of these patients with longstanding or severe deformities have poor functional capacity, preoperative optimization of all medical comorbidities and other parameters is strongly encouraged. For pediatric patients, halo traction prior to surgery allows gradual and safe elongation of the spinal column and neural axis. Presurgical hospitalization also provides opportunities for the patient to receive appropriate nutritional support, exercise, and physical therapy, as well as daily respiratory therapy. Structured ambulation programs can maximize pulmonary and cardiac capacity. Patients with severe nutritional deficiencies can receive enteral or parenteral nutrition and preliminary gastrostomy tubes or central venous access can be placed if necessary. All of these modalities can, in theory, reduce the morbidity associated with the surgery that will correct their structural deformity.
9.3 Surgical Considerations
The surgical techniques employed during a posterior VCR are technically demanding. Prior experience with cadaver training, as well as visitation with a surgeon well versed in performing the procedure are both strongly encouraged before attempting this type of operation. The operating surgeon should also have a baseline comfort level with posterior three-column pedicle subtraction osteotomies in the thoracolumbar and lumbar regions, performing posterior thoracic and lumbar hemivertebra resection, costotransversectomies for the treatment of spinal tumor, trauma and infection, and a comfort level with handling the dural sac—including removing adhesions, fibrous tissue, or epidural fat over multiple levels of the dura. There is no pretense that performing this type of complicated spinal deformity surgery is without significant risk to the patient and the learning curve for the surgeon is steep.
Intubation is often very difficult in patients with cervicothoracic deformities and thorough preoperative evaluation by the anesthetic team is mandatory as fiberoptic intubation may be required. Many of these patients’ spinal cords are at risk, secondary to chronic myelopathy or to ligation of segmental vessels after previous surgery, so optimizing spinal cord blood supply is imperative. It is therefore recommended that a normotensive blood pressure with mean arterial pressure (MAP) of approximately 70–80 mmHg be maintained. When treating severe angular kyphosis, we often request that the MAP be maintained at a minimum of 80 mmHg during the entire procedure and higher during the most critical portions of the VCR. During actual closure of the resected area, a mean pressure of >80 mmHg is preferred for all patients. It is also extremely important that the anesthesia team remain acutely aware of the likelihood for significant blood loss during the procedure, and it is recommended that various antifibrinolytics be utilized to aid in decreasing overall operative loss. We currently use Tranexamic Acid at a 100 mg/kg loading dose and 10 mg/kg maintenance dose, which anecdotally decreases blood loss 25–50 % intraoperatively [16].
9.3.1 Spinal Cord Monitoring
Sensory and motor tract monitoring should be provided throughout the duration of these neurologically high-risk surgeries and the spinal cord monitoring team must be attentive during all stages of the procedure. Intraoperatively, we typically utilize somatosensory-evoked potentials (SSEP) and either transcranial motor-evoked potentials (TC-MEP) or neurogenic mixed evoked potentials (NMEP). Spinal motor conduction can be evaluated quickly and accurately by transcranial motor-evoked potentials [17]. Upper extremity SSEPs are utilized to prevent brachial plexopathies. Electromyography (EMG) used in a spontaneous elicited fashion (primarily for procedures involving the lumbar spine) also provides helpful information to monitor the lumbar nerve roots. Normally, we also use stimulus triggered EMGs of pedicle screws in the thoracic spine from T6-T12 and the entire lumbar spine to S1 to evaluate for any violation of the pedicle wall into the canal.
Our experience has suggested that approximately 10–15 % of these procedures will have neuromonitoring changes requiring surgical adjustment [10, 15]. In those patients with previously treated intraspinal anomalies, such as tethered cord or intraspinal tumors—or even in patients with a coexistent condition such as Charcot–Marie–Tooth disease—intraoperative monitoring will be unobtainable. Frequent wake-up tests will be necessary to confirm neural integrity during all aspects of the procedure when monitoring is not feasible. Despite this, it is known that patients with unobtainable intraoperative data will have a higher risk of neurologic deficits following treatment of severe spinal deformity [14]. Surgeons must recognize this higher neurologic risk and if spinal cord monitoring is unobtainable or cannot be maintained, performing an alternative deformity correction procedure may be indicated.
9.4 Surgical Technique
The posterior-only approach of this VCR technique necessitates prone positioning of the patient on a standard radiolucent orthopedic table. Depending on the size of the patient and the nature of the deformity, it is our preference to place a halo or Gardner-Wells tongs with traction in the operating room. Doing so allows the skull to be anchored while the face and eyes remain free, but it is important that excessive traction be avoided in patients with severe kyphotic deformities. By keeping the abdomen free and the arms abducted and externally rotated and well padded, occurrence of various skin injuries, brachial plexopathies, and peripheral neuropathies can be minimized. While proper positioning of patients with severe deformities can be time-consuming, it is extremely important for patient safety.
A thorough subperiosteal dissection of the exposed posterior vertebral column is performed. Each transverse process is exposed from the most superior level involved in the instrumentation and fusion to the most distal vertebra. In some cases, exposure of the sacrum and/or ilium may be required. At the apex of the thoracic deformity, it is not uncommon to perform convex medial rib thoracoplasties to gain adequate exposure of the convex transverse processes. Proper identification of spinal levels with intraoperative radiographs is obtained. Typically, the resection procedure will be performed at the apex of the deformity.
Following exposure and appropriate level identification, multilevel posterior column osteotomies (Ponté or Smith-Petersen type) are performed around the apex of the deformity. Individual notching and removal of 3–4 mm of the inferior facet at every level is performed, and the ligamentum flavum is excised and the proximal portion of the superior articular facet is removed above the pedicle within the foramen over the levels to be osteotomized. In performing multilevel posterior column osteotomies, the flexibility of the periapical region is increased, thereby allowing for more harmonious correction once the resection is complete. This maneuver also makes periapical pedicle screw placement safer; since these vertebrae are often severely deformed exposing the spinal canal following the osteotomy allows palpation of the medial border of the pedicle and prevents potentially catastrophic intracanal placement of the concave screws. The only condition under which we will place pedicle screws prior to performing the osteotomies is in patients with severe angular kyphosis; because there is a risk of sagging of the spinal column and subsequent ventral pinching of the spinal cord, we prefer to gain pedicle screw access and place temporary stabilizing rods prior to any posterior column destabilization. Once obtained, we proceed with the osteotomies.
The efficient and safe placement of pedicle screws is a critical component and typically proceeds from distal to proximal. We prefer segmental fixation with many periapical screws placed to provide stability near the planned resection site. We utilize the free-hand technique of anatomical landmarks and a blunt gearshift to place screws. In patients with a prior fusion mass at the apex of their deformity, we never attempt apical concave screw placement without having prior access to the spinal canal and medial pedicle border through a laminectomy or laminotomy at the apex. We will place convex thoracic periapical screws in fusion masses as the spinal cord is usually quite a distance from the convex pedicle site. Depending on surgeon preference and experience level, fluoroscopic and image guidance techniques may be utilized for safe and efficacious screw placement. The majority of screws utilized will be multiaxial screws or multiaxial reduction screws (MARS). We strongly recommend the use of MARS at the immediately adjacent levels of the resection site, as these screws allow efficient placement of temporary rods around the apex and the ends of kyphotic deformities and can aid in reducing any subluxations that may occur. Once all screws have been placed, intraoperative radiographs are obtained in the anteroposterior and lateral planes to document accurate screw placement. Electromyography (EMG) is performed for all screws placed from T6 caudal to S1. In ambulatory patients fused to the sacrum and ilium, adjunctive transforaminal lumbar interbody fusion (TLIF) may be performed for anterior structural support and fusion of the lumbosacral disc.
At the level of the thoracic vertebra to be resected, we begin by performing a costotransversectomy bilaterally. Five centimeters of the associated medial rib is removed prior to the laminectomy, which avoids inadvertent canal intrusion. This maneuver is achieved using circumferential, subperiosteal dissection of the rib utilizing electrocautery. Ideally, rib head removal is performed with the entirety of the associated rib, but occasionally a portion of the rib head will remain attached to the lateral portion of the vertebra. These ribs are kept whole and not morcellized, as they will be used to cover the laminectomy defect at the end of the procedure and provide structural bone graft to the area. A complete laminectomy is then performed from the inferior pole of the pedicles above the resection to the superior pole of the pedicles of the level below the resection. In a characteristic adolescent or adult patient undergoing a single-level resection, this action will result in approximately a 5-cm laminectomy defect. The entire dural sac is identified through this exposure and freed of any fibrous tissue, adhesions, or epidural fat. At this point, the thoracic nerve root on the convex side of the apical vertebra to be resected is typically ligated. Although not absolutely necessary, doing so makes the remainder of the vertebral resection easier. We recommend temporary clamping of the nerve root and continuous spinal cord monitoring (performed for 5–10 min) to verify that there is no diminution in spinal cord blood supply. If monitoring remains stable during clamping of the nerve root, the root is then double tied as medial to the dural sac as possible and transected. Anecdotally, we have found that ligation of multiple thoracic roots unilaterally has neither caused any neurologic compromise nor have we seen any sensory deficit to the chest wall—provided less than three or four roots are ligated. We attempt to save the concave roots and in the lumbar spine; the roots are obviously maintained.
A temporary stabilizing rod is attached to, at a minimum, two or three pedicle screws both above and below the resection area. Classically, a unilateral rod is used; however, in severe angular kyphotic or kyphoscoliotic deformities, bilateral rods are recommended to prevent subluxation of the spinal column. The pedicles to be resected are encircled and the vertebral body resection begins by gaining access to its cancellous bone through a lateral pedicle–body entrance. The cancellous bone of the vertebral body is curetted and all removed bone is saved for grafting. For a patient with pure scoliosis or kyphoscoliosis, the majority of the vertebral body will be removed from the convexity of the deformity. Indeed, resecting the apical concave pedicle can be quite challenging. The pedicle encountered during this step tends to be extremely cortical and often the entire dural sac rests on the medial concave pedicle. However, the pedicle on the concavity may not even have an associated ventral vertebral body, as it is often rotated laterally and dorsally on the convexity of the deformity. It is our preference to utilize a small, high-speed burr to carefully remove the cortical bone along the concavity of the deformity while carefully protecting the adjacent dural sac/spinal cord. By performing the concave resection of the pedicle prior to the convexity, bleeding into the dependent concave region is minimized. Doing so also allows the concave dural sac to drift medially, thereby reducing tension on the cord prior to completion of the corpectomy. Following subperiosteal exposure of the lateral portion of the vertebral body and placement of a malleable or customized “spoon” retractor to protect the adjacent vascular structures and viscera, the entire body is thus removed except for the anterior shell. Maintaining a thin rim of bone on the anterior longitudinal ligament (ALL), in theory, improves fusion. However, if the anterior bone is very dense, it must be thinned to allow easy closure of the resection area.
Discectomies above and below the corpectomy site are now performed. It is important that the end plates of the superior and inferior adjacent vertebral bodies are not violated, as placement of a structural intracorporeal cage may be required. Epidural bleeding must be controlled and hemostasis can be achieved through the judicious use of bipolar cauterization, topical hemostatic agents and cottonoids. Removal of the posterior vertebral body wall or floor of the spinal canal may then proceed. The dural sac must be circumferentially exposed and separated from the epidural venous complex, as well as from the posterior longitudinal ligament (PLL). The entire posterior vertebral wall may be removed with reverse-angled curettes, Kerrison rongeurs, Woodson elevators, or specialized posterior wall impactors. It is imperative that the ventral spinal cord is completely free of any bony prominences to avoid impingement during closure of the osteotomy. Osteophytosis of the adjacent disc levels may cause ventral compression and careful resection of any bony prominences at these levels must be performed.
The vertebral body resection is now complete. Closure of the resected area always begins with compression forces applied on the convexity, with initial shortening of the spinal column and convex compression as the main correcting vector. In primary cases with good bone stock, this technique is performed with individual pedicle screws. Alternatively, a construct-to-construct closure mechanism utilizing domino connectors at the apex of the resected area may be performed. This method distributes the forces of correction over several vertebral levels and functions in a stepwise fashion by closing the osteotomy from a construct rod above to a construct rod below. It is imperative to compress deliberately and monitor the dural sac as vertebral subluxation or dural impingement can occur during this step of the operation. If the patient’s deformity has any degree of kyphosis, we often place an anterior structural cage to prevent over-shortening of the deformity. This cage also acts as a hinge to provide further kyphosis correction. We also prefer to place an intervertebral cage for all posterior VCR procedures to provide shear force stabilization by the interdigitation of the tines of the cage into the end plates above and below and to procure an anterior fusion as well. Once the closure has been completed and appropriate correction maneuvers performed, a permanent contralateral rod is placed. The temporary closing rod is removed and a permanent, final rod is placed on the ipsilateral side. Appropriate compression and distraction forces, in situ contouring, and other correction techniques may be performed. Careful and repetitive palpation of the dural sac circumferentially is performed at every iterative step of the correction to confirm that it is free and not under undo tension.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








