Fig. 50.1
AP c-arm image. Note operative L4–L5 operative disc endplates are not parallel to X-ray beam
4.
Trendelenburg bed so that operative disc is perpendicular to floor. L5–S1 and L4–L5 typically require reverse trendelenburg to raise head of bed. This allows tube to be placed more perpendicular to floor for better ergonomics (Fig. 50.2).
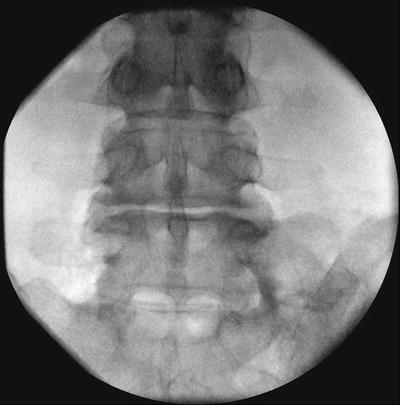
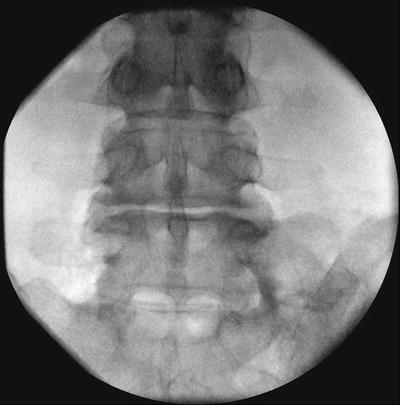
Fig. 50.2
Reverse Trendelenburg makes L4–L5 operative disc endplates parallel to X-ray beam and perpendicular to floor. Therefore, operative tube will be perpendicular to floor for better ergonomics
5.
Use oblique X-ray to determine skin incision. Typical angles: L2–L3 = 15°, L3–L4 = 20°, L4–L5 = 25°, and L5–S1 = 30°. The iliac crest will often limit the severity of the angle for approach to L5–S1. This is visualized on the oblique X-ray. Take off the degree of obliqueness until the crest moves laterally allowing access to the facet joint at L5–S1. Using the oblique X-ray for skin incision adjusts for the varying thickness of patients and the position of the disc and neural sac in relation to the pars.
6.
Mark a line on the skin that is just lateral to the pars interarticularis of the operative level.
7.
Mark a line bisecting this line at the caudal edge of the cephalad pedicle and the cephalad edge of the caudal pedicle. This delineates the skin incision (approximately 2 cm) (Fig. 50.3).
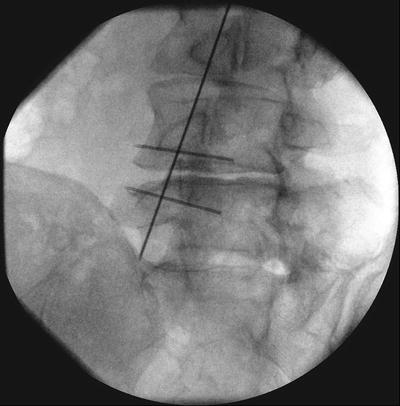
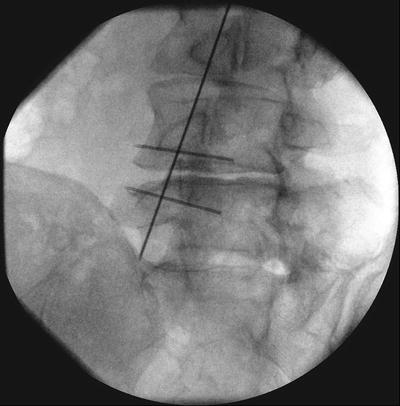
Fig. 50.3
Oblique c-arm image with vertical skin mark just lateral to the L4 pars and horizontal mark at edges of L4 and L5 pedicles for approach to the left L4–L5 foramen. Note, if surgery to be done at L5–S1, work in the triangle between the iliac crest, L5 transverse process, and L5–S1 facet joint
8.
Incise skin. Inject with marcaine and epinephrine.
9.
Incise fascia at same angle as oblique X-ray with 11 blade scapel. Insert first tubular dilator. (If patient is too obese for scalpel to reach fascia, may use blunt tip k-wire to penetrate fascia in line with oblique X-ray. Use oblique X-ray to guide k-wire down to pars, ensuring that it is not passed lateral and deep to pars and into foramen. Insert first tubular dilator over k-wire and remove k-wire.)
10.
Palpate junction of pars interarticularis with base of superior facet and transverse process.
11.
Sequentially dilate over trocar to accommodate 18 mm tube.
12.
Check oblique image to confirm position (Fig. 50.4). If any doubts, check lateral X-ray for depth.
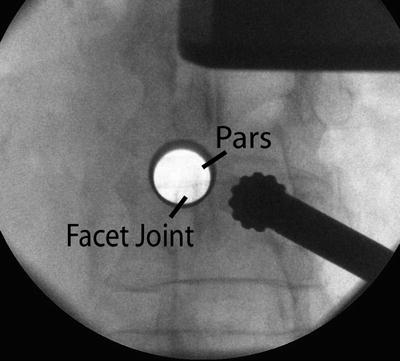
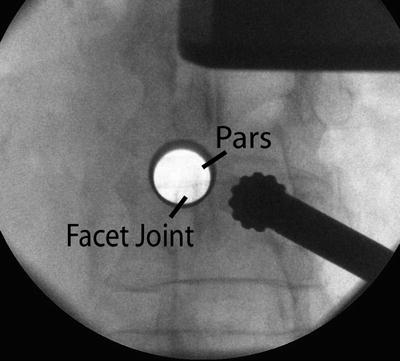
Fig. 50.4
Ideal position of tube: operative disc in caudal/lateral quadrant, facet joint in medial/caudal quadrant, transverse process in cephalad/lateral quadrant, and pars interarticularis in cephalad/medial quadrant
13.
Secure 18 mm tube to table clamp.
14.
Bring in microscope.
15.




Remove soft tissue in the tube with suction in one hand and electrocautery in the other hand. Use a pituitary rongeur to remove remaining soft tissue.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








